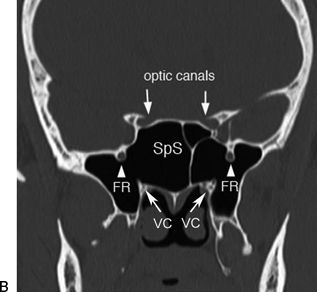
FIGURE 7.1 Radiologic examination of the lateral recess of the sphenoid sinus according to the degree of pneumatization. When the sphenoid sinus is not well pneumatized, (A) the lateral recess is a virtual space, and the vidian nerve and V2 are closely related. In the case of extensive pneumatization of the sphenoid sinus, (B) the lateral recess divides the above-mentioned nerves. (OC, optic canal; AC, internal carotid artery canal; VC, vidian canal; SpS, sphenoid sinus; PtP, pterygoid plate; FR, foramen rotundum.)
The traditional approaches to the sphenoid and its lateral recess (transantral, transpalatal, transfacial, and transcranial approaches) are considered invasive and disfiguring procedures. The development of intranasal endoscopic techniques offered a practical alternative to the traditional methods and direct access to the sphenoid sinus while preserving nearby anatomical structures. Endoscopic endonasal surgery of the middle and posterior cranial base is becoming increasingly refined, and the sphenoid sinus is considered the main anatomical landmark for a variety of approaches.
HISTORY
Isolated diseases of the sphenoid are rare according to the literature. Generally, there are no specific symptoms associated with sphenoid sinus disease. Nasal blockage and/or discharge, especially when unilateral, should always be investigated to exclude benign or malignant tumors with extension to the lateral recess of the sphenoid sinus, involving the pterygopalatine fossa or nasopharynx. Notably, when this symptom is associated with epistaxis in a young male patient, the possibility of juvenile nasopharyngeal angiofibroma (JNA) always has to be taken into account.
Headache is a general symptom that, in certain conditions or associated with other symptoms, can lead to the diagnosis of skull base disease. Often, this kind of headache is located at the vertex or retroorbital and does not respond to conventional treatments.
Watery unilateral nasal secretions could be a warning symptom, especially in a patient with previous episodes of meningitis. In this regard, female sex, postmenopausal age, and obesity are considered as risk factors for spontaneous cerebrospinal fluid (CSF) leaks associated with meningo-/encephaloceles. In these latter cases, the possibility of persistence of Sternberg canal has to be considered. In young patients with previous episodes of meningitis, it is mandatory to exclude a congenital malformation or syndrome even for patients who look phenotypically normal. Lesions of the maxillary or vidian nerves due to compression (fibro-osseous lesions, meningoencephaloceles, inflammatory or benign lesions such as schwannomas) or infiltration (malignancies) may cause numbness of the face and dry eye, respectively.
Invasive or expanding lesions of the sphenoid might destroy the adjacent vital structures. The presence of diplopia could be a sign of involvement of cranial nerve III, IV, or VI. Decreased visual acuity or light perception is an alarming sign of optic nerve involvement.
PHYSICAL EXAMINATION
Nasal endoscopy is now considered an essential diagnostic step in the evaluation of cranial base anatomy and pathology. Endoscopic exploration of the nasal fossa, nasopharynx, and cranial base is necessary for any tissue abnormality or liquorrhea. Watery nasal secretions should always be collected to detect β-2 transferrin protein, for patients with a high suspicion of CSF leak. The traditional neurologic examination of cranial nerves is always included for lesions of the cranial base. The audiometric examination could also be helpful in selected patients with a suspicion of involvement of the petrous apex.
In cases of a cranial base malformation, a thorough evaluation of the head and cranium is necessary. Most of these patients must be evaluated in a multidisciplinary manner with maxillofacial and neurosurgeons. Similarly, careful endocrinologic and neurosurgical assessments are required in case of pituitary pathology to properly plan the minimally invasive and major effective therapeutic option. A multidisciplinary approach is necessary as well for patients with orbital manifestations with screening by an ophthalmologist. Examination of the neck is required to evaluate the presence of lymphadenopathy, especially with malignant lesions of the cranial base.
INDICATIONS
The transpterygoid approach is indicated for accessing pathologies of the lateral recess of the sphenoid sinus or used as a corridor to reach pathologies of the middle cranial fossa (MCF) and posterior cranial fossa. Fibro-osseous lesions, JNA, meningo-encephalocele, schwannoma, and inverted papilloma are some examples of the diseases that can originate from or extend into the lateral recess of the sphenoid sinus. Pathologies of the paramedian–lateral structures of the middle cranial base such as the sella, parasellar area, and lateral portion of the cavernous sinus can be accessed by this approach as well (particularly in case of highly pneumatized lateral recess of the sphenoid).
