6.2 Diffuse Swellings
6.2.1 Acute Diffuse Swellings
The most common cause of acute diffuse facial swellings is acute infection of the upper jaw, which results from apical infection or after tooth extraction. Pain is marked, temperature is high, the swelling is diffuse, and edema may close the eyes. Other causes include furunculosis (multiple face furuncles), angioneurotic edema (Fig. 6.1), and recurrent erysipelas. The latter causes repeated attacks of swelling of the face mainly the upper lip. The rosy red color, absence of lymphadenopathy, raised margins with peripheral vesicles, and desquamation help in diagnosis.
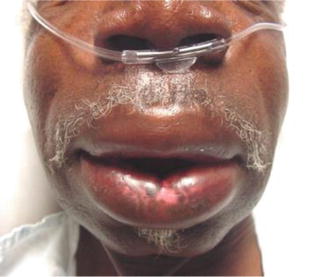
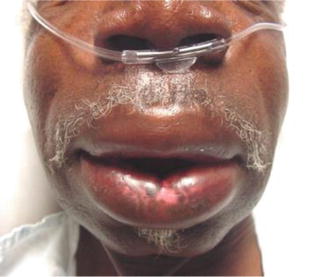
Fig. 6.1
Angioneurotic edema causing diffuse swelling in the face
6.2.2 Chronic Diffuse Swellings
Chronic diffuse facial swellings usually result from diffuse hemangioma (hemangiomatosis) or plexiform neurofibroma (neurofibromatosis).
6.2.2.1 Diffuse Hemangioma
There are two major categories of vascular anomalies: tumors and malformations [1]. Vascular tumors are endothelial neoplasms characterized by increased cellular proliferation. Hemangioma is the most common and is almost exclusive to infants. Vascular malformations, on the other hand, are the result of abnormal development of vascular elements during embryogenesis and fetal life. These may be single-vessel forms (capillary, arterial, lymphatic, or venous) or a combination. Vascular malformations do not generally demonstrate increased endothelial turnover. History and physical examination can distinguish between vascular tumors and vascular malformations with a diagnostic accuracy of over 90 % [2].
6.2.2.2 Plexiform Neurofibromas (PNF)
Plexiform neurofibroma (PNF) is a rare type of generalized neurofibromatosis, which occurs due to overgrowth of neural tissue in the subcutaneous (SC) tissue [3, 4]. Such tumors are generally present at birth and often progress slowly during early childhood. The lesions can occur anywhere along a nerve and may appear on the face [4], orbit, and globe [5] and frequently involve the cranial and upper cervical nerves [6]. The condition results in functional disability and disfigurement by pulling down of important structures [7, 8]. Complications include bleeding from trauma, neurological deficits, and psychological disturbance [4], in addition to malignant transformation in 4–5 % of cases [8].
Diagnosis on clinical basis is not difficult; however, MRI evaluation of tumors involving the head and neck region can help in determining the local infiltration and precise anatomy.
Surgical management remains the mainstay of therapy, but it is limited in facial PNFs by the infiltrating nature of these tumors, inherent operative morbidity, postoperative functional disturbances [9, 10], and the high recurrence rate that may reach 20 % after complete resection and 45 % after incomplete resection [11]. Surgical interventions are thus commonly postponed to as long as possible [12] and should be undertaken only after giving due consideration to the possible psychological and social benefits. Periodic clinical examination and MRI evaluation are required for about 2 years for timely detection and repeat surgery to achieve further correction. No chemotherapeutic agent has yet been identified that reduces the size of these tumors [13].
6.3 Localized Swellings
6.3.1 Cystic Swellings
6.3.1.1 Sebaceous Cyst
It is very common in the face of young adults with acne vulgaris but may also occur in the elderly (Fig. 6.2). It is often multiple and is like a sebaceous anywhere else. Treatment is by surgical excision.
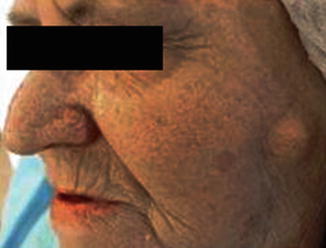
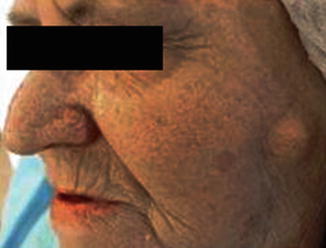
Fig. 6.2
A single sebaceous cyst in the left cheek of an 81-year-old lady
6.3.1.2 Dermoid Cyst
It occurs at the lines of fusion of the five parts constituting the face. The outer canthus is the most common site. Other sites are rare and include the inner canthus, at the fusion of the mandibular and maxillary processes, and in the midline of the chin. Treatment is also by surgical excision.
6.3.1.3 Hemangioma
Capillary, cavernous, or mixed hemangiomas may occur in the skin and SC tissue. Early onset, bluish coloration, and compressibility are characteristic. Propranolol is the treatment of choice for facial hemangiomas or those that affect function. Injectable or oral steroids and laser therapy remain viable treatment options as well [14].
6.3.1.4 Lymphangioma
Lymphangiomas are uncommon congenital malformations of the lymphatic system that are generally diagnosed during childhood and rarely seen in adults. It causes thickening of the tissues of the cheek, and clinically, it is translucent and does not empty on pressure. Management of this condition in the facial region is still challenging because they tend to infiltrate adjacent tissues, causing frequent recurrences. Radical surgery is the main line of treatment but should avoid the sacrifice of function or aesthetics of the patient [15].
6.3.1.5 Cystic Swellings of the Parotid Gland
Cystic parotid lesions are either bilateral, including Warthin’s tumor, benign lymphoepithelial cysts, sialocele, and Sjogren’s syndrome, or unilateral, including necrotic or infected lymph nodes (LNs) (for more details, refer to Chap. 3 “Surgery of the Salivary Glands”).
6.3.1.6 Cystic Swellings Around the Orbit
(a)
External angular (sequestration) dermoid cyst: The outer end of the eyebrow characteristically extends over the swelling which distinguishes it from a swelling of the lacrimal gland (Fig. 6.3). The skin is mobile over the swelling which is partly mobile on the underlying structures. There is evident indentation of bones beneath the swelling. It is no compressible, and its size does not increase on straining. Treatment is by excision.


Fig. 6.3
A right supraorbital dermoid cyst at the outer canthus
(b)
Inner angular dermoid cyst: It is less common than the external angular dermoid. It lies over the root of the nose, in a more or less central position.
(c)
Swellings of lacrimal glands: The lacrimal gland may be the seat of a tumor (similar to salivary gland tumors) or Mickulicz disease. Its position is more medial to the site of the external angular dermoid.
(d)
Swellings of the lacrimal sac:
Swellings of the lacrimal sac include dacryocystitis (inflammation of the lacrimal sac, which causes swelling below and medial to the inner canthus) and mucocele of the lacrimal sac, which results from blockage of the nasolacrimal duct and causes a cystic swelling between the root of the nose and the inner canthus, accompanied by lacrimation. There is usually a history of recurrent inflammation.
(e)
Mucocele of the frontal sinus: It results from frontonasal duct blockage and lies just above and medial to the inner canthus. If it enlarges more, it displaces the globe.
6.3.2 Solid Swellings
6.3.2.1 Keloid (Greek Crab’s Claw)
A keloid means hypertrophy and overgrowth of fibrous tissue extending beyond the original wound into normal tissues. It usually follows wounds, burns, vaccination marks, and tuberculous sinuses but may occur spontaneously. It occurs in certain sites more than others, such as the face, the neck, the ears, and over the sternum. It is also more common in darker races but less common in infants and old people. The incidence of keloid is known to increase in pregnant women and in patients with tuberculosis (TB) [16].
The lesion is elevated above the skin surface and is devoid of hair. It is unsightly, tender, and usually itchy, firm, and pinkish in color in its early states (Fig. 6.4), but later on, it becomes pale. It may give a clawlike processes and the margin is ill defined (Fig. 6.5). It should be differentiated from a hypertrophic scar, which results from excessive fibrous tissue formation, and is usually thick and reddish in color and may itch. However, unlike keloid, it is always confined to the scar, never gets worse after 6 months, and does not recur after excision [16].



Fig. 6.4
Keloid of the right side of the cheek of a 30-year-old lady

Fig. 6.5
Extensive keloid of the left side of the face extending down to the lateral side of the neck
Management of keloid is challenging as recurrence is very common particularly in chronic cases. The most effective treatment is superficial external beam radiotherapy (SRT), which can achieve cure rates of up to 90 %. In long-standing cases, excision and re-suturing whenever feasible, preceded, and followed by radiation may be required to achieve cure. Other therapeutic options include intralesional injection with a corticosteroid such as Kenalog, which aids in reduction of inflammation and pruritis, the use of silicone sheets, and shaving the keloid with resurfacing the area by a thin skin graft [17]. Cryotherapy or cryosurgery is easy to perform and has shown results with least chance of recurrence.
6.3.2.2 Lipoma
Lipoma of the face is a subcutaneous (SC) one and is similar to lipoma elsewhere. It is usually attached to the overlying skin by strands causing dimpling of the skin. It is freely mobile and soft, with lobulated surface and slippery edges.
6.3.2.3 Neurofibroma
Neurofibroma is rather common in the supraorbital region and the face. It may occur in the form of a firm nodule, fusiform in shape, along the course of a nerve, or it may present as a plexiform neuroma involving the skin and subcutaneous (SC) tissue. The skin may be redundant, overhanging, and pigmented causing severe disfigurement. Other neurofibromata and cafe au lait patches may be present (Neurofibromatosis) (Fig. 6.6).


Fig. 6.6
Neurofibromatosis (Note multiple neurofibromata and café au lait pigmentation)
6.3.2.4 Other Solid Swellings
Other solid swellings of the face are discussed in detail elsewhere in this book and include malignant skin tumors, swellings of the parotid gland, swellings of the preauricular LNs, and swellings of the jaw.
6.4 Ulcers of the Face
6.4.1 Classification
Ulcerative infective lesions | Ulcerating tumors | |
|---|---|---|
A. Nonspecific | B. Specific | |
1. Chronic nonspecific ulcer | 1. Tuberculosis (TB) | 1. Molluscum sebaceum |
2. Infected sebaceous cyst | 2. Syphilis ($) | 2. Basal cell carcinoma (BCC) |
3. Leishmaniasis | 3. Squamous cell carcinoma (SCC) | |
4. Leprosy | 4. Malignant melanoma | |
5. Actinomycosis | 5. Metastatic mass ulceration | |
6. Anthrax | 6. Infiltrating deeply seated tumor that invades and ulcerates the skin | |
6.5 Ulcerating Infective Lesions
6.5.1 Nonspecific Ulcers
6.5.1.1 Chronic Nonspecific Ulcer
A chronic nonspecific ulcer could either be of the exuberant type, which presents with a wartlike, soft, and granulating lesion that bleeds easily, or the flat type, in which the ulcer is painful, with an irregular margin, a floor covered with granulation tissue (GT), a firm base, and purulent or serous discharge. Persistence of the cause maintains its chronicity.
6.5.1.2 Infected Sebaceous Cyst
An infected sebaceous cyst is easily diagnosed by its long history, irregular edge, and floor covered with purulent exudate, in addition to the painful and firm base. In addition, hair follicle or punctum may be seen, and infected sebaceous-like material may come out on squeezing.
6.5.2 Specific Ulcers
6.5.2.1 Tuberculous (TB) Ulcers
Tuberculous ulcers are characteristically painful. The ulcer is common in the neck due to breakdown of LNs, in the maxillary region due to TB of underlying bone, and in the skin of the face due to lupus vulgaris. The outline of the ulcer is irregular and scarring may be present. The edge is undermined and bluish in color, with apple-jelly nodules (in lupus vulgaris) around it. The floor of the ulcer is pale and soft, covered with unhealthy granulation tissue, and the discharge is serous or watery.
6.5.2.2 Syphilitic ($) Ulcer
In primary syphilis, a chancre may occur in the face (lips, nose, or eyelids), surrounded by marked edema and associated with enlarged LNs. Swab examination will show the spirochetes and confirm diagnosis. In tertiary syphilis, a gummatous ulcer occurs in the frontal region. It is painless and has a serpiginous margin, punched-out edges, and a wash-leather floor. The skin around the ulcer shows pigmentation and scarring. It is fixed to the bone and plain radiography will show bone sclerosis. Other stigmata of syphilis are usually present and Wassermann-reaction (WR) is positive.
6.5.2.3 Leishmaniasis (Oriental Sore)
An oriental sore presents with a slowly progressive, painless, ulcer that may occur anywhere in the face (exposed to mosquito bites). It may be raised above the surface and have a cauliflower-like appearance. Diagnosis is reached by microscopic examination, which shows “Leishmania donovani bodies.”
6.5.2.4 Actinomycosis
Actinomycosis, once thought to be a fungal infection, is currently known to be a bacterial one. It is characterized by multiple sinuses with sulfur-like granules (colonies of the organism) and diffuse dense fibrosis around the openings.
6.5.2.5 Anthrax
Anthrax affects mainly wool workers and horse workers. It presents as a localized, painful area of induration, with multiple sinuses, covered with yellow necrotic slough.
6.6 Ulcerating Tumors
6.6.1 Molluscum Sebaceum (Keratoacanthoma, KA)
Keratoacanthoma (KA) is a common low-grade skin tumor that is believed to originate from the neck of hair follicles [18]. It is commonly found on sun-exposed areas such as the face, forearms, and hands [19] and is unlikely to invade or metastasize. Many pathologists often label KA as “well-differentiated SCC, KA variant” [20], because about 6 % of KA manifests itself as SCC when left untreated [21], which mandates prompt and aggressive treatment [22].
The characteristic feature of KA is that it presents with a dome-shaped, symmetrical, ulcer with an umbilicated central hyperkeratotic core and surrounded by a smooth wall of inflamed skin (Fig. 6.7). Only when almost the entire lesion is submitted to histopathology can a true diagnosis of a KA be made. A shave biopsy is not recommended as it will often reveal only keratin fragments. This is especially important for facial and nasal KAs, as it allows the surgeon to treat the tumor with margin-controlled surgery and minimal tissue removal, like Mohs surgery. Recurrence after electrodesiccation and curettage is common.


Fig. 6.7
Left facial keratoacanthoma (Note the central hyperkeratotic core)
6.6.2 Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is a locally invasive carcinoma of the basal layer of the epidermis. It does not metastasize but still can kill by local infiltration. The deoxyribonucleic acid (DNA) of certain genes is often damaged in patients with BCC (mostly caused by exposure to light), which implicates that inheritance may be a factor.
6.6.2.1 Incidence
Approximately, 80 % of all skin cancers are BCCs. It usually occurs in elderly people (mostly >65 years – related to duration of exposure to UV light), affecting men more than women (2:1) probably due to increased recreational and occupational exposure to sun. It is more common in countries that have much bright sunlight and in fair-skinned people (e.g., Australia). Whites of Celtic ancestry have the highest risk for BCC. Incidence is low in dark-skinned individuals, Asians, and Hispanics.
6.6.2.2 Body (Anatomic) Distribution
Nearly, 70 % of BCCs occur on the head (most frequently on the face) [23, 24], 25 % on the trunk [25], and 5 % on other sites such as the penis [26], vulva [27, 28], or perianal skin. Very rarely, other organs are affected such as the prostate. On the face, the majority is found in the middle-third (bounded by a line joining the angle of the mouth to the ear lobule and a line from the outer canthus of the eye to the root of the helix), affecting mainly the lower eyelid, inner canthus, tip of the nose (Fig. 6.8), ala nasi, outer canthus, dorsum of the nose, glabella, and lastly the cheeks. Less commonly, BCC affects the lower and upper thirds; thus, the back of the ear (Fig. 6.9), upper eyelid, and lower lip are not commonly affected.



Fig. 6.8
BCC near the tip of the nose in a 42-year-old gentleman (Note the raised, rolled edge and dark pigmentation)

Fig. 6.9
Retroauricular BCC (uncommon site) in a 58-year-old lady (Note the inverted (rolled-in) edge of the ulcer and granulating floor)
Recent data (2007) indicate that after adjusting for surface area, BCC occurrence is greater than four times more likely on embryonic fusion planes than on other regions of the midface, which supports the possibility of an embryologic role for BCC pathogenesis [29].
6.6.2.3 Etiology
The exact etiology of BCC is unknown, but environmental and genetic factors are believed to increase the risk.
Radiation exposure
Sunlight, particularly chronic exposure, is the most frequent association with the development of BCC; risk correlates with the amount and nature of accumulated exposure, especially during childhood. A latency period of 20–50 years is typical between the time of ultraviolet (UV) damage and the clinical onset of BCC [30]. The skin can repair superficial damage, but the underlying cumulative damage remains, including DNA damage. The damage worsens with each successive sun exposure, causing a lifetime progression [31]. Wehner et al. (2012) in their systematic review and meta-analysis of 12 studies reported that indoor tanning was associated with a significantly increased risk of both BCC and SCC, particularly in those under the age of 25 years [32]. In another 2012 study, indoor tanning was strongly associated with early-onset BCC, particularly among women [33].
Gene mutations
Recent studies (2007) showed a high incidence of TP53 gene mutations in BCC, caused mainly by UV sunlight. However, genetic involvement has been demonstrated on chromosome 9 only in patients with familial basal cell nevus syndrome (Gorlin syndrome). Such mutation involves the patched (PTCH) gene, a tumor suppressor gene [34].
Immunosuppression
Organ transplant patients must be instructed to limit sun exposure because immunosuppression and sun damage may cooperate to cause skin cancer. The incidence of skin cancer is tenfold higher in transplant patients than in the general population. A modest increase in risk of BCC has also been noted in patients with AIDS.
Xeroderma pigmentosum
This is an autosomal recessive disease that results in the inability to repair UV-induced DNA damage. Characteristic features include pigmentary changes seen early in life, followed by the development of skin cancer (BCC, SCC, and malignant melanoma), corneal opacities, eventual blindness, and neurological deficits [35].
Other contributing factors
These include exposure to or contact with arsenic [28, 36], tar, coal, paraffin [37], and certain types of industrial oil. Basal cell carcinoma can also be associated with albiminism, scars (e.g., burn complications) [38], previous trauma [39], vaccinations, tattoos, or previous non-melanotic skin cancer [40], as well as alcohol consumption [41].
6.6.2.4 Related Syndromes
Nevoid BCC Syndrome (Gorlin’s Syndrome)
In addition to BCC, this autosomal dominant (AD) disorder can result in the early formation of multiple odontogenic keratocysts, palmoplantar pitting, intracranial calcification, and rib anomalies [42]. Other tumors can also occur such as medulloblastoma, meningioma, fetal rhabdomyoma, and ameloblastoma [41].
Bazex Syndrome
Features of Bazex syndrome include follicular atrophoderma (so-called ice pick marks, especially on dorsal hands), multiple basal cell carcinomas, and local anhidrosis (decreased or absent sweating) [31].
Rombo Syndrome
Rombo syndrome is an AD disorder characterized by BCC and atrophoderma vermiculatum, trichoepithelioma, hypotrichosis, milia, and peripheral vasodilatation with cyanosis [43].
6.6.2.5 Symptoms
Patients presenting with BCC often report a persistent nodule or ulcer (often multiple), with a central scab that repeatedly falls off and then reforms, giving the patient a false impression that it is benign and not important. As tumors most commonly occur on the face, patients often complain of disfigurement. It may cause itching. If neglected and becomes deep, it may cause pain and bleeding and may become infected. Large neglected rodent ulcer destroying one side of the face is nowadays, fortunately, rare. Patients often have a history of chronic sun exposure, including recreational sun exposure (e.g., sunbathing, outdoor sports, fishing, boating) and occupational sun exposure (e.g., farming, construction). Occasionally, patients have a history of exposure to ionizing radiation.
6.6.2.6 Physical Examination
Clinical presentation of BCC varies by type. Clinically, BCC could be categorized as being either superficial or penetrating. In the superficial type, there is a beaded, raised, or rolled-in edge (Fig. 6.10), a firm base, and a granulating floor with attempts of epithelization. The draining LNs are not enlarged. In the penetrating type, there is additional infiltration of deeper structures such as bone and cartilage.


Fig. 6.10
Nasal BCC of a 60-year-old lady (Note the raised, beaded, inverted (rolled-in) edge of the ulcer)
Regarding the color, the raised part of the lesion (i.e., the edge of an ulcer or the center of a nodule) is smooth, glistening, and transparent. This gives the impression that there are pearly white nodules of tissue just below the epidermis. These nodules also give the ulcer its typical “rolled edge.” The surface of the nodular type is covered by distinct blood vessels (telangiectases) which may give it a pink hue. The whole lesion may be colored (brown) by excess melanin, simulating a mole or melanoma (Fig. 6.11).


Fig. 6.11
BCC at the inner canthus of a 69-year-old gentleman (Note the dark-brown (blackish) coloration)
Basal cell carcinoma starts as a nodule that later ulcerates. The ulcer has a raised rolled-in edge but not everted. The center of the nodule can become large and look cystic (called cystic rodent ulcer). It is not cystic because it is solid and not fluctuant. The ulcer or nodule is usually small in size at presentation, but it can grow to a large size if neglected. The rolled edges are at first circular but later become irregular. An irregular raised edge around a flat white scar is sometimes called a “geographical or forest-fire BCC.” The base consists of the tissue into which the tumor is eroding (fat, muscle, bone, eye, etc.), covered with granulation tissue. The base is usually not tender.
Most BCCs are superficial and confined to the skin. However, neglected cases may erode deep into the face destroying the skin and bone and exposing the nasal cavity, air sinuses, and even the eye and brain (rare). Local LNs should not be enlarged (unless infected or transformed into a SCC). Early lesions are freely mobile; later they invade deeply and become fixed. The lesion grows slowly (0.5 cm in 1–2 years), is not painful, and does not itch.
6.6.2.7 Complications
Spread is usually by direct infiltration of muscles, cartilage, and bone (locally malignant), leading to significant local destruction and considerable disfigurement [44, 45]. Orbital invasion can cause diplopia, proptosis, and ophthalmoplegia. Any limitation in ocular movements and/or diplopia should be tested. The BCC rarely causes regional or distant metastasis, with the exception of the metatypical and basosquamous types. To evaluate for LN metastasis, particular attention should be taken to examine the parotid, posterior auricular, suboccipital, and upper cervical groups of LNs.
Secondary infection will cause the local LNs to become enlarged and tender. Hemorrhage may easily occur if the lesion is traumatized and may be severe due to erosion of a blood vessel by the growing ulcer.
Epitheliomatous transformation (into a SCC) may occur and is evidenced by the rapid growth of the lesion, everted edges at least in a part of the ulcer, extension of induration beyond the base of the ulcer, loss of the pearly white margin, enlargement of local LN(s) which may become hard and fixed, evidence of distant metastases, and finally, the characteristic histopathological features of SCC on biopsy.
6.6.2.8 Clinic-pathological Types of BCC
Several different clinic-pathological types of BCC exist, each with distinct biologic behavior.
Nodular (Noduloulcerative) BCC
Nodular BCC is the most common type, representing more the 60 % of BCCs. It presents as a round, pearly, flesh-colored papule with telangiectases (Fig. 6.12). As it enlarges, it frequently ulcerates centrally, leaving a characteristic raised, pearly, beaded, border with telangiectases. Most lesions are seen on the face, although the trunk and extremities also are affected.


Fig. 6.12
Nodular BCC presenting as a waxy, translucent papule with central depression and a few small erosions
Variants of Nodular BCC
•
Cystic BCC. It is an uncommon variant of nodular BCC that may be mistaken for inclusion cysts of the eyelid. Typically, a bluish-gray cyst-like lesion is observed. The cystic center of the tumor is filled with clear mucin that has a gelatin-like consistency. Often, the typical features of a nodular BCC are seen in addition to the cystic features.
•Pigmented BCC. It is another uncommon variant of nodular BCC with additional dark pigmentation from melanin deposition that imports a dark-brown or blue-black color. It may, therefore, be confused with malignant melanoma. However, it can be differentiated easily if a few basic rules are appreciated. Firstly, the pigment in a BCC is punctate, because it lies in islands of nevus cells, which have been left behind as the tumor infiltrates the skin; pigment in melanoma is more widespread and uniform. Secondly, the typical signs of a BCC (i.e., the rolled edge, telangiectases, and the central depression) can be observed (Fig. 6.13).

Fig. 6.13
Pigmented BCC simulating melanoma, in the face of a 64-year-old lady (Note the raised, beaded border)
•Keratotic BCC. It is a variant of nodular BCC and is usually clinically indistinguishable from nodular BCC histologically.
Infiltrative BCC
With this variant of BCC, the tumor infiltrates deeper into the dermis in thin strands between collagen fibers, making the tumor margins less clinically distinguishable. It may erode deeply into the underlying structures, known as “rodent ulcer” (ulcus rodens). Because of its growth pattern, electrodesiccation and curettage has a significantly higher recurrence rate as compared to nodular BCC. Mohs micrographic surgery is thus the treatment of choice.
Micronodular BCC
This type is rather rare and has the typical BCC distribution. It is firm in consistency, is not prone to ulceration, may appear yellow-white when stretched, and may have a well-defined border.
Morphea-Like (Fibrosing, or Sclerosing) BCC
Morphea-like BCC is an uncommon type of BCC accounting for nearly 10 % of lesions. The tumor cells induce a proliferation of fibroblasts within the dermis and an increased collagen deposition (sclerosis) that clinically resembles a scar. This tumor thus assumes an indurated, yellowish plaque with ill-defined borders over which the skin remains intact for a long period of time. The skin actually looks shiny and taut because of the intense fibroblastic response the tumor induces, giving its “scar-like” appearance (Fig. 6.14). It is more often initially overlooked than the nodular type. The margins of this form are difficult to identify because the tumor cells invade normal tissue well beyond the visible margin. It, therefore, requires a wider safety margin on excision than the typical BCC. Mohs micrographic surgery is the treatment of choice because recurrence is more likely with other treatment modalities.
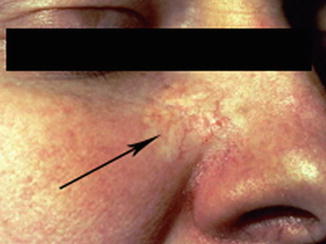
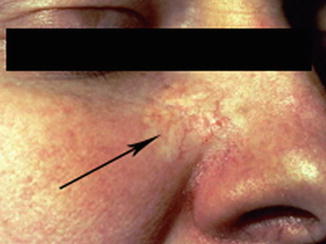
Fig. 6.14
A large, morphea-like (sclerosing) BCC on the right nasolabial fold (arrow)
Superficial BCC
Superficial BCCs are seen mostly on the upper trunk or shoulders (and not on the face). It grows slowly, has minimal tendency to invade surrounding tissues, and presents clinically as an erythematous, well-circumscribed patch or plaque, often with a whitish scale (Fig. 6.15). The tumor often appears multicentric, with areas of clinically normal skin between lesions. Numerous superficial BCCs may indicate arsenic exposure. Superficial BCC should be differentiated from psoriasis and eczema.


Fig. 6.15
Superficial BCC (on the trunk) showing erythema, scales, and a threadlike raised border
Gorlin Syndrome (Basal Cell Nevus Syndrome)
Gorlin syndrome (basal cell nevus syndrome) is an AD inherited condition, with the responsible gene located on 9q [46]. A feature of this syndrome is BCC. Multiple, often highly invasive, BCCs appear after puberty on the face, trunk, and extremities [47]. Other features (fortunately, uncommon) include mental retardation, congenital agenesis of the corpus callosum and medulloblastoma, odontogenic jaw cysts, bifid ribs and pectus excavatum, absent or undescended testes, mesenteric lymphatic cysts, palmar and plantar pits, ectopic calcification (particularly of the falx cerebri), as well as ocular and skeletal abnormalities such as hypertelorism, and shortening of the fourth and fifth metacarpals [48].
Other Types of BCC
Other types of basal cell carcinoma include the following:
1.
Polypoid (Pinkus tumor, fibroepithelioma). According to several studies, this tumor, which was considered to be a premalignant skin condition, must be considered as a fenestrated variant of BCC [49–51]. It occurs mostly in the back and consists of thin, anastomosing strands of basaloid cells in a prominent stroma.
2.
Basosquamous. This variant has the general configuration of a BCC, but contains also atypical squamous cells (squamatoid cells) and intermediate cells. It is more aggressive than typical BCC and has a metastatic potential.
3.
Geographical (forest-fire or field-fire variant). This variant is characterized by an advancing edge and a healing center.
4.
Metatypical BCC. This rare tumor is often aggressive, with an increased tendency for lymphatic and perineural spread. Histologically, nests and strands of cells mature into larger and paler cells, and peripheral palisading, if any, is less developed than in other types. Prominent stroma, prominent mitotic activity, and many apoptotic cells may be present.
5.
Infundibulocystic. This rare type, which resembles the keratotic variant, is usually found on the face. Nests are arranged in an anastomosing pattern and lack stroma. Many small, infundibular cyst-like structures with keratinous material are present. Melanin is sometimes present as well.
6.6.2.9 Diagnosis
Skin Biopsy
A skin biopsy is often required to confirm the diagnosis and determine the histological subtype of BCC. Most often, a shave biopsy is all that is required. However, in case of a pigmented lesion, an excisional or punch biopsy may be indicated to ensure that the depth of the lesion can be determined if it proves to be a malignant melanoma. A punch biopsy should be avoided if curettage is planned for final treatment.
Histologically, tumor cells typically resemble the basal cell layer of the epidermis or analogous cells of hair follicles, sebaceous or sweat glands. It spreads microscopically beyond the visible lesion. Characteristic features include palisade arrangement of columnar cells at the periphery, central mass of polyhedral cells, stroma of fibrous tissue and chronic inflammatory cells. Cystic spaces may be seen. Mitotic figures are very rarely observed and are usually few. Basal cell carcinoma is divided histologically into two categories; undifferentiated and differentiated. In undifferentiated BCC, there is little or no differentiation, the carcinoma is referred to as solid BCC, and this form includes pigmented BCC, superficial BCC, sclerosing BCC, and infiltrative BCC. On the other hand, differentiated BCC often has slight differentiation toward hair (keratotic BCC), sebaceous glands (BCC with sebaceous differentiation), and tubular glands (adenoid BCC). Noduloulcerative (nodular) BCC is usually differentiated.
Imaging
Given that BCC rarely metastasizes, laboratory and imaging studies are not commonly indicated in patients presenting with localized disease. Imaging studies may be necessary when involvement of deeper structures, such as bone, is clinically suspected. In such cases, CT scans or radiography may be utilized.
The use of ultrasonography (US) is controversial, because of the inadequate accuracy (20 %) in delineating malignant from benign lesions. Furthermore, the claims of reliable tumor sizing and depth of invasion, though promising, are still passionately debated. As an adjunct tool, laser Doppler may assist ophthalmologists in distinguishing between benign and malignant adnexal skin lesions and in establishing the tumor margin. In histologically documented BCC of the eyelid, cutaneous perfusion was significantly greater [52].
6.6.2.10 Differential Diagnoses
The list of lesions from which BCC should be differentiated is rather long and includes actinic keratosis, angiofibroma, Bowen disease, fibrous facial papule, malignant melanoma, keratoacanthoma (molluscum sebaceum), melanocytic nevi, psoriasis, sebaceous hyperplasia, and squamous cell carcinoma (SCC).
6.6.2.11 Staging
Since BCC rarely metastasizes, it is usually not staged, unless the cancer is very large and is suspected of metastasizing. Staging of BCC may be similar to that of SCC as follows:
Stage | Description |
|---|---|
0 | Cancer involves only the epidermis and has not spread to the dermis |
I | Cancer is <2 cm and has not spread to LNs or other organs |
II | Cancer is >2 cm but has not spread to LNs or other organs |
III | Cancer has spread to tissues beneath the skin (e.g., muscle, bone, cartilage) and/or to regional LNs but not to other organs |
IV | Cancer can be any size and has spread to other organs |
High-Risk Tumors
High-risk BCCs include recurrent or incompletely excised BCC; tumors with indistinct borders; lesions in high-risk (the H, or mask) areas, mainly the embryonic fusion planes; tumors with rapid growth or large size (>2 cm); and aggressive histological variants or types including sclerosing and basosquamous BCCs, with perineural, peri-appendageal, or perivascular invasion. Moreover, BCCs that develop in sites with previous radiation therapy or in immunosuppressed patients are also considered to be high-risk tumors.
6.6.2.12 Treatment
Approach Considerations
According to the 2011 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology, the goal of treatment of BCC and SCC is elimination of the tumor with maximal preservation of function and physical appearance. Management decisions should thus be individualized according to the patient’s particular risk factors and preferences. In the majority of cases, the treatment of choice is surgery, which varies according to cancer size, depth, type, and location [44, 45], in addition to patient’s age and general condition. Small and superficial BCC may respond to local therapy with chemotherapeutic and immune-modulating agents such as topical 5 % imiquimod and fluorouracil (5-FU) (most commonly used on smaller superficial non-facial BCC on the trunk and extremities) [53].
For tumors that are more difficult to treat (i.e., infiltrative, sclerosing, micronodular, and recurrent BCCs) or those in which sparing normal tissue is important, Mohs micrographic surgery should be considered.
For metastatic BCC, the 2011 NCCN guideline recommends clinical trials of systemic chemotherapy, particularly platinum-based combination therapy, which has been observed to produce useful, even complete, responses in a few patients. Clinical trials of investigational biologic modifiers such as hedgehog pathway inhibitors are also recommended.
Surgical Modalities
In nearly all cases of BCC, surgery is the recommended treatment modality [44, 45]. Techniques used include electrodesiccation and curettage, curettage without desiccation, curettage with laser ablation, laser ablation without curettage, excisional surgery, Mohs micrographically controlled surgery, cryosurgery, and immuno-cryosurgery [54].
Electrodesiccation and Curettage (E&C) [55]
Under local anesthesia, a curette is used firmly in multiple directions to vigorously scrape the tumor away from adjacent normal skin, followed by electrodesiccation. The entire process may be repeated 1–2 more times. It is an operator dependent, relatively blind technique in which the specimen cannot be examined for margin control, which limits its success in high-risk areas, such as the face and ears. Furthermore, the aggressive subtypes of BCC, such as sclerosing, infiltrating, micronodular, and recurrent tumors, are usually not friable, and therefore, E&C is unlikely to be successful. Healing by secondary intention often leads to atrophic, white scars that may not be satisfactory in aesthetically important areas. Finally, it is not suitable for patients with cardiac pacemakers. On the other hand, E&C is a simple and brief procedure (<5 min) and is effective in treating primary nodular and superficial BCC because these tumors tend to be friable and not embedded in fibrous stroma. The overall cure rate exceeds 90 % for low-risk BCCs. Small tumors (2–5 mm) have a 15 % recurrence rate (RR), whereas large tumors (>3 cm) have a 5-year RR of 50 %.
Curettage Without Dessication [54]
Under adequate local anesthesia, the tumor is scraped using a curette. This is often repeated two more times. It is a brief (<5 min) procedure, effective in treating primary nodular and superficial BCC, with cure rates as high as 95 %. Curettage alone is believed by some authors to have a better cosmetic outcome than that of E&C. However, it is neither widely accepted nor commonly performed, and it has the same disadvantages of E&C.
Curettage with Er:YAG Laser Ablation
After curettage, the newly formed ulcer is then ablated, along with a narrow (<1 mm) margin of adjacent epidermis using Er:YAG laser. This is often repeated two more times. This brief (<5 min) method is also effective in treating primary nodular and superficial BCC, with a 95 % cure rate, and is believed by some authors to have a better cosmetic outcome than does E&C, though with similar limitations and disadvantages.
Laser Ablation Without Curettage
A carbon dioxide laser is applied superficial BCC (most frequently) and nodular BCC. This procedure may be considered when a bleeding diathesis is present. It provides a bloodless field, minimal postoperative pain, and good cosmetic appearance without scar formation [56, 57]. With the recent devices, the reported RR went down from 50 to 3 % [58]. However, this procedure has been studied less than other methods, and a great variance in RR has been reported. Hypopigmentation may develop, which may not be apparent for 1 or more years.
Surgical Excision
This method can usually be performed in an ambulatory setting and provides the pathologist with a specimen to examine the tissue margins via routine paraffin processing or using frozen sections. Healing time is generally shorter with sutured closure than with granulation, and cosmesis compares favorably with that of curettage. The cure rate is also as high as 95 % [59].
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


