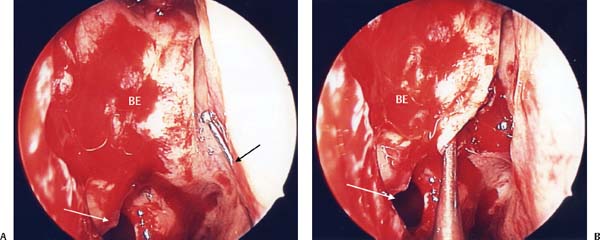
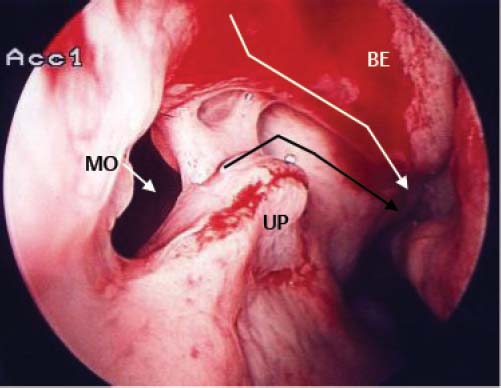
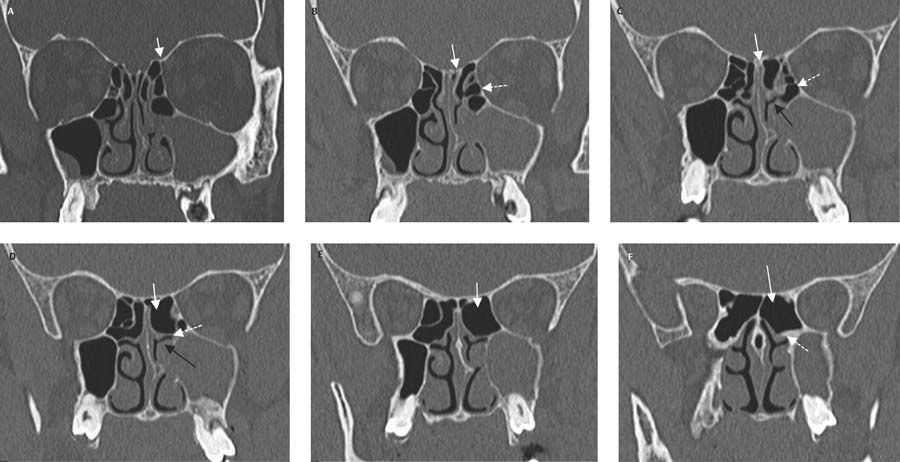
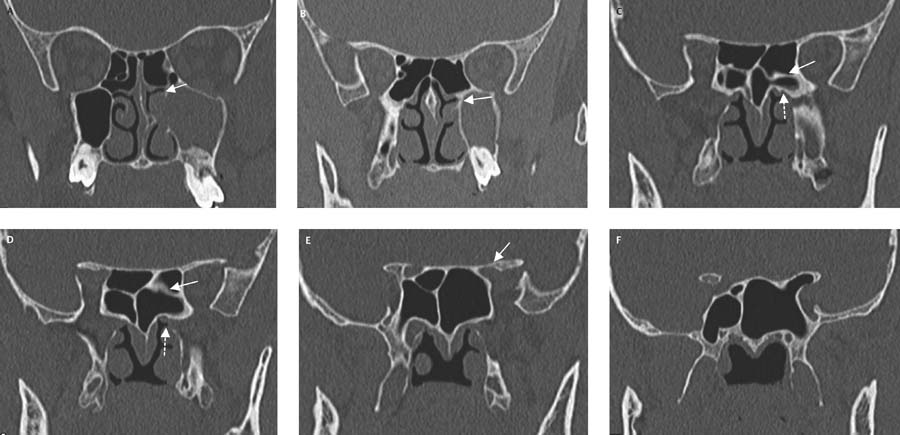
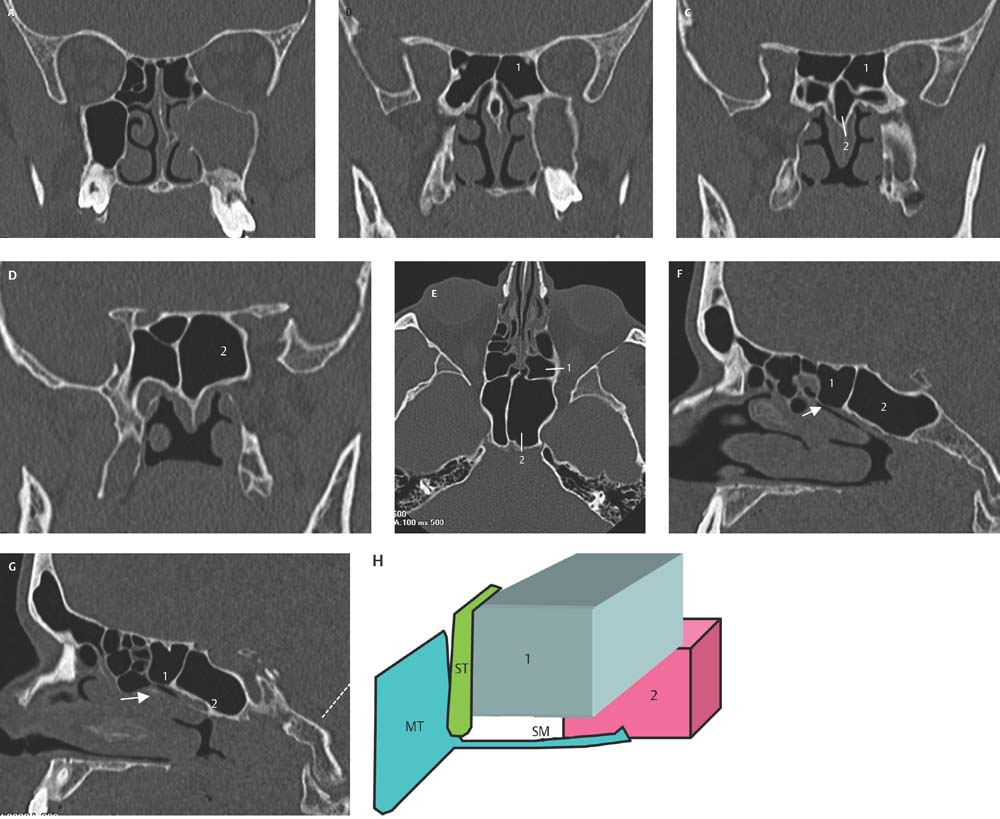
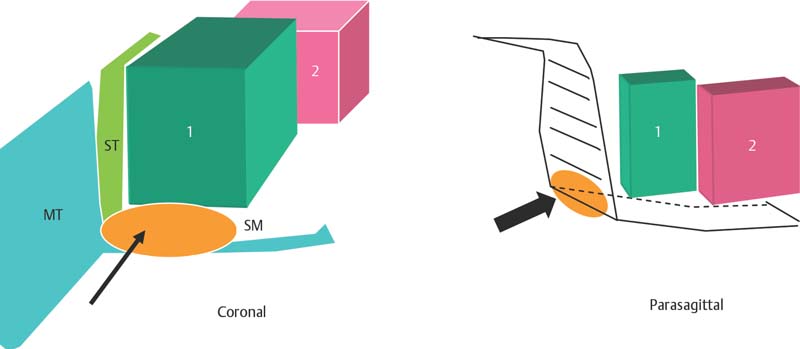
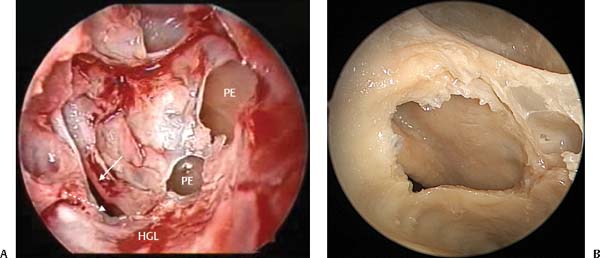
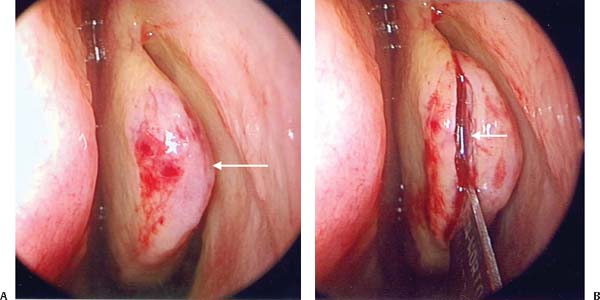
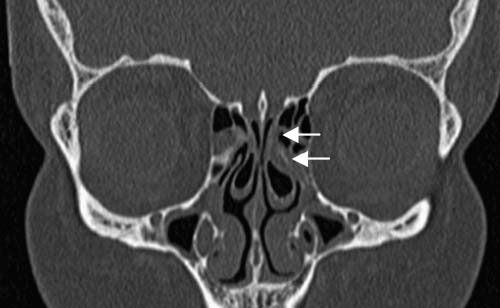
8 Reviewing the embryology of the sinuses, the middle turbinate forms from the third lamella and the superior turbinate from the fourth lamella. The ground lamella of the middle turbinate divides the ethmoid sinuses into anterior ethmoid sinuses (anterior to the ground lamella) and posterior ethmoid sinuses (posterior to the ground lamella). Anterior ethmoid sinuses are further subdivided into those associated with the frontal process of the maxilla—the frontal ethmoidal cells, and cells associated with the bulla ethmoidalis. The bulla ethmoidalis forms from the second embryological lamella. It is a large ethmoid air cell directly anterior to the middle turbinate lamella. Cells directly above the bulla ethmoidalis are referred to as suprabullar cells. Posterior ethmoidal cells are found behind the middle turbinate ground lamella and anterior to the lamella of the superior turbinate. The bulla ethmoidalis is either a single cell or group of cells which are visible directly behind the free edge of the middle and horizontal portions of uncinate process. The gap between the anterior face of the bulla ethmoidalis and the free edge of the uncinate process is known as the hiatus semilunaris which is the entrance to the ethmoidal infundibulum. When the anterior face of the bulla ethmoidalis extends to the skull base it usually forms the posterior limit of the frontal recess. However, when its anterior lamella fails to reach the skull base, a suprabullar recess is created. The bulla ethmoidalis will usually have a posterior wall which is separate from the vertical portion of the ground lamella. The space between its posterior wall and the ground lamella is known as the retrobullar recess. A suprabullar recess can also form from the retrobullar recess as it pneumatizes over the top of the bulla. The bulla ethmoidalis like all sinuses drains via a natural ostium. This can usually be found on its posteromedial aspect in the retrobullar recess. To find the natural ostium a double right-angled probe is passed medial to the bulla between the bulla and the middle turbinate. The tip of the probe is gently rotated laterally until it falls into the natural ostium (Fig. 8.1). As the probe is pulled forward, the medial and anterior walls are fractured. This fracture should be in continuity with the natural ostium. To open the bulla ethmoidalis the microdebrider is placed in this fractured area and the medial wall and anterior wall of the bulla removed. This allows the natural ostium to be enlarged and to be a part of the opening created into the bulla. This follows the general philosophy of endoscopic sinus surgery (ESS) of including the natural ostium in any opening made into a sinus. If only a mini-ESS has been performed (uncinectomy and opening of the bulla), then 3 or 4 mm of the anterior and inferior edge of the bulla is retained. This 3 to 4 mm of the anterior face of the bulla forms the posterosuperior part of the final common drainage pathway (see Chapter 5). This region is termed the “final common drainage pathway” as mucus from the frontal and anterior ethmoid cells and maxillary sinus is cleared to the nasopharynx along this pathway (Fig. 8.2). If a posterior ethmoidectomy is to be performed in addition to opening the bulla, none of its anterior wall is retained. Removing the bulla in its entirety gives improved access to the posterior ethmoid complex. As described in Chapter 6, three-dimensional (3D) anatomical reconstruction and planning of each surgical step is performed prior to dissection of the posterior ethmoids and sphenoid. In a similar manner as the agger nasi cell is used as the cornerstone of the dissection of the frontal recess dissection, a cell or space in the posterior ethmoids needs to be identified that can be accurately correlated to the computed tomography (CT) scan. The space used in the 3D reconstruction of the posterior ethmoids is the superior meatus. To be able to accurately identify the superior meatus on sequential CT scans, the transition from the anterior to the posterior ethmoids must be established on the CT scans. If the coronal CT scans are evaluated, the first landmark that is sought is the superior turbinate. Each sequential coronal CT is evaluated until the superior turbinate is identified (Fig. 8.3). Fig. 8.1 (A) The ball-probe (black arrow) is slid medial to the anterior face of the bulla ethmoidalis (BE). (B) The anterior face of the bulla is fractured creating an edge for the microdebrider. The maxillary sinus ostium is marked by a white arrow. Once the transition between the anterior and posterior ethmoids is established on the CT scans, the superior meatus (SM) should be sought. This is clearly marked in Fig. 8.3C,D. This space is directly above the horizontal part of the ground lamella and should be easily located on all CT scans. The ability of the surgeon to locate this space on both the CT scan and the patient is critical as it provides the starting point of the surgery. Once penetration of the posterior ethmoids has taken place through the ground lamella, the superior meatus and superior turbinate are identified (Fig. 8.1). The surgeon now has a landmark in the dissection that can be clearly placed on the CT scan. Each sequential cell in the posterior ethmoids is identified and, using the building block principle, a 3D picture of the posterior ethmoids can be constructed. However, before a complete understanding of the anatomy of the posterior ethmoids is possible, a clear understanding of the transition between posterior ethmoids and sphenoid is necessary. This follows the theme of understanding the transition between the frontal sinus and anterior ethmoids, between the anterior and posterior ethmoids, and finally between the posterior ethmoids and sphenoid. The key to determining the transition from the posterior ethmoids to the sphenoid is identifying the first coronal CT scan in which the solid posterior bony choanae can be seen (Fig. 8.4). Fig. 8.2 In this picture of the right nasal cavity, the final common drainage pathway is indicated by the black arrow. This also indicates the drainage pathway of the maxillary sinus. The white arrow indicates the drainage pathway of the frontal and anterior ethmoidal cells along the anterior face of the bulla ethmoidalis (BE). This portion of the BE forms the posterosuperior part of the final common drainage pathway. The residual portion of the uncinate process (UP) after uncinectomy and the natural ostium of the maxillary sinus (MO) are marked. In addition to the coronal CT scans, the parasagittal scan is helpful (Fig. 8.5). This scan is very useful in helping to place the cells either one on top of the other or anterior or posterior to the other cells of the posterior ethmoids. Cell number 3 is placed lateral to the parasagittal reconstruction and cannot be seen on scan Fig. 8.5C. Each configuration of the posterior ethmoids is different and each side of every patient needs to be independently assessed and the 3D picture built. Figure 8.5 scans and diagram illustrate the building block 3D reconstruction of the posterior ethmoids. Although not all the posterior ethmoid and sphenoid scans can be shown, refer back to Figs. 8.3 and 8.4 for additional CTs of the same patient if further clarification of the cells and reconstruction is needed. Note that once the superior meatus has been clearly identified in Fig. 8.5A scan, there is a single posterior ethmoid cell. This should be confirmed on both the parasagittal and coronal CT (Fig. 8.5E-G). Also note that the first CT on which the posterior bony choanae can be seen is Fig. 8.5C and there is a horizontal septation seen in that scan (between cells 1 and 2). Note on the two parasagittal scans (Fig. 8.5F,G) that the anterior face of the sphenoid is angled posteriorly allowing this wall to be cut by the CT giving the horizontal septation. On the left this is not carried significantly over the sphenoid and the optic nerve is not seen in cell 1 and therefore this does not represent an Onodi (sphenoethmoidal cell). The right side will be discussed later in this chapter. The 3D reconstruction demonstrates this slight posterior angulation of the anterior face of the sphenoid and also gives the surgeon a clear indication of exactly what to expect once the surgeon has entered the superior meatus and clearly identified this space and the anterior end of the superior turbinate. Fig. 8.3 The following six sequential CT scans are marked (A–F) and show the transition of the anterior to the posterior ethmoids. (A) The series starts at the anterior ethmoidal artery marked with a solid white arrow. (B) The superior turbinate is visible and this scan marks the transition from the anterior to posterior ethmoids. The broken arrow marks the beginning of the superior meatus. (C) The broken arrow again marks the superior meatus with the horizontal part of the ground lamella directly beneath the superior meatus (black arrow). (D) The solid white arrow marks the single large posterior ethmoid cell with the superior meatus (broken arrow) and horizontal ground lamella (black arrow) visible. (F) The single posterior ethmoid cell and the solid bone of the posterior choanae beginning to form (broken white arrow). This marks the beginning of the sphenoid sinuses. Fig. 8.4 (A,B) The superior meatus (solid white arrow) without any posterior bony choanae. (C) The solid bony choanae are first seen (broken white arrow) indicating the transition from the posterior ethmoids to the sphenoid. In most patients the cell directly above the solid bone of the choana is the sphenoid sinus. (D) A horizontal septation is seen (solid white arrow). This septation separates the sphenoid (always directly above the bony choanae) and the ethmoid cell pneumatizing over the top of the sphenoid. Fig. 8.5 A series of coronal CT scans (A–D) followed by an axial CT scan (E) and two parasagittal CT scans (F,G). (F) Scan is close is to the midline; (G) more lateral. Cells are numbered on the CT scan and in the three-dimensional reconstruction with cell 1 the single posterior ethmoid and cell 2 the sphenoid sinus. MT, middle turbinate; ST, superior turbinate; SM, superior meatus. Once a 3D reconstruction of the posterior ethmoids has been performed, a surgical plan is formulated as to how the dissection will be performed in the posterior ethmoids. The first step is to enter the superior meatus through the ground lamella in a region that can be easily identified on the CT scans. To achieve this, the transition from the posterior horizontal ground lamella to the vertical ground lamella needs to be identified. To positively identify the horizontal ground lamella, slide the endoscope under the middle turbinate toward the back end of the middle turbinate. As the posterior end of the middle turbinate is approached, the horizontal portion of the ground lamella is directly above the endoscope. The endoscope is brought anteriorly following the horizontal ground lamella until it tuns vertically. At the point where it turns vertically, in the area directly adjacent to the middle turbinate, the microdebrider or straight Blakesley is pushed through the ground lamella (Fig. 8.6). This access area is widened horizontally until the superior meatus and anterior edge of the superior turbinate are identified with certainty (Fig. 8.7). The surgeon can now place the point of dissection on the CT scans and knows how many and in what order the remaining cells are placed. These can then be sequentially entered and a complete dissection of the posterior ethmoids achieved. This low and medial entry into the posterior ethmoids minimizes the potential risk of damage to the skull base which may occur if entry is made higher on the vertical portion of the ground lamella.1 Fig. 8.6 The posterior ethmoids are entered at the junction of the horizontal and vertical portions of the ground lamella directly adjacent to the middle turbinate (as indicated by the black arrow). MT, middle turbinate; ST, superior turbinate; SM, superior meatus. In most patients the middle turbinate is preserved. It is important that during the surgery that the middle turbinate is not destabilized. The most common cause for destabilization of the middle turbinate is fracturing its anterior vertical insertion from the skull base. The axillary flap is designed to preserve this insertion but does remove some support from the anterior insertion of the middle turbinate. The horizontal portion of the ground lamella should also be preserved to give posterior stability to the middle turbinate. However, excessive manipulation of the middle turbinate can fracture the turbinate’s insertion on the skull base and result in it becoming floppy. The maneuver that should be avoided is placing the endoscope and instruments medial to the middle turbinate. The combination of a 4-mm endoscope and a 4-mm instrument will usually be enough to fracture the middle turbinate. Therefore the techniques of posterior ethmoidectomy and sphenoidotomy are described through the middle meatus medial to the superior turbinate rather than medial to the middle turbinate. Despite all attempts to preserve the middle turbinate, there are some situations where partial or total resection of the middle turbinate is necessary. Fig. 8.7 (A) Intraoperative picture illustrates the opening of the superior meatus on the left side (broken white arrow). The superior turbinate can be clearly seen (solid white arrow) and the partially opened posterior ethmoid (PE) cells are seen. (B) Cadaveric image on the left side. Penetration through horizontal ground lamella will immediately enter the superior meatus enabling a direct view of the superior turbinate. Fig. 8.8 (A) The concha bullosa is seen. Note the breadth of the middle turbinate (white arrow). (B) The scalpel has been used to vertically incise (white arrow) the concha separating the medial and lateral lamella. Patients with a concha bullosa need to have the lateral lamella of the middle turbinate removed to improve access to the middle meatus and, because this cell is often involved in the disease process, to clear the disease. To minimize damage to the lateral mucosa of the medial lamella, a scalpel is used to incise the anterior face of the concha bullosa vertically (Fig. 8.8). A pair of 5-mm endoscopic scissors* (Medtronic ENT, Jacksonville, FL) are used to continue the incision along the inferior margin of the middle turbinate to the lateral insertion of the turbinate on the lateral nasal wall. The scissors are used to continue the superior incision posterior as high as possible on the turbinate but progressively moving inferiorly as the posterior region of the turbinate is approached. Once the lateral lamella of the turbinate has been resected it is removed. The residual upward continuation of the lateral lamella of the middle turbinate needs to be removed as part of the frontal recess and bulla ethmoidalis dissection. Failure to remove this upward continuation can result in residual disease in the medial compartment of the anterior ethmoids (Fig. 8.9). The most common indication for middle turbinate resection is revision surgery with extensive polyposis. In patients who have previously undergone posterior ethmoidectomy, contracture of the horizontal part of the ground lamella may drag the middle turbinate laterally narrowing the ethmoidal space. This results in under ventilation of the posterior ethmoid region and could precipitate secretion retention in the posterior ethmoids and sphenoid and polyp formation.2,3 In patients with massive polyposis often from Samter’s triad (aspirin sensitivity, asthma, and polyps) or fungal sinusitis, increased aeration of the posterior ethmoid cavity may be necessary to reduce polyp recurrence.2,3 In these patients it may be necessary to partially resect the lower half of the middle turbinate and the horizontal portion of the ground lamella. This marsupializes the posterior ethmoids and sphenoid sinus (after a large sphenoidotomy) into the posterior nasal cavity with improved postoperative aeration of these sinuses (Fig. 8.10). This also facilitates the penetration of topical medications and nasal douches postoperatively. In some patients, especially those with long-standing severe septal deflections into the nasal cavity, the turbinate may be underdeveloped, very floppy, and lateralized. In these patients part of the turbinate may be resected at the time of surgery. When part of the middle turbinate is resected then the horizontal portion of the middle turbinate should also be removed flush with the lateral nasal wall. This almost invariably exposes the middle turbinate branch of the sphenopalatine artery with resultant bleeding and requires bipolar cautery (Fig. 8.11).
Three-Dimensional Reconstruction
and Surgery of the Bulla Ethmoidalis,
Middle Turbinate, Posterior Ethmoids,
and Sphenoid
 Surgery of the Bulla Ethmoidalis and Suprabullar Cells (Anterior Ethmoidectomy)
Surgery of the Bulla Ethmoidalis and Suprabullar Cells (Anterior Ethmoidectomy)
The Three-Dimensional Reconstruction of the Posterior Ethmoids
Surgical Plan for the Posterior Ethmoids (Videos 23 to 27)
The Middle Turbinate
Concha Bullosa (Videos 6 and 7)
Revision Surgery with Extensive Nasal Polyposis
Lateralized Atrophic Middle Turbinate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree