CHAPTER 72 The Esophagus
Anatomy, Physiology, and Diseases
Normal Esophageal Anatomy and Physiology
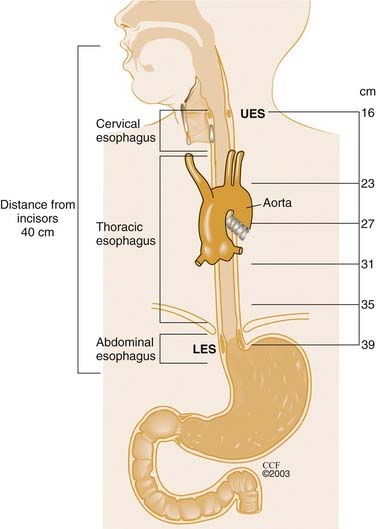
The proximal margin of the tubular esophagus is the upper esophageal sphincter (UES), the functional unit correlating anatomically with the junction of the inferior pharyngeal constrictor and cricopharyngeus.1 The esophagus extends distally 18 to 26 cm within the posterior mediastinum as a hollow muscular tube to the lower esophageal sphincter (LES) (Fig. 72-1). The LES is a 2- to 4-cm–long focus of tonically contracted thickened circular smooth muscle that lies within the diaphragmatic hiatus.2
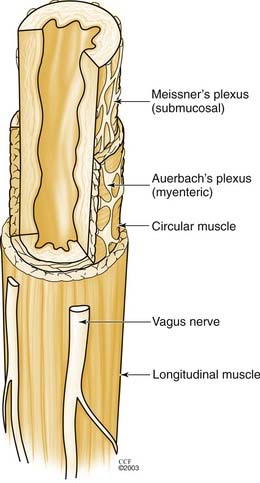
The esophageal wall is composed of four layers: mucosa, submucosa, muscularis propria, and adventitia. The esophagus has no serosa, making it unique to the rest of the gastrointestinal tract. The mucosa is normally composed of stratified squamous epithelium, lamina propria, and the muscularis mucosa. Lymphatic drainage begins in the lamina propria. The muscularis propria consists of both skeletal muscle and smooth muscle. The proximal 5% to 33% is skeletal muscle, the middle 35% to 40% is mixed, and the distal 50% to 60% is smooth muscle.3 The muscles are arranged into inner circular and outer longitudinal layers.
The smooth muscle portions of the esophageal body are innervated by the vagus nerve, which controls peristalsis under physiologic conditions. Neural innervation of the esophagus is from the myenteric or Auerbach’s plexus, located between the two muscle layers, and Meissner’s plexus, located in the submucosa.4 The myenteric plexus is responsible for esophageal peristalsis, whereas Meissner’s complex is the site of afferent sensory input (Fig. 72-2). Although the precise interaction between morphology and function of the nerve plexuses is not entirely clear, there are two main neurotransmitters within the myenteric plexus. Excitatory stimulation from acetylcholine mediates contraction of both the longitudinal and circular muscle layers. Inhibitory neurons predominantly affect the circular muscle layer via nitric oxide (NO). Excitatory stimulation from acetylcholine has its largest effect proximally, whereas the inhibitory effect of nitric oxide is seen distally.5
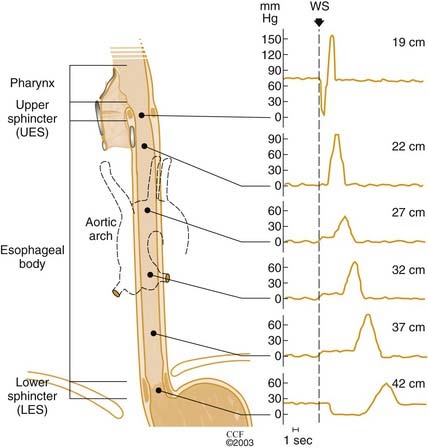
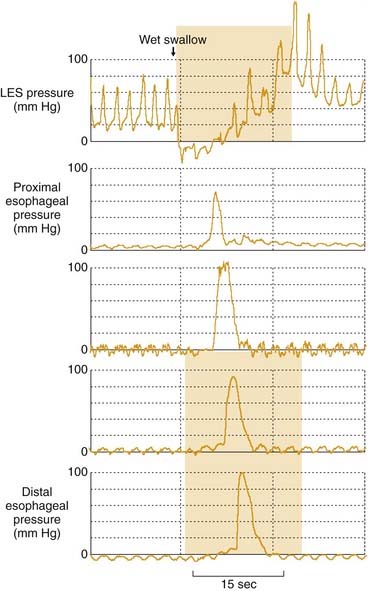
Functionally, the UES, the esophageal body, and the LES act in a coordinated manner to allow normal swallowing. Swallowing begins when a food bolus is propelled into the pharynx from the mouth. This oropharyngeal phase of swallowing is voluntary, but the esophageal phase that follows is involuntary. In rapid sequence and with precise coordination, the larynx is elevated and the epiglottis seals the airway. A rapidly progressing pharyngeal contraction then transfers the bolus through the relaxed UES into the esophagus. As the UES closes, a progressive circular contraction begins in the upper esophagus and proceeds distally along the esophageal body to propel the bolus through the relaxed LES (Fig. 72-3). Peristaltic pressures normally ranging from 30 to 180 mm Hg are generated.6–8 The measured pressure tends to be lower in the more proximal portions of the esophagus and greater in the distal smooth muscle portions.8 The pressures may also vary with the consistency of the bolus itself. The LES subsequently closes with a prolonged contraction, preventing movement back into the esophagus. The mechanical effect of peristalsis is a stripping wave, so called because it strips the esophagus clean from its proximal to its distal end.
Both the UES and LES are tonically contracted at rest. The closed state for the UES is a result of continuous neural excitation, with a small passive component to tone.9 The UES pressures are asymmetric, being higher anteriorly and posteriorly. During general anesthesia or sleep, this pressure falls to 10 mm Hg as a result of cessation of neural discharge.10 It is believed that the tonic contraction of the LES is a function of the muscle itself and is not dependent on neural innervation. Stimulation of inhibitory fibers results in LES relaxation. The resting tone of the LES is typically between 15 and 45 mm Hg and is affected by a wide array of events, foods, drugs, and hormones.8 LES relaxation occurs not only in response to swallowing but also in response to esophageal distention (secondary peristalsis) or without peristalsis. The latter is referred to as a transient lower esophageal sphincter relaxation (TLESR). TLESR is a vagally mediated reflex that is a part of normal digestion and is triggered by gastric distention. It represents the primary mechanism for gastroesophageal reflux in normal individuals and patients with mild gastroesophageal reflux disease (GERD).11
Esophageal Symptom Assessment
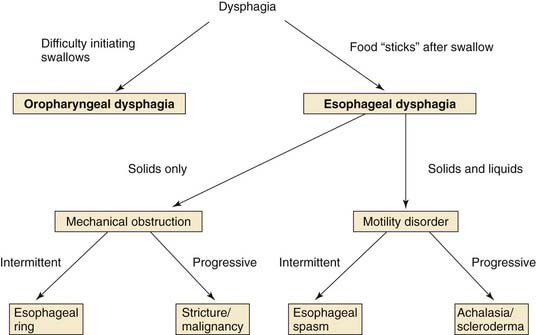
Dysphagia refers to the sensation of food being delayed in its normal passage from mouth to stomach. Patients often complain of a sensation of food “sticking.” It may be classified anatomically into two separate clinical entities, oropharyngeal and esophageal. Oropharyngeal dysphagia, discussed later in this chapter, is the difficulty in initiating a swallow. Esophageal dysphagia results from difficulty transporting food down the esophagus secondary to structural or neuromuscular defects in the smooth muscle portion of the esophagus. Further history can often establish the diagnosis in patients with esophageal dysphagia (Fig. 72-4). Patients with primarily solid food dysphagia typically have a structural lesion, such as a peptic stricture, ring, or malignancy. Esophageal rings tend to cause intermittent solid food dysphagia, whereas strictures and cancer cause progressive dysphagia. Patients with both solid and liquid dysphagia are more likely to have a motility disorder such as achalasia or scleroderma. The site at which a patient localizes dysphagia is of limited value. Although dysphagia in the retrosternal or epigastric areas frequently corresponds to the site of obstruction, dysphagia localized to the neck may be from either lower in the esophagus or the hypopharyngeal area.12,13
Oropharyngeal or transfer dysphagia is an abnormality related to the movement of a food bolus from the hypopharynx to the esophagus. Oropharyngeal dysphagia arises from disease of the upper esophagus, pharynx, or UES, in contrast to esophageal dysphagia, which is the difficulty in propagating food down the esophagus. Esophageal dysphagia arises within the body of the esophagus, as a result of either a mechanical or motility disturbance. A careful history may be adequate to make this distinction.14 Patients with oropharyngeal dysphagia typically present with difficulty initiating a swallow and immediately experience coughing, choking, gagging, or nasal regurgitation when attempting to swallow. Although patients with oropharyngeal dysphagia accurately localize the problem to the cervical or throat region, up to 30% of patients with esophageal dysphagia secondary to distal esophageal obstruction can localize the problem to the same area.12,13 Dysphagia must be distinguished from globus sensation. Globus is a sensation of a lump in the throat in which food transport is not limited. A key distinction is that globus is not related to swallowing and, in fact, may improve with swallowing. Most patients with globus do not give a history of dysphagia with food.
The distinction between oropharyngeal dysphagia and esophageal dysphagia is crucial, because the conditions have distinctly different causes (see Fig. 72-4). Oropharyngeal dysphagia is most commonly caused by disruptions in the finely coordinated act of swallowing secondary to neuromuscular dysfunction. In this setting, the symptoms may be more severe during the swallowing of liquids. History and physical examination should concentrate on neurologic signs and symptoms. Both sensory and motor injury may result in an inability to accomplish the transfer of a bolus to the esophagus. Any disease that affects the nerves or muscles can produce oropharyngeal dysphagia; the more common associations are cerebrovascular accidents, amyotrophic lateral sclerosis (ALS), Parkinson’s disease, myasthenia gravis, and tardive dyskinesia. Rarely, structural abnormalities, such as cervical osteophytes, hypopharyngeal diverticulum (Zenker’s diverticulum), tumors, and postcricoid webs, can cause oropharyngeal dysphagia. Affected patients typically note difficulty with a solid food bolus leaving the mouth. Although these structural abnormalities occur rarely, they are important to identify, because they may be amenable to endoscopic or surgical therapy.
Esophageal Testing
Endoscopy
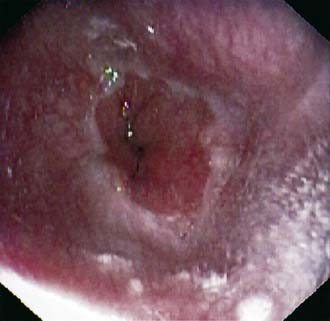
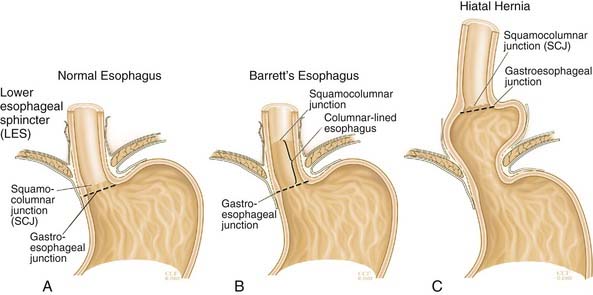
In the United States, upper gastrointestinal endoscopy is routinely performed with the patient under conscious sedation. After local anesthetic is sprayed on the posterior pharynx and intravenous sedation is given, the examination begins with insertion of the endoscope into the posterior pharynx. The posterior pharynx and larynx are examined for abnormalities. The endoscope is advanced under direct vision into the tonically closed UES. The patient is asked to swallow in order to relax the UES, and the endoscope is advanced into the proximal esophagus. The esophageal mucosa normally appears smooth and light pink. The mucosa should be thoroughly inspected for any abnormalities, including mucosal breaks, ulcers, strictures, and lesions. The area of the gastroesophageal junction (GEJ) must be carefully examined in order to identify specific landmarks. The squamocolumnar junction can be recognized from the irregular Z line demarcating the interface between the light pink esophageal squamous mucosa and the red columnar gastric mucosa (Fig. 72-5).15 The GEJ is defined by the proximal margin of the gastric folds. Although, the squamocolumnar junction and GEJ are normally located at the same level (Fig. 72-6A), the two are not synonymous. In patients with Barrett’s esophagus, the squamocolumnar junction is more proximal in the esophagus than the GEJ (see Fig. 72-6B). Endoscopy can also be used to diagnose the presence of hiatal hernia. In patients with a hiatal hernia, the GEJ is more proximal than the diaphragmatic indentation (see Fig. 72-6C) visualized by diaphragmatic contraction noted during patient respiration.
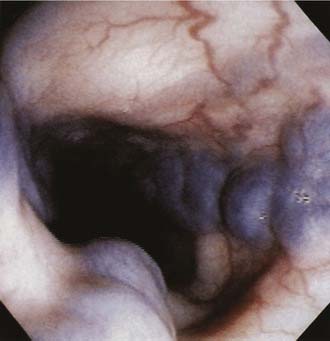
The current indications for endoscopy include presence of warning symptoms such as weight loss, upper gastrointestinal bleeding, dysphagia, odynophagia and chest pain, partial or no response to empiric therapy, and evaluation for Barrett’s esophagus. Esophageal causes of bleeding include severe esophagitis (Fig. 72-7), Mallory-Weiss tears (Fig. 72-8), and esophageal varices (Fig. 72-9).
Esophageal Manometry
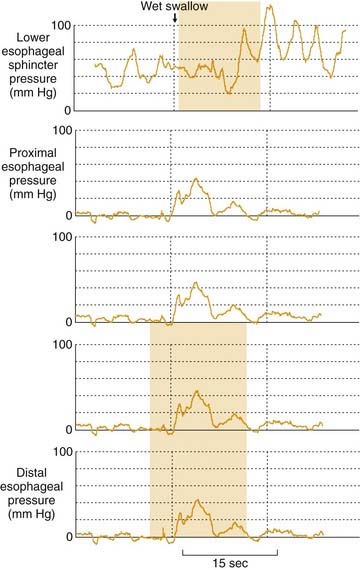
The technique of manometry involves inserting the catheter into the esophagus via the nares. The catheter is then advanced to approximately 60 cm, which should be well within the stomach. At this point, the patient is placed supine on the left side, and the catheter calibrated. The station pull-through technique is then employed. This involves slowly withdrawing the catheter through the LES, esophagus, and UES. Resting LES pressure and relaxation, esophageal peristalsis, and UES pressure and relaxation are thus evaluated with a series of wet swallows (Fig. 72-10).
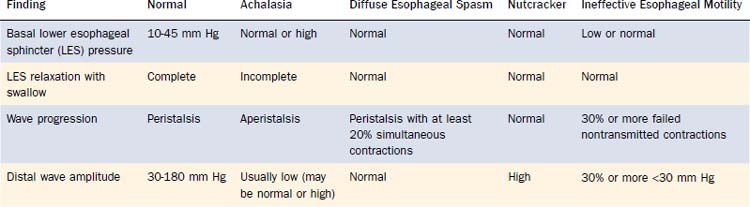
Manometry is the accepted standard for diagnosis of motor disorders of the esophageal body and LES. Manometric evaluation of the LES can accurately assess basal pressure and relaxation of the sphincter during swallowing. The esophageal body can be assessed for amplitude and duration of contractions and peristalsis. Peristalsis is defined by a coordinated contraction sequence and is quantified by the percentage of swallows with peristalsis. Through the use of these characteristics of the LES and esophageal body, a number of esophageal manometric disorders can be diagnosed (Table 72-1).
Table 72-1 Esophageal Manometric Findings in Normal Patients and in Patients with Motility Disorders
Manometric evaluation of UES often yields limited information, partly because of a great variability in what are considered normal values for UES resting pressure. Resting UES pressure is asymmetric, with greater values anteriorly and posteriorly than laterally.16 Also, the technique of measurement may stimulate sphincter contraction. In addition, the duration of UES relaxation depends on the volumes of swallow boluses. Because of these limitations, disorders of the UES may be better defined by barium radiography.
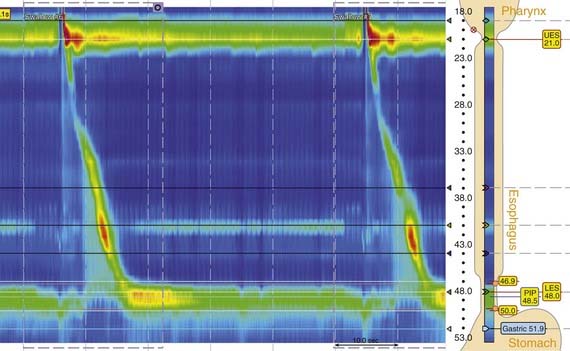
A solid-state high-resolution system has become available that is able to monitor esophageal function without the need for water perfusion. The solid-state manometry probe has 36 circumferential sensors spaced at 1-cm intervals. Each of the 36 pressure-sensing elements contains 12 circumferentially isolated sectors detecting pressure over a 2.5 mm length. The procedure involves simply placing the catheter in the esophagus, allowing a brief adjustment period, recording 10 swallows, and withdrawing the probe. Pressures detected by each sector are averaged to obtain a mean pressure measurement for each sensor, making each of the 36 sensors a circumferential pressure detector. The data are processed by a computerized program to create the plots that can be viewed as conventional line traces or switched to high-resolution plots. This method has significant potential advantages over conventional methods. It is simple, faster, and more precise. The software simplifies data collection and gives more accurate diagnostic information while shortening procedure time by 50% to 200%. Additionally, this novel technique provides a complete observation of motor function from the pharynx to the esophagus to the stomach without the need for catheter repositioning. The computer program is customized for processing the data into an isocontour pressure plot (Fig. 72-11).
Ambulatory 24-Hour Esophageal pH Monitoring
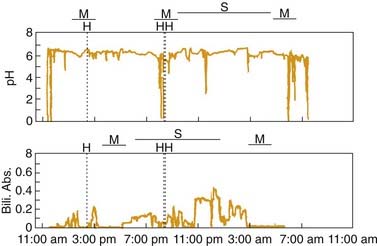
Standard pH monitoring measures distal esophageal acid exposure by using a single pH electrode catheter that is passed through the nose and positioned 5 cm above the superior margin of the manometrically determined LES. Although other techniques for electrode placement exist, such as pH step-up (rise in pH from stomach to esophagus), and endoscopic and fluoroscopic placement, they are less accurate and not standardized.17–19 After catheter placement, the patient is encouraged to have a typical day without dietary or activity limitations. The pH is recorded every 6 to 8 seconds, and the data are transmitted to an ambulatory data logger. Typical pH units have an event marker that can be activated by the patient during the study to indicate the timing of symptoms, meals, and recumbence (Fig. 72-12). The patient also records these events on a diary card so that specific symptoms can later be correlated with the esophageal acid exposure recorded by the pH probe. At the end of the study, data are downloaded to a computer, which generates a pH tracing and a data summary (Figs. 72-13 and 72-14).
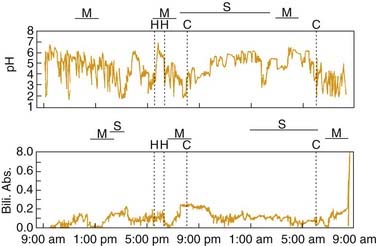
Figure 72-14. pH tracing of a patient with gastroesophageal reflux disease (GERD). Although the baseline pH varies considerably, several long episodes of reflux with pH less than 4 are shown. These events occur postprandially, not exclusively in relation to a meal as such events are in Figure 72-13. The total time during which the pH value is less than 4.0 is abnormal, and thus, the patient has GERD. The patient’s symptom of chest pain (C) correlates with episodes of reflux. Bili. Abs., bilirubin absorbance; H, heartburn; M, meal; S, supine.
A reflux episode is defined when the esophageal pH drops below 4.0. This value is chosen on the basis of the proteolytic activity of pepsin, which is most active at and below this pH. Additionally, a pH value less than 4.0 best distinguishes between symptomatic patients and asymptomatic controls.20–23 Some gastroesophageal reflux is physiologic and may be seen in normal individuals, especially after meals. Although many scoring systems and parameters have been evaluated, the percentage of time that the pH is less than 4 is the single most important parameter to measure and is calculated in most software programs used in the analysis of pH monitoring. Results are generally considered abnormal when the total time that the pH is less than 4 is exceeds 4.2% of the study period.24,25 Stratification by supine time and upright time is also reported by all software programs.
Although the pH software automatically calculates the total, upright, and supine reflux times, manual review of the pH tracing to exclude artifact is essential for precise interpretation. A typical reflux event involves an abrupt drop in pH (see Figs. 72-13 and 72-14). This must be distinguished from a slowly drifting pH value, which may be secondary to the probe’s losing contact with the esophageal mucosa and drying out. Probe dysfunction or disconnection can result in a reading that drops to zero. In addition, some patients may sip on acidic carbonated or citrus beverages, causing prolonged periods during which pH is less than 4. These artifacts should be identified and their corresponding time excluded from the calculation of acid exposure times.
One potential advantage of ambulatory pH monitoring is the ability to correlate symptoms with reflux episodes. However, even in patients with well-documented GERD, less than 20% of reflux episodes are associated with symptoms. This observation has led to the development of several scoring systems. The “symptom index score” is defined as the percentage of symptom episodes related to reflux events during the study period.26 Good correlation is considered to be 50%. The “symptom association probability” (SAP) score is a statistical probability calculation in which the entire pH tracing is separated into 2-minute intervals and each segment is evaluated for reflux and symptom episodes; a modified chi-square test is used to calculate the probability that the observed distribution could have occurred by chance.27 Unfortunately, no clinical trials prove that either of these symptom scores predicts a cause-and-effect relationship. This relationship can be confirmed only by the response to appropriate antireflux therapy.
Monitoring of pH may be performed with or without medical therapy. In monitoring performed without medical therapy, patients are asked to stop proton pump inhibitor (PPI) therapy for at least one week, histamine H2 blocker therapy for 48 hours, and antacid use for 2 hours.28 Whether the study should be performed with or without therapy depends on what information the clinician desires to gain. A pH study without therapy simply documents whether acid reflux is present, such as in a patient considering antireflux surgery or with atypical GERD symptoms. The study performed in a patient undergoing therapy documents whether continued acid reflux is the cause of symptoms in patients with poor or incomplete response to therapy.
Multiple-probe catheters have additional pH electrodes located more proximally in the esophagus or the hypopharynx. These electrodes allow the detection of proximal esophageal and pharyngeal acid reflux events, which may be useful in the evaluation of extraesophageal GERD symptoms, particularly laryngitis, chronic cough, and asthma. The conventional location of the proximal esophageal pH probe is 15 cm to 20 cm above the LES, with a normal value for total time with pH below 4.0 being less than 1%.29,30 The hypopharyngeal probe is usually placed 2 cm above the manometrically determined UES. Although normal values are not clearly defined, more than two or three episodes of hypopharyngeal reflux is considered abnormal. It is again critical to review the pH tracings to be sure that proximal esophageal or hypopharyngeal reflux events are accompanied by distal esophageal reflux and are not secondary to artifacts. The clinical utility of these multiple-probe catheters is considered later in the atypical reflux discussion.
Ambulatory 24-Hour Bile Monitoring
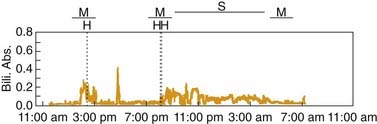
Duodenogastroesophageal reflux (DGER) refers to regurgitation of duodenal contents through the pylorus into the stomach, with subsequent reflux into the esophagus. DGER may be important because factors other than acid, namely bile and pancreatic enzymes, may play a role in mucosal injury and symptoms in patients with GERD.31–33 Initially esophageal pH greater than 7.0 during pH monitoring was considered a marker of such reflux, but alkaline reflux was later proved to be a poor marker for DGER.31 This finding led to the development of a fiberoptic spectrophotometer (Bilitec 2000, Synectics, Stockholm), that detects DGER in an ambulatory setting independent of pH (Fig. 72-15).34 This instrument utilizes the optical properties of bilirubin, the most common bile pigment. Bilirubin has a characteristic spectrophotometric absorption band at 450 nm. The basic working principle of this instrument is that absorption near this wavelength implies the presence of bilirubin and, therefore, represents DGER.
As in pH monitoring, data from the bilirubin spectrophotometer are usually measured as percentage of time that bilirubin absorbance is greater 0.14 and can be analyzed separately for total, upright, and supine periods (Fig. 72-16). Percentage of time bilirubin absorbance exceeds 0.14 is commonly chosen as a cutoff because studies show that values lower than this number represent scatter owing to suspended particles and mucus present in the gastric contents.34 In a study using 20 healthy controls, the 95th percentile values for percentage of total, upright, and supine times that bilirubin exceeded 0.14 were 1.8%, 2.2%, and 1.6%, respectively.35 Several reports have indicated a good correlation between Bilitec fiberoptic spectrophotometer readings and bile acid concentration measured by duodenogastric aspiration studies.34,36–38 Validation studies have found that this instrument underestimates bile reflux by at least 30% in an acidic medium because of bilirubin isomerization with a shift in wavelength absorption.35 Therefore, the instrument’s measurement of DGER must always be accompanied by simultaneous measurement of esophageal acid exposure by means of prolonged pH monitoring. Furthermore, a variety of substances may result in false-positive readings by this instrument, because it indiscriminately records any substance with an absorption band around 470 nm. This fact necessitates the use of a modified diet to avoid interference and false readings.34,38 Also, it is important to remember that the Bilitec spectrophotometer measures reflux of bilirubin and not bile acids or pancreatic enzymes, thereby assuming that the presence of bilirubin in the refluxate is accompanied by other duodenal contents.
New Technologies
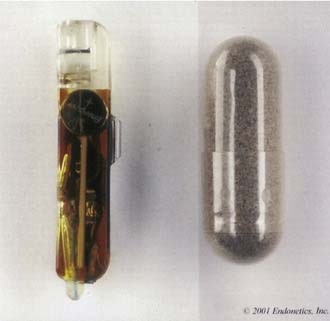
The Bravo is a catheter-free monitoring system in which a pH monitoring probe approximately the size of a medication capsule is placed endoscopically (Fig. 72-17). A standard upper gastrointestinal endoscopy is performed to locate the GEJ. The endoscope is removed, and an introducer with an attached pH capsule probe is inserted. The introducer is advanced and the capsule probe is placed 6 cm above the GEJ (Fig. 72-18). pH data are then transmitted to a recording device on the patient’s waist. Besides being catheter free, the wireless system has the advantage of recording 48 hours of pH data. The capsule pH probe falls off after 4 to 10 days and is passed in the stool. The wireless system is significantly better tolerated, causing less interference with daily activities, and having a higher overall satisfaction rate and better quality of life for patients with GERD. The second, often discussed, and important advantage of the Bravo system is its greater sensitivity for detecting reflux events due to (1) prolonged monitoring (48 hours vs. 24 hours), (2) improved patient compliance, (3) reduced impairment of patients’ daily activity, and (4) decreased likelihood of catheter movement during the study.
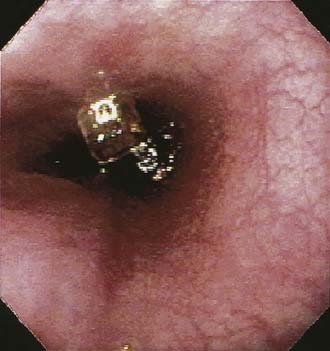
Figure 72-18. The Bravo wireless pH capsule (Medtronic Inc, Minneapolis, MN) attached to the distal esophageal mucosa after deployment.
The latest pH monitoring system is the Restech Dx–pH Measurement System, a highly sensitive and minimally invasive device for detection of acid reflux in the posterior oropharynx. It uses a nasopharyngeal catheter able to measure pH in either liquid or aerosolized droplets. The probe is a 1.5-mm–diameter oropharyngeal catheter with a wireless digital ZigBee transmitter attached to the shirt collar. The catheter employs a 3.2-mm teardrop tip to aid in insertion and to ensure that the sensor is positioned in the airway. The tip has a colored light-emitting diode (LED) for oropharyngeal visualization, to aid proper placement (Fig. 72-19). The sensing element consists of a circular 1-mm antimony surface and a reference electrode separated by a 0.05-mm polymer insulator (Fig. 72-20). Moisture from exhaled air condenses on the sensor surface, creating a fluid layer that bridges the gap between the antimony and reference sensor elements. The sensor records pH values twice every second (2 Hz), and it features a hydration monitor to eliminate data if the tip dries out. Special circuitry monitors each reading to ensure sufficient sensor hydration. This circuitry prevents the inclusion of dryout-related “pseudo-reflux” events in the data. The potential clinical utility of this device is in patients with extraesophageal reflux disease. Clinical data are needed to assess the future role of this device.

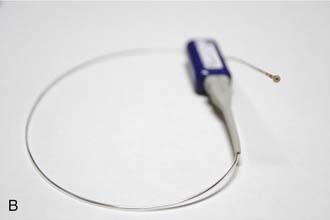
Figure 72-19. A, Oropharyngeal pH probe with light-emitting diode (LED) tip in the posterior aspect of the mouth. B, The probe transmitter.
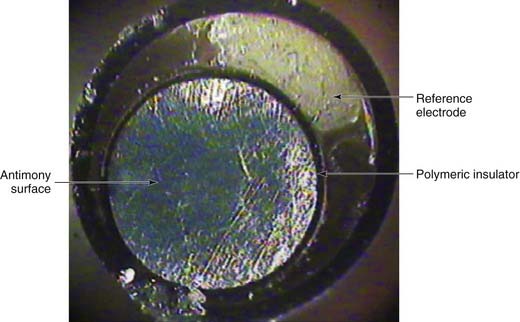
Figure 72-20. Magnified cross-sectional view of the Dx–pH probe (Restech Respiratory Technology Corporation, San Diego, CA) (×75).
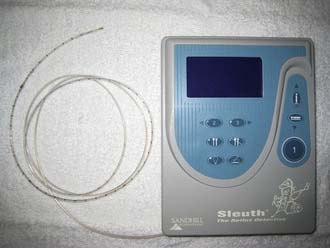
Multichannel intraluminal impedance (MII) is a relatively new technique that measures both acidic and nonacidic refluxates of liquid or gas consistency.39 This ZepHR impedance/pH recorder (Sandhill Scientific Inc, Highlands Ranch, CO) is capable of measuring characteristics of gastroesophageal reflux that are not detectable by the current “gold standard,” the pH probe. Impedance, a measure of the total resistance to current flow between adjacent electrodes, is capable of differentiating between liquid and gas refluxates on the basis of their inherent current and resistance properties. Combined MII-pH measurement has an advantage over standard pH monitoring, which does not detect nonacidic reflux. Hence, clinically this approach may be most useful for further evaluation of typical or atypical reflux symptoms refractory to acid suppression therapy, in assessing the role of nonacid and/or nonliquid reflux. Although there is no doubt that MII-pH measurement is currently the most accurate and detailed method to detect reflux of all kinds, the clinical indications for its use are still evolving, and its role in the management of patients with GERD awaits further definition for two main reasons: (1) the relevance of nonacid reflux in specific clinical settings has to be further discerned, and (2) there is a paucity of high-quality blinded, randomized, controlled studies examining the benefit of treating nonacid reflux.
Provocative Testing
Provocative testing in the esophagus is mostly of historical value. Such testing arose because of the difficulty in evaluating patients with noncardiac chest pain. The Bernstein test, introduced by Bernstein and Baker40 in 1958, is an acid perfusion test used as an objective method to reproduce symptoms of acid related injury. After a brief control period, consisting of intraesophageal saline infusion, 0.1 N hydrochloric acid is infused in the esophagus. If the infusion produces the patient’s chest pain and saline does not, the result is considered positive. Because of its low sensitivity, especially in comparison with pH monitoring, the Bernstein test is now rarely used.41,42
The edrophonium test is a provocative test designed to implicate esophageal motility disorders as a cause of chest pain. Edrophonium, a parasympathomimetic, increases the amplitude and duration of esophageal contractions. The tests consists of an intravenous injection of 80 µg of edrophonium, which reproduces esophageal manometric changes and chest pain in 20% to 30% of patients with noncardiac chest pain.43,44 As with the Bernstein test, the sensitivity of this test is low and varies widely in the literature. Also, studies have shown poor correlation between increased amplitude and duration of esophageal contractions and patient’s symptoms of chest pain.44–46
Esophageal Disease States Causing Dysphagia
Esophageal Motility Abnormalities
Box 72-1 highlights the latest classification system for esophageal motility disorders.47 This system categorizes such disorders according to four major patterns of esophageal manometric abnormalities: inadequate LES relaxation, uncoordinated contraction, hypercontraction, and hypocontraction.47 Most esophageal motility abnormalities fall predominantly into one of these four major categories, although there can be considerable overlap.
Box 72-1 Classification of Esophageal Motility Abnormalities
Data from Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut. 2001;49:145-151.
Achalasia
Achalasia is a primary esophageal motility of unknown etiology characterized by insufficient LES relaxation and loss of esophageal peristalsis. Available data suggest hereditary, degenerative, autoimmune, and infectious factors as possible causes.48,49 Pathologic changes occur in the myenteric plexus, consisting of a patchy inflammatory infiltrate of T lymphocytes, eosinophils, and mast cells, loss of ganglion cells, and myenteric neural fibrosis.50 These changes result in selective loss of postganglionic inhibitory neurons, which contain both nitric oxide and vasoactive intestinal polypeptide. The postganglionic cholinergic neurons of the myenteric plexus are spared, leading to unopposed cholinergic stimulation.51 This condition produces high basal LES pressures, and the loss of inhibitory input results in insufficient LES relaxation. Aperistalsis is related to the loss of the latency gradient along the esophageal body—a process mediated by nitric oxide.
The most common symptoms of achalasia are dysphagia for solids and liquid, regurgitation, and chest pain. Most patients are symptomatic for years before seeking medical attention. Patients with achalasia tend to localize their dysphagia to the cervical or xiphoid areas. Initially, dysphagia may be for solids only, but most patients have dysphagia for solids and liquids at the time of presentation.48 Patients tend to accommodate for their problem by using various maneuvers, including lifting the neck or drinking carbonated beverages to help empty the esophagus. Regurgitation occurs in 75% of patients with achalasia and becomes a greater problem as the esophagus dilates with progression of the disease.52 It occurs most commonly in the recumbent position and may awaken the patient from sleep because of choking and coughing. Chest pain is experienced by approximately 40% of patients with achalasia.52 Weight loss occurs in 60% but is usually minimal.53
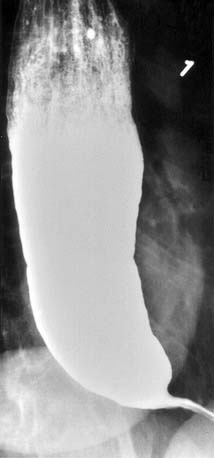
When the diagnosis of achalasia is suspected, a barium esophagram with fluoroscopy is the best initial diagnostic study. This test reveals loss of primary peristalsis in the distal two thirds of the esophagus. In the upright position, there is poor emptying, with retained food and saliva often producing a heterogeneous air-fluid level at the top of the barium column. The esophagus may be dilated (Fig. 72-21). In early disease the dilation is often minimal, but in chronic disease it can be massive with a sigmoid-like tortuosity (Fig. 72-22). There is a smooth tapering of the lower esophagus leading to the closed LES that resembles a bird’s beak. The presence of an epiphrenic diverticulum may also suggest the diagnosis of achalasia.54

Figure 72-22. Esophagram of late-stage achalasia. The esophagus now has a sigmoid-like tortuosity with a large amount of retained debris.
Esophageal manometry may also be used to establish the diagnosis (Fig. 72-23).55 In the body of the esophagus, aperistalsis is always present. This means that all swallows are followed by simultaneous contractions, typically with low contraction amplitudes. Abnormal LES relaxation is seen in all patients with achalasia. About 70% to 80% of patients have absence or incompleteness of LES relaxation with swallows; in the remainder, the relaxations are complete but are of short duration. The baseline LES pressure is usually elevated but may be normal in up to 45% of patients; however, a low LES pressure is never seen in untreated patients with achalasia.
All patients with achalasia should undergo upper endoscopy to exclude pseudoachalasia arising from a tumor at the GEJ. Pseudoachalasia may mimic classic achalasia both clinically and manometrically. This diagnosis should be suspected in patients of older age with a short duration of symptoms and more significant weight loss.56 At endoscopy, the esophageal body in classic achalasia often appears dilated and tortuous. Retained secretions and food debris may be encountered (Fig. 72-24). The LES region usually appears puckered and remains closed with air insufflation; however, with gentle pressure the endoscope can transverse this area. The GEJ and gastric cardia must be examined closely for the presence of tumors in order to rule out pseudoachalasia.
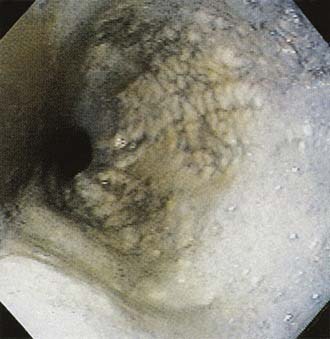
Figure 72-24. Endoscopic view of the distal esophagus in a patient with achalasia. The esophagus is dilated with retained fluid and debris.
There is no cure for achalasia, but most patients can obtain relief of symptoms and improvement in esophageal emptying. The two most effective treatments are graded pneumatic dilation and surgical myotomy. All patients considered for pneumatic dilation should be surgical candidates, because the procedure is associated with a 2% to5% risk of esophageal perforation.49,57 Pneumatic dilation, performed endoscopically, uses air pressure to dilate and disrupt the circular muscle fibers of the LES. Balloon dilators, available in three diameters (3, 3.5, and 4 cm) are positioned over a guidewire at endoscopy. The most important aspect of an effective pneumatic dilation is accurate positioning of the balloon across the LES, followed by fluoroscopic visualization of effective obliteration of the balloon waist. After pneumatic dilation, all patients should undergo a (Gastrografin) study followed by barium swallow to exclude esophageal perforation.58 Studies to date indicate good-to-excellent relief of symptoms in 50% to 93% of patients in whom the graded dilators were used.49 The clinical response improves in a graded fashion with increasing size of the balloon diameter.57 Surgical myotomy for achalasia involves performing an anterior myotomy across the LES (Heller’s myotomy) usually associated with an antireflux procedure. Myotomies are increasingly being performed by laparoscopy, which has a good-to-excellent response rate of 80% to 94%.49 A potential complication of myotomy is GERD, which occurs in 10% to20% of cases.59
For patients who are at high risk for pneumatic dilation or surgery, endoscopic injection of the LES with botulinum toxin (Botox) or pharmacologic treatment with nitrates or calcium channel blockers may be acceptable alternatives. Botulinum toxin injection, which inhibits the release of acetylcholine from nerve terminals, is initially effective in about 85% of patients.49 However, symptoms recur in more than 50% of patients at 6 months.60 Therefore, botulinum toxin injection is reserved for elderly patients for whom surgery poses a high risk. Calcium channel blockers and long-acting nitrates are effective in reducing LES pressure and temporarily relieving dysphagia but do not improve either LES relaxation or peristalsis.61,62 The clinical response is short acting, the agents usually do not provide complete symptom relief, and their efficacy decreases with time. Given these limitations, pharmacologic therapy is recommended only for patients who are not candidates for pneumatic dilation or surgical myotomy and in whom botulinum toxin injections fail.63