FIGURE 11.1 In this coronal scan, opacification of the left frontal sinus is seen.
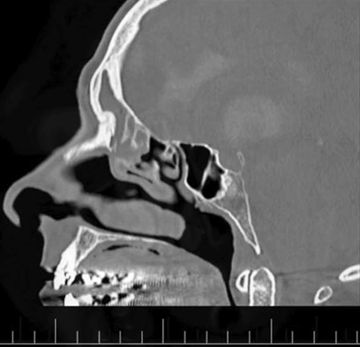
FIGURE 11.2 In the parasagittal CT scan, the opacification can be seen extending into the frontal recess.

FIGURE 11.3 The coronal T2-weighted MRI scan allows the distinction to be made between tumor and mucus in the opacified regions of the CT scans. The tumor can be seen filling the frontal recess and frontal sinus.
INDICATIONS
Benign nasal tumors are the most common to be addressed by this technique. These include frontal sinus inverting papillomas (Figs. 11.1 to 11.3), osteomas, fibrous dysplasia, meningoceles, and meningoencephaloceles. Malignant tumors isolated to the frontal sinuses are uncommon and may be metastatic, usually from the lung or breast, and, unless small and accessible, would not be approached with this technique. Malignant tumors extending into the frontal sinuses will have this approach as part of the resection, but consideration needs to be given as to where else the tumor extends and the involvement of surrounding structures.
CONTRAINDICATIONS
Although most areas of the frontal sinus can be accessed through the endoscopic modified Lothrop approach, osteomas involving the entire frontal sinus and following the contours of the sinus are easier to access through an osteoplastic approach. In general, osteomas that do not extend past the midpupillary line are approached in this way, and tumors extending beyond the midpupillary line are dealt with via an osteoplastic flap approach. While I prefer to deal with all inverting papillomas via the endoscopic modified Lothrop approach, even those extending to the far lateral regions of the frontal sinus, it may be easier to remove these very large and extensive tumors via an osteoplastic flap approach. Fibrous dysplasia and meningoencephaloceles that extend to or present lateral to the midpupillary line are also best removed via an osteoplastic approach.
PREOPERATIVE PLANNING
All patients have an image guidance CT scan performed prior to surgery. If there is no other sinus disease present, then surgery should start with an uncinectomy and clearance of the anterior ethmoids up to the frontal ostium. If, however, there is sinus disease present, then this is dealt with before the frontal sinuses are approached. In most cases, we would plan to do bilateral frontal sinus minitrephines as part of the surgery. This allows fluorescein-stained saline to be injected into the frontal sinus, and the passage of this fluorescein through the frontal sinus ostium marks the skull base; the skull base should remain safe if the surgeon stays anterior to the fluorescein.
SURGICAL TECHNIQUE
The first step is to complete any sinus surgery that is indicated. All patients will have an uncinectomy and maxillary antrostomy, but only those with disease in the posterior ethmoid and sphenoid will undergo a complete sphenoethmoidectomy. Next, the septal window is created. The landmarks for the septal window are consistent and should be followed in every case. The posterior limit of the septal window is the anterior end of the middle turbinate. The septal window is lowered until a straight instrument can be passed from one side through the septal window and under the middle turbinate axilla on the opposite side (Fig. 11.4). The anterior edge of the septal window is brought further anteriorly until the straight drill can access the bone of the frontal process of the maxilla anterior to the middle turbinate. The superior edge of the window is created by taking the window up onto the nasal vault. Leaving 3 to 4 mm of septal bone here will impair the dissection as one works from the one side across the septum onto the opposite frontal sinus. It is important that throughout this early part of the surgery that both scope and drill are placed from the one side through the septal window and drilling occurs on the opposite frontal sinus. This improves the angle and allows drilling to occur laterally under direct visualization. Attempting the bone removal from the same side of the dissection is very difficult and can be dangerous as the bone removal cannot be accurately visualized and damage can result inadvertently.
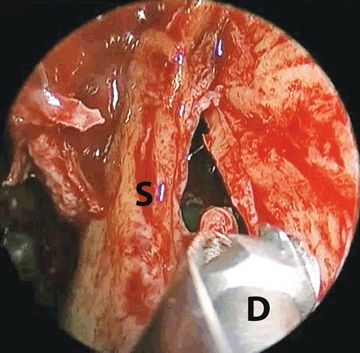
FIGURE 11.4 The septal window is lowered until a drill (D) can be passed from the one side of the nose across the septum (S) and under the axilla of the middle turbinate on the other side.
Once the other sinus surgery is complete, surgery on the frontal sinuses can begin. Our first step is to place bilateral minitrephines into the frontal sinuses to allow for fluorescein-stained saline to be flushed through the sinuses (Fig. 11.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