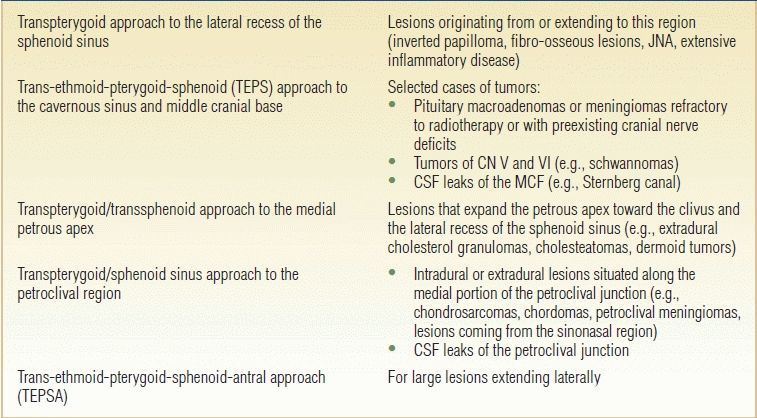
The indications for this approach depend upon the location, type, and consistency of the lesion; they are generally indicated when the neurovascular structures are not involved. Tumors with limited vascular supply and/or that compress and devascularize the cavernous sinus are most favorable for endoscopic resection. Preoperative embolization of hypervascular tumors of the cranial base can be useful. The possibility of this minimally invasive approach for biopsy procedures is particularly advantageous. Furthermore, the transpterygoid approach is indicated as a corridor to target different areas such as the medial petrous apex, infrapetrous region, inferior cavernous sinus, petroclival area, and ITF (Table 7.1).
Table 7.1 Indications for Transpterygoid Approach
CONTRAINDICATIONS
Contraindications for an exclusively endoscopic approach include the encasement of vital vascular structures (internal carotid artery [ICA] or perforating vessels) and the impossibility to treat or remove the lesion through the nasosphenoid corridor, as in the case of a tumor with a hard consistency and pial adherence. A purely endoscopic approach is also contraindicated in cases in which neurovascular surgery (ICA shunting) or orbital exenteration is needed. In these cases, a combined cranioendoscopic approach is preferable.
Nevertheless, the most important contraindication when choosing the type of approach remains the surgeon’s insufficient experience in the endoscopic management of these anatomical regions and overall inability to manage complications.
PREOPERATIVE PLANNING
The routine use of nasal endoscopy, CT scans, and MRI has improved the accuracy of the diagnosis of disease of the sphenoid sinus. Endoscopic and radiologic examinations allow for evaluation of the localization, size, and extent of lesions and, in some cases, can provide preoperative diagnosis (e.g., cholesterol granuloma, JNA) without resorting to biopsy. Preoperative endoscopic examination, together with CT scans, provides details on anatomic features (e.g., septal spur, concha bullosa, pneumatization of the sphenoidal rostrum, and pneumatization of the superior turbinate) that can influence the choice of the ideal surgical corridor. Identification of radiologic landmarks such as the vidian nerve, V2, ICA, optic nerve, and pneumatization of the PP is needed to avoid potential surgical hazards.
CT is extremely helpful in delineating the integrity of the bone and the variations of density. The finding of remodeling of the bone or erosion on CT requires careful evaluation of complementary soft tissue details on MRI. MRI plays a prominent role in imaging of the sphenoid sinus and the adjacent structures. Its high-contrast resolution combined with multiplanar capability makes it a valuable tool not only in the evaluation of benign and malignant neoplasms but also in the evaluation of aggressive inflammatory lesions. MRI allows identification of intracavernous structures in extreme detail and perfectly highlighting the intracavernous portion of the cranial nerves. The boundaries of the cavernous sinus, dura, and CSF are well defined. CT and MRI with contrast and angiography are particularly important to determine the consistency of the lesion, which helps to form the differential diagnosis. The imaging also helps to understand the relationship between the lesion and adjacent blood vessels. PET–CT is necessary for staging in malignant lesions prone to regional or distant metastasis.
Tissue biopsy is an essential step of the pretreatment evaluation. However, some pathology can be diagnosed based on clinical and radiologic assessment such as highly vascular lesions and meningo-encephalocele when biopsy is contraindicated. Before planning removal of a lesion, it is important to consider the histology of the tumor to avoid unnecessary surgery.
Early diagnosis is crucial because the presenting symptoms are both delayed and nonspecific, and often, diagnosis is made after the complication arises.
In order to avoid excessive bleeding during surgery, the patient should suspend all anticoagulant drugs and nonsteroidal anti-inflammatory drugs. Infectious sinonasal conditions should be resolved prior to surgery.
The patient must be informed about the possible risks of this operation, the hazards of neurovascular injury, and the possibility of duraplasty and that an external approach might be used as an alternative or complementary procedure. Of course, treatment should be based on multidisciplinary input including an otorhinolaryngologist, neurosurgeon, neurovascular interventionist, maxillofacial surgeon, neuroradiologist, and other related specialists.
SURGICAL TECHNIQUE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


