Techniques of Prenatal Diagnoses
Karen L. Smith-Silone
James E. Silone Jr.
The development of prenatal diagnosis has been an important advance in the field of clinical genetics.1 Techniques in prenatal diagnosis have made it possible for genetic counselors and parents to transform risks of certain genetic diseases from purported intermediate risks (5%, 25%, or 50%) to 0% or 100%. Although it is impossible currently to identify all genetic abnormalities, screening and diagnostic programs are available to detect the most common chromosomal defects prenatally. The techniques of prenatal diagnosis include maternal serum screening, amniocentesis, ultrasound, chorionic villi sampling, and cordocentesis.
BACKGROUND
Down syndrome and other autosomal trisomies increase with maternal age (Table 1).1,2 Genetic amniocentesis is generally offered to women who will be 35 years or older at delivery. At this age, the incidence of trisomy starts to increase rapidly. However, 87.1% of children are born to women who are less than 35 years of age at delivery, so the majority of children with Down syndrome are born to younger women.2 Because of advances in ultrasound techniques and biochemical markers, noninvasive methods of prenatal diagnosis are becoming more prevalent.
TABLE 1. Risk of Having a Live-Born Child with Chromosomal Abnormalities | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
INDICATIONS FOR PRENATAL DIAGNOSIS
The most common indication for prenatal diagnosis is the routine screening of the general population.2 The most common methods of screening include ultrasound and maternal serum biochemistry. Table 2 lists the indications for which a couple should be offered prenatal testing. The incidence of Down syndrome increases as maternal age increases. The relationship between the incidence of Down syndrome and maternal age was noted long before the chromosomal etiology of the syndrome was known. Other chromosomal trisomies, such as trisomy 13; trisomy 18; 47, XXY; 47XXX; and 47XYY, may also increase with age.3,4
TABLE 2. Indications for Prenatal Diagnosis | ||||||||
|---|---|---|---|---|---|---|---|---|
|
In 1952, metabolic disorders were first demonstrated to be the result of an absence of a normally functioning enzymatic or structural protein.5 Most of these metabolic disorders are inherited in an autosomal-recessive manner; approximately 0.8% of newborns have such a disorder.6 Couples who are both heterozygous carriers of an autosomal-recessive genetic trait have a 25% risk of a homozygous affected fetus in each pregnancy. The metabolic conditions amenable to prenatal diagnosis include mucopolysaccharidoses, mucolipidoses, sphyngolipidoses, lysosomal-storage forms of carbohydrate metabolic disorders, aminoacidopathies with cultured cell expression of a known enzymatic defect, and a growing list of heterogeneously classified disorders.1,7
Women who are either known or suspected carriers of an X-linked recessive disorder may wish to use prenatal diagnosis because of the potential risk of 50% of male offspring having the disorder in question. Carrier tests for X-linked conditions are difficult and in many cases are not completely reliable. Therefore, many women may choose to consider themselves carriers when test results are in doubt. Presently, only a few X-linked conditions (e.g., Fabry’s syndrome, Hunter’s syndrome, Menkes’ kinky hair syndrome, and Lesch-Nyhan syndrome) can be diagnosed by enzymatic analysis.1,5 Duchenne-type muscular dystrophy and classic hemophilia can be diagnosed by fetal blood aspiration and serum creatine phosphokinase determination.8 Other mothers may choose to undergo amniocentesis in order to identify the fetal gender by chromosomal study or to determine testosterone levels, electing to bear only girls, who will be unaffected.9
TECHNIQUES IN PRENATAL DIAGNOSIS
METHODS OF SCREENING AND DIAGNOSIS
Maternal Screening
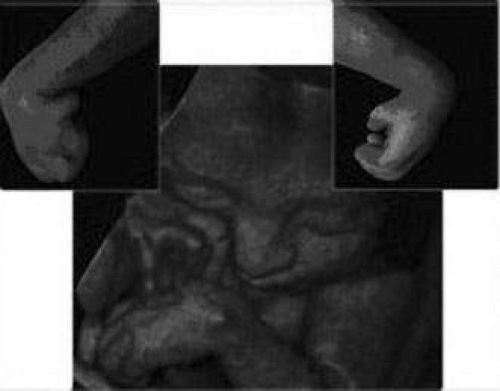
Maternal serum screening can identify pregnant women who are at an increased risk for having a baby with certain birth defects. Patient-specific risks for open spina bifida, Down syndrome and trisomy 18 (Edwards syndrome) (Fig. 1) can be determined by measuring the levels of certain proteins in maternal serum and combining those data with the patient’s maternal age and clinical information.10 Women with a positive screen should be offered a definitive diagnostic test.
Serum Alpha-Fetoprotein
Until the mid-1980s, there was no way to identify younger women at risk of having children with Down syndrome. Down syndrome screening for younger women was initiated when researchers discovered that the mean level of maternal serum alpha-fetoprotein (AFP) in pregnancies complicated by Down syndrome is 0.7 multiples of the normal medium (MOM).2 AFP can also be used to detect at least 80% of open neural tube defects, such as spina bifida.
Alpha-Fetoprotein P X-tra/Triple Screen Test
Shortly after the associated between AFP and Down syndrome was established, it was found that higher levels of human chorionic gonadotropins (hCG) and lower levels of unconjugated estriol levels (uE3) were also associated with Down syndrome.2 These three markers were combined to make the Triple Screen Test. Together, these markers are combined with gestational age, maternal age, weight, race, number of fetuses (up to twins), and presence of maternal diabetes to provide patient-specific risks for open spina bifida, Down syndrome, and trisomy 18. The Triple Screen Test detects at least 80% of open neural tube defects and at least 60% of Down syndrome and trisomy 18.10 Although serum screening does not detect other aneuploidies with great frequency, the aneuploidies likely to be missed by serum screening usually are ultimately lethal (e.g., trisomy 13) or are gender-chromosome abnormalities not associated with profound mental retardation or other severe physical or developmental limitations.
Maternal blood sampling can be performed between 15 and 20 weeks of gestation but is most accurate when performed between 16 and 18 weeks of gestation. Accurate pregnancy dating is essential.
Alpha-Fetoprotein Tetra/Quad Screen
AFP tetra adds a fourth marker, dimeric inhibin A (DIA), to the AFP X-tra. AFP Tetra increases the detection efficiency of Down syndrome by approximately 15%, while slightly lowering the false-positive rate. DIA is a glycol protein hormone made by the ovary and placenta. DIA levels are twice as high in Down syndrome pregnancies.11 Unlike AFP, hCG, and uE3, DIA does not vary with gestational age, resulting in greater screening accuracy.
Pregnancy-Associated Plasma Protein-A and β-Human Chorionic Gonadotropin
Many maternal serum analytes have been evaluated for possible use for first-trimester Down syndrome screening.12 Pregnancy-associated plasma protein-A (PAPP-A) is a highly glycosylated, high molecular weight protein and is produced by the human placenta and released into maternal circulation during pregnancy.13 Maternal serum concentrations of PAPP-A have been found to be reduced in pregnancies affected by Down syndrome in the first trimester when compared to normal, unaffected pregnancy at the same gestational period. This reduction is most pronounced before the twelfth week of gestation. Later, serum concentrations in Down syndrome gradually reach the control range and, in the second trimester, PAPP-A does not distinguish between normal and Down syndrome pregnancy. Therefore, accurate gestational dating is needed.
In the less frequent cases of fetal trisomy 18 and 13, first trimester maternal serum PAPP-A is even more strongly reduced than in Down syndrome, and preliminary results indicate that in fetal trisomy 18 PAPP-A continues to be below the normal range, including in the early second trimester (weeks 15 to 20).
Early pregnancy maternal serum PAPP-A is also reduced in nonviable pregnancies and threatened abortion and is absent in the very rare Cornelia de Lange syndrome. In ectopic pregnancies, PAPP-A has also been found to be
reduced.
β Subunit of hCG is also produced by the placenta. When combined with PAPP-A, a 65% detection rate for Down syndrome can be achieved, with a 5% false-positive rate. When PAPP-A and β-hCG are combined with an ultrasound obtained nuchal translucency (to be discussed later in the text), an 86% detection rate for Down syndrome with a 5% false-positive rate can be achieved, while providing results earlier in the pregnancy so that a woman may have the choice of chorionic villus sampling (CVS) or amniocentesis.14,15,16,17,18 Both of these procedures will be discussed in depth later in the chapter. The first trimester only screen also affords the chance for women to make personal decisions regarding prenatal diagnosis and termination earlier in the pregnancy.
AMNIOCENTESIS
Amniocentesis was introduced in the 1930s as a diagnostic aid for placental localization by amniography.19 It gained widespread acceptance as a technique in the prenatal diagnosis of genetic diseases in the 1950s, after successful reports of amniotic fluid analysis in cases of Rh isoimmunization.20,21,22
In 1956, Fuchs and Riis23 demonstrated the feasibility of fetal sex determination by examining X-chromatin bodies in amniotic fluid cells. The ability to culture amniotic fluid cells in tissue culture and to acquire sufficient viable cells for karyotype analysis and biochemical studies was demonstrated in 1966.24 A partial list of conditions that lend themselves to prenatal diagnosis by amniocentesis is found in Table 3; all of these disorders have ocular manifestations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree