CHAPTER 74 Zenker’s Diverticulum
Esophageal diverticula are classified on the basis of anatomic location (pharyngoesophageal, midesophageal, or epiphrenic) and mechanism of origin (pulsion or traction). Traction diverticula are a result of pulling forces external to the esophagus that are secondary to inflammatory or neoplastic processes and usually occur on the anterior wall of the esophagus near the bifurcation of the trachea. In contrast, pulsion diverticula are a result of herniation of esophageal mucosa and submucosa through an area of weakened esophageal musculature. Of the various types of esophageal diverticula, Zenker’s diverticulum (ZD), a pulsion-type diverticulum, is one of the most common symptomatic esophageal diverticula, with an annual incidence of 2 per 100,000 people per year, with men being affected 2 to 3 times more commonly than women.1–6 For patients referred for an examination of the upper gastrointestinal tract, the incidence can reach 1 in 1000.4,6,7 ZD is extremely rare in Asia and Africa, where gastroesophageal reflux disease is also uncommon, suggesting that reflux may play a role in its etiology.5,7,8 Most esophageal diverticula are acquired lesions found in adults, particularly in the seventh and eighth decades. Pediatric hypopharyngeal diverticula along with true ZD are extremely rare, with most cases being congenital in nature and fatal secondary to massive aspiration pneumonia.9–19
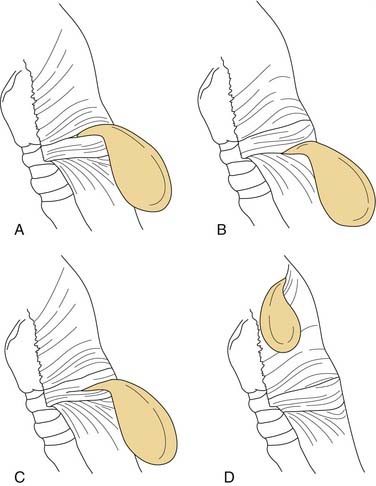
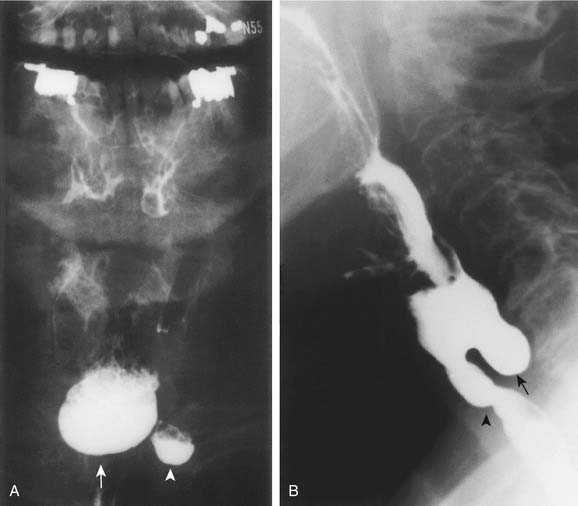
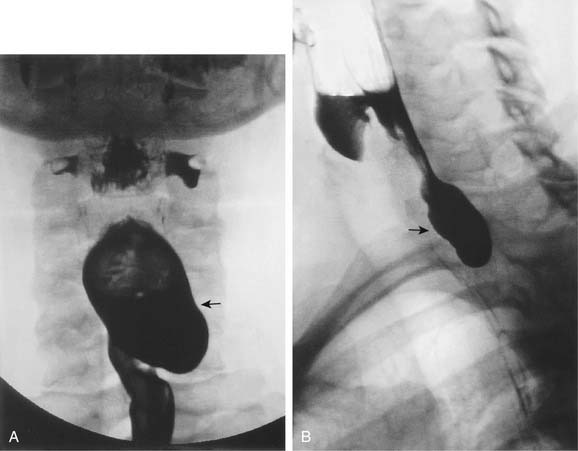
Zenker’s diverticulum is classically defined as a pulsion diverticulum between the cricopharyngeal muscle and inferior constrictor muscle in an area of weakness called Killian’s dehiscence or triangle, first described by Killian20 in 1907 (Fig. 74-1). However, there are other areas of weakness where pulsion diverticula may form, including Killian-Jamieson’s area, between the oblique and transverse fibers of the cricopharyngeal muscle, and Laimer’s triangle, formed between the cricopharyngeal muscle and the most superior esophageal wall circular muscles (Fig. 74-2).21 More rarely, pharyngoceles may be found in the posterolateral or lateral areas of the pharynx and hypopharynx (Fig. 74-3).22 Cases of double pharyngeal pouches have also been described (Fig. 74-4).23 Interestingly, ZD is found almost exclusively in humans, a fact hypothesized to be secondary to the large size and relatively caudal cervical location of the larynx in comparison with lower animals.8,21 The caudal location of the larynx results in an oblique orientation of the pharyngeal constrictor muscles, resulting in regions of weakness. Such muscular vulnerabilities are absent in animals because the pharyngeal and esophageal musculatures have a coherent parallel orientation throughout the upper aerodigestive tract. Indeed, ZD has been found in only one animal, the Mangabay monkey, in a single case so far.21
Theoretically, a diverticulum herniates to the side of less resistance. Accordingly, it is hypothesized that ZD is more prone to herniate to the left because the carotid artery is more laterally located on this side of the neck, making it less adherent to the adjacent prevertebral fascia, and because there the cervical esophagus has a slight convexity to the left.21,24 According to one series, although two thirds of Zenker’s diverticula are found in the midline, nearly 25% protruded to the left, and only 10% to the right.25,26
Presentation
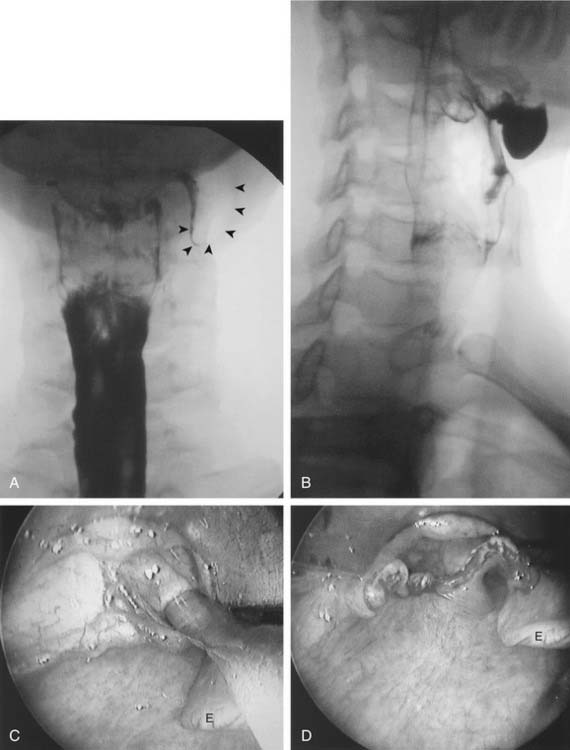
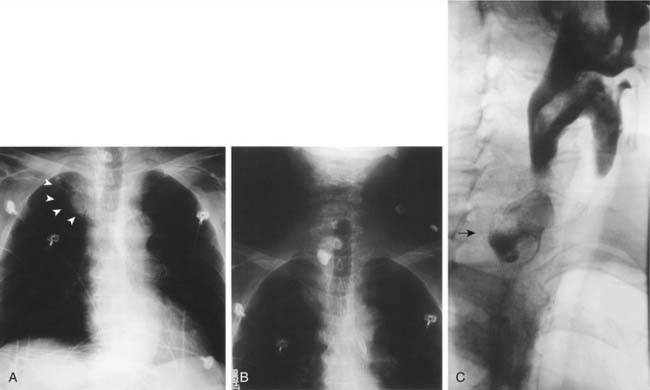
Patient history alone may raise suspicion for ZD. The predominant symptom is progressive dysphagia, which may occur in excess of 90% of patients presenting with the disorder.27 Regurgitation of food even hours after a meal, unprovoked aspiration, and noisy deglutition (borborygmi) specifically suggest ZD. Other symptoms are belching, hypopharyngeal mucus collection, halitosis, choking, coughing, hoarseness, globus pharyngeus, weight loss, and recurrent respiratory infections. Symptoms may last for weeks to many years before diagnosis and are generally more severe with a larger ZD. Minimal physical findings may include mucus pooling in the hypopharynx that initially clears with swallowing then recurs, emaciation or dehydration, and, only rarely, Boyce’s sign, a swelling in the neck that gurgles on palpation.28 However, it is more often the case that patients are without any specific findings on physical examination. Diagnosis is confirmed by barium swallow radiography, which can also define the size and position of the sac (Fig. 74-5). Fiberoptic endoscopy is also performed to help rule out other potential causes of dysphagia (Table 74-1). Occasionally, ZD may be first discovered during esophagogastroduodenoscopy or rigid cervical esophagoscopy as an incidental finding during the course of a gastrointestinal evaluation. The size of the sac may range from less than 1 cm to a truly enormous 12 cm or more. Rarely, a large diverticulum may be seen on a regular chest radiograph (Fig. 74-6).
Table 74-1 Differential Diagnosis of Dysphagia
| Congenital or acquired | Esophageal stenosis, stricture, web |
| Extrinsic compression from neck mass | |
| Carcinoma | |
| Trauma or iatrogenic (prior surgery) | |
| Inflammatory or infectious masses | |
| Tumor | |
| Plummer-Vinson syndrome | |
| Esophageal diverticulum | |
| Motility disorders | Achalasia |
| Esophageal spasm | |
| Muscular incoordination | Myasthenia gravis |
| Muscular dystrophy | |
| Thyrotoxicosis | |
| Carcinomatosis | |
| Central neuropathic | Stroke |
| Bulbar palsy | |
| Trauma | |
| Peripheral neuropathic | Trauma |
| Neuritis | |
| Collagen-vascular disorders | |
| Idiopathic | Idiopathic |
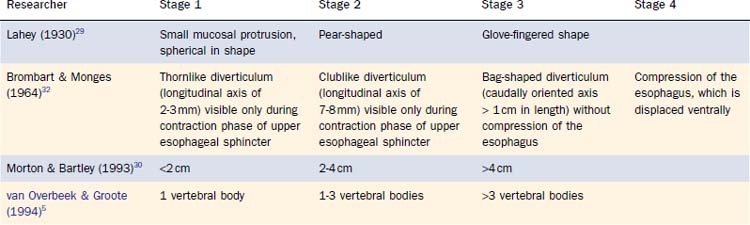
Through the years, physicians have attempted to classify ZD on the basis of contrast radiology findings (Table 74-2). In 1930, Lahey29 described three stages based on radiologic appearance. Morton and Bartley,30 along with subsequent writers, also described three stages but based them on size.31 van Overbeek and Groote5 used cervical vertebral bodies as a standard for comparison rather than absolute size measurements. Brombart and Monges32 expanded the classification into four stages, incorporating size, appearance, and stage of deglutition. Other workers have created increasingly more complex categories incorporating elements from both Brombart and Monges’s and van Overbeek and Groote’s systems.33 Although useful in terms of classifying ZD, these arrangements have limited clinical utility.
Pathophysiology
Although it is widely accepted that ZD is an acquired pulsion diverticulum, considerable controversy exists about the mechanism of its formation. Ludlow34 in Bristol, England, gave the first anatomic description of a pulsion diverticulum of the hypopharynx in 1769. He believed that this condition was induced in his subject by trauma after the swallowing of a cherry stone. Subsequent pathologists hypothesized traumatic rupture or burn, congenital upper esophageal stricture, thyroid goiter, or foreign bodies as triggers for ZD formation.21 It was not until 1877 that these hypotheses were rejected as erroneous and the basic pathophysiology was described by, and the diverticulum named after, Zenker, a German pathologist.35 The original German description was later translated into English in New York in 1878, allowing wider dissemination of Zenker’s findings.21 However, before Zenker, Bell36 (best known for describing facial nerve palsy) proposed in 1816 that incoordination of the inferior constrictor muscle against a closed cricopharyngeal muscle resulted in this type of outpouching at regions of inherent weakness. This etiology was later supported by other researchers.37–46 Similarly, the congenital theory describes an unusually weak or large Killian’s triangle from birth that with time herniates with normal pharyngeal contraction.47 Variations on this theme for the mechanism of formation of ZD have been debated ever since.
Patterson48 in 1919 first proposed cricopharyngeal achalasia as an etiology for ZD. Others noted a higher incidence of reflux and hiatal hernia in patients with ZD as well as epidemiologic observations that ZD occurs predominantly in populations with a high incidence of reflux, suggesting a possible relationship between the two.7,49 Several writers in the early 1970s suggested that spasm or persistently elevated resting tone of the cricopharyngeus secondary to reflux could cause ZD, although others refuted a direct causal association.7,49–51 On the basis of histologic studies, Lerut52 in 1988 proposed a structural abnormality of the cricopharyngeal muscle itself. Cook and associates53 in 1992 suggested partial, but incomplete, opening of the cricopharyngeal muscle because of fibroadipose tissue replacement as an etiology. Six years later, Walters and colleagues54 proposed that ZD might be a manifestation of central or peripheral neurologic disease. Regardless of the theory, the cricopharyngeal muscle is the common theoretical culprit behind the formation of ZD, and whether to address this muscle during surgical management has been debated through the years.55
Management
The treatment of ZD, as well as other forms of hypopharyngeal diverticula, is surgery. The presence of ZD is an additional risk factor in the overall health of the elderly patient, who may have concomitant pulmonary, cardiac, and other morbidities. With symptomatic ZD, the patient may have persistent aspiration causing deterioration of pulmonary function. Furthermore, with severe symptoms of dysphagia and aspiration, patients with ZD often become cachectic and dehydrated because of fear or inability to eat or drink. Definitive surgical management is mandated in these patients to prevent continued pulmonary compromise and malnutrition. Generally, all operative procedures addressing esophageal diverticula should be performed with the use of general anesthesia and as elective operations before complications have occurred. However, surgery may become urgent once problems have arisen and a patient’s condition is unlikely to be optimized before definitive treatment. In these patients, it is also important to fully evaluate and treat for other etiologies of dysphagia to obtain maximal benefit from surgery (see Table 74-1). Surgery is not necessary if the patient is asymptomatic or if the diverticulum is causing the patient minimal, if any, problems, but the patient does require long-term monitoring.
External Techniques
History
A variety of open, external surgical approaches to treating ZD have been performed, with and without the inclusion of cricopharyngeal myotomy. The first-recorded, but unfortunately fatal, treatment was performed in Vienna in 1877 by Nicoladoni,56 who established a fistula to drain the sac, a procedure Bell36 first proposed in 1816. Zenker and von Ziemssen35 in 1877 recommended dilations of the esophageal inlet.21 Niehans58 unsuccessfully attempted ZD excision in 1884. This procedure, first suggested by Kluge in 1850, resulted in the death of his patient from hemorrhage from the superior thyroid artery.21,57 Wheeler,59 2 years later, successfully excised a diverticulum. Kocher60 in 1892 performed a diverticulectomy with primary closure. Girard61 in 1896 inverted the diverticulum, a procedure first described by Keyrat in 1866.21 Schmid62 in 1912 described the method of diverticulopexy, which was performed by Hill63 in 1917. Unfortunately, these procedures, which often necessitated multiple stages, were associated with high mortality, particularly before the discovery of antibiotics to help reduce the morbidity and mortality. With technical advances and the availability of antibiotics, one-stage procedures became standard.
Despite the numerous different theories on the formation of ZD, the vast majority point toward the cricopharyngeal muscle as the etiologic factor. It thus follows that performing a cricopharyngeal myotomy does have a logical role in the surgical management of ZD. Although Richardson64 in 1899 performed the first cricopharyngeal myotomy with good results, albeit accidentally, it was not until 1936 that Aubin65 proposed cricopharyngeal myotomy as a useful adjunct to surgical diverticulectomy. Instead of a myotomy, Lahey66 in 1946 recommended cricopharyngeal dilation. Beginning in the 1950s, performance of a myotomy became a planned component of the surgical treatment of ZD and, in some cases, the sole treatment.1,67 It is now commonly accepted that surgical treatment of ZD without a cricopharyngeal myotomy is associated with a high recurrence rate.39,55,57,68–71
Procedure
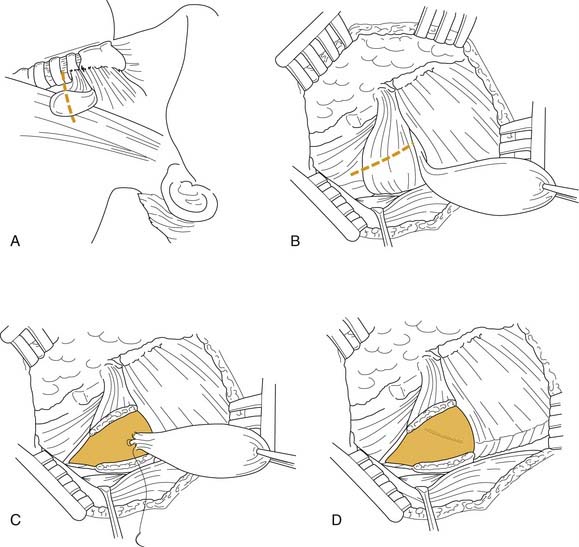
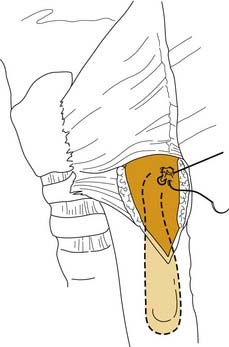
The standard incision is usually made along the anterior border of the sternocleidomastoid muscle from the level of the hyoid bone to several centimeters above the clavicle. However, a curvilinear transverse incision along a neck crease between the hyoid and clavicle is preferable for cosmesis (Fig. 74-7). Subplatysmal flaps are then raised, followed by lateral retraction of the sternocleidomastoid muscle. The fascial attachments along the anterior border are divided. The strap muscles may be retracted anteromedially, but for better exposure, the anterior belly of the omohyoid muscle may be divided inferiorly. As blunt dissection is carried out to expose the posterior aspect of the pharynx, larynx, and esophagus, the recurrent laryngeal nerve is identified and protected before the thyroid vessels are ligated and divided, if necessary. Once the diverticulum is identified and freed from the surrounding tissues down to its base attachment to the esophagus, a long cricopharyngeal myotomy is performed. The pouch itself can then be excised, inverted, or suspended by a suturing or stapling technique (Figs. 74-8 and 74-9).72–74 Each of these techniques has had its advocates.2,30,68,72,75–82 For small diverticula (1-2 cm), a cricopharyngeal myotomy alone may be sufficient.28,83,84 The patient generally is fed postoperatively through a feeding tube for several days, after which an oral diet may be resumed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree