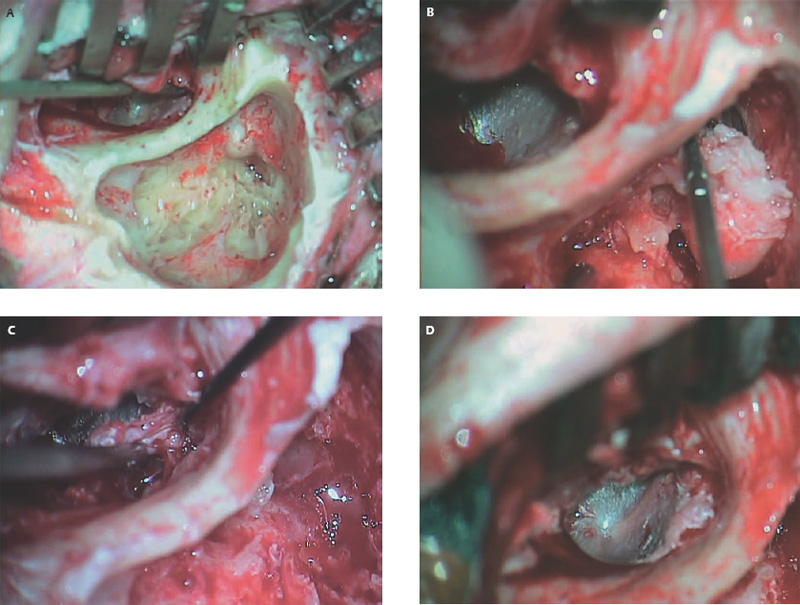
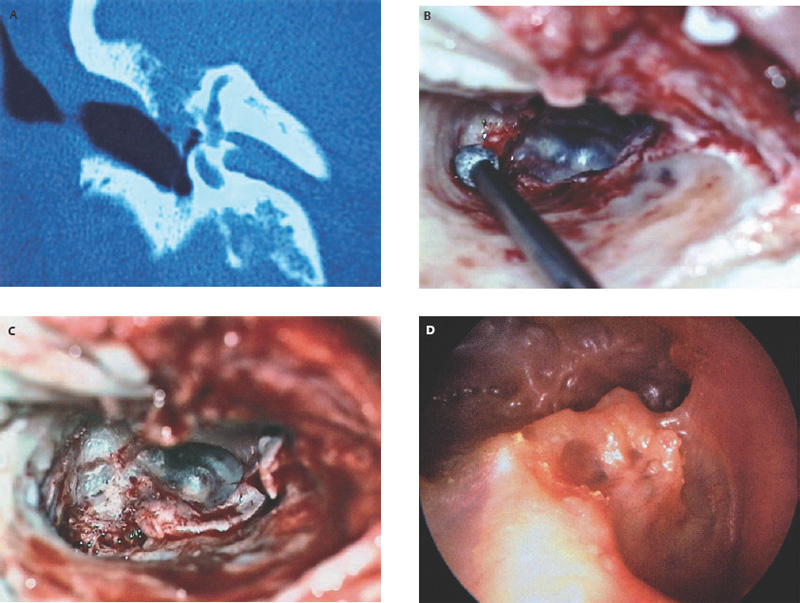
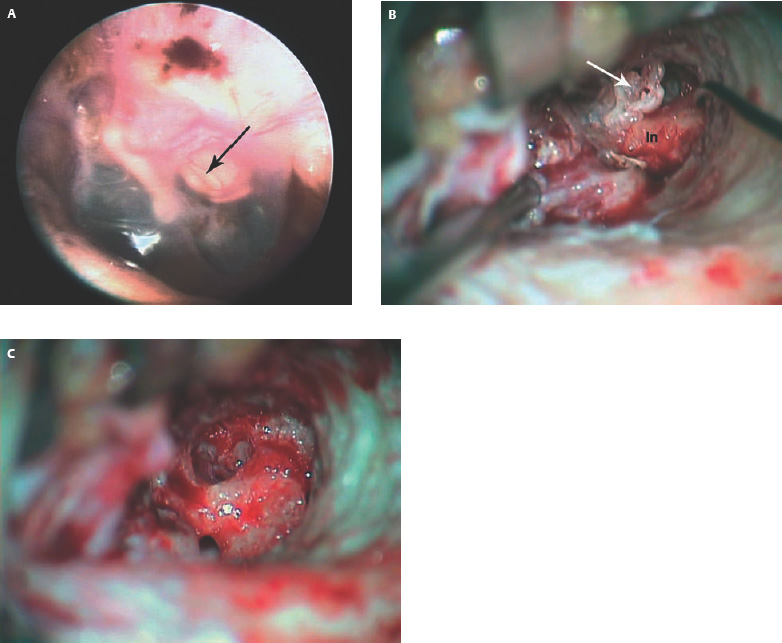
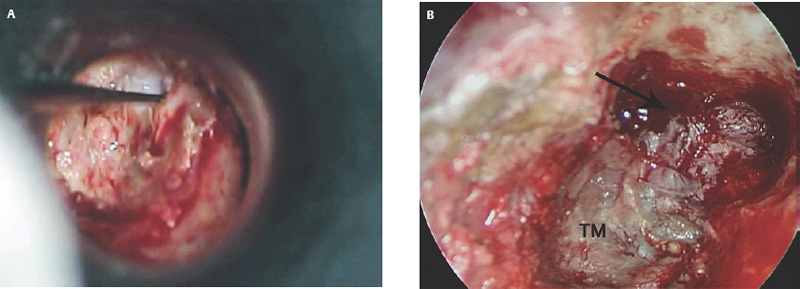
7 Situations That Arise at Surgery: Hearing Issues This chapter and the previous one address the unique situations that arise during cholesteatoma surgery. The prior chapter dealt with anatomical factors that confront surgeons. The current chapter deals with issues related to hearing. The preservation or restoration of hearing function is the second key goal of cholesteatoma surgery, and this is generally subservient to the complete removal (or exteriorization) of the disease. However, there are certain instances in which the hearing status will be an important issue in surgical timing and surgical decision making. These clinical instances are addressed in this chapter, and include the intact ossicular chain, cholesteatoma in the better-hearing ear, bilateral cholesteatoma, and cholesteatoma developing in an only hearing ear. Occasionally, the surgeon encounters an intact ossicular chain in the presence of cholesteatoma. It is tempting in these cases to try to maintain ossicular continuity in the interest of hearing preservation, but the surgical management should never compromise the complete removal of the disease. Good hearing outcomes can usually be expected even when the ossicular chain has to be reconstructed, and especially when the stapes superstructure can be preserved. On the other hand, leaving residual disease will eventually require additional surgery and lead to erosion of the ossicles, making long-term hearing preservation unlikely. When abundant inflammation is found at surgery, a normal hearing outcome is unlikely, even if the ossicular chain is preserved. The preoperative hearing level does not correlate with the location and size of the cholesteatoma. Normal preoperative hearing is occasionally seen in cases with ossicular erosion because the cholesteatoma itself may conduct sound efficiently. In these cases, patients may be disappointed if they have postoperative hearing loss despite an otherwise good surgical outcome (Fig. 7.1). Conversely, preoperative hearing loss can occur in the presence of an intact ossicular chain because the cholesteatoma or associated inflammation impedes the conduction of sound. Preserving the ossicular chain does not routinely lead to normal hearing in these cases.1,2 When an intact ossicular chain is found in the presence of normal preoperative hearing, the desire to maintain good hearing may conflict with the need to remove all the disease. Often the cholesteatoma can be removed without interrupting the ossicular chain, but this does not always result in normal postoperative hearing. In our series of cholesteatomas in normal-hearing ears, 72% had an intact ossicular chain, and ossicular continuity could be maintained in three fourths of these cases. Seventy-eight percent of patients with intact ossicular chains achieved hearing preservation to within 7 dB at the initial audiogram, but this decreased to 61% long term.1 In contrast, hearing preservation after ossicular reconstruction was 88% short term and 75% maintained long-term good outcomes. Reasons for long-term hearing decline include fibrosis, retraction, and disease recurrence. An intact ossicular chain is often encountered in cases of congenital cholesteatomas, acquired cholesteatomas confined to the middle ear, or attic cholesteatomas limited to the Prussak space. Congenital cholesteatomas, if they are detected early, can usually be removed without disrupting the integrity of the eardrum or ossicular chain, and a normal hearing result can be maintained (see Chapter 9). Middle ear cholesteatomas can be associated with an intact ossicular chain if they are small and attached to the tympanic membrane or if they grow posteriorly and avoid the incus and stapes. In these cases, surgery can be done with ossicular preservation, but re-retraction can compromise the long-term hearing. Attic cholesteatoma confined to the Prussak space can often be removed with ossicular preservation. Larger epitympanic cholesteatomas can also be handled this way if they spread posteriorly along the plane lateral to the incus (Fig. 7.2A–D). If disease extends more superiorly into the epitympanum but remains lateral to the incus and malleus, a Bondy mastoidectomy can be performed and the integrity of the ossicular chain preserved. Posterior epitympanic cholesteatoma usually envelops the incus, necessitating removal of the incus. Preserving the incus should be done very selectively in these instances because of the higher likelihood of residual disease. The endoscope may be helpful in assessing the completeness of cholesteatoma r emoval in these cases.3 Cholesteatoma usually occurs unilaterally and a less-than-perfect hearing outcome can be accepted when one good ear remains. However, when there is hearing loss in the opposite ear, either from cholesteatoma or from an unrelated cause, hearing preservation is more crucial. The choice of surgical approach, and, indeed, the decision to operate at all, may be critical to the outcome. Cholesteatoma occurs bilaterally in at least 8% of cases.4 The majority of cases present simultaneously, but some will present sequentially.5 When cholesteatoma affects both ears, patients will be subjected to multiple surgical operations, and the hearing outcome may be poor.5,6 Complete disease removal with the lowest possible chance of recurrence is therefore paramount, and a canal wall down or Bondy approach will achieve these goals in most cases when the disease begins in the attic. Hearing preservation has greater significance in bilateral than in unilateral cases, and in most instances performing a canal wall down procedure will not introduce a hearing penalty.7 In cases of middle ear cholesteatoma, a tympanoplasty approach will be used, and primary ossicular reconstruction can be undertaken. Obtaining a dry, stable ear is an important goal when a hearing aid will be needed. A bone-anchored cochlear stimulator (BAHA Cochlear Americas, Centennial, CO)8 or even a cochlear implant may be considered in certain instances. A few cases are presented that illustrate the decision-making process when cholesteatoma occurs in a better-hearing ear. A 38-year-old male patient complained of progressive hearing loss in the right ear without drainage. He had undergone cholesteatoma surgery in the left ear 8 years earlier, with a poor hearing outcome. Examination revealed a dry attic retraction with squamous debris on the right side, and a canal wall down mastoidectomy on the left side with a small, dry cavity. Audiometry revealed bilateral conductive hearing loss, 35 dB on the right and 50 dB on the left. Computed tomography (CT) revealed a poorly developed mastoid on the right side with soft tissue density in the attic and antrum, enveloping the ossicles (Fig. 7.3A). The procedure is done through a postauricular approach. Working through the ear canal with a diamond burr, the attic is opened first to identify the tegmen tympani laterally near the outer cortex. The tegmen is then followed medially toward the epitympanum. The scutum is thinned down to an eggshell and then removed with a curette to avoid vibrational trauma from the drill to the ossicles. The atticotomy is enlarged back to the antrum, again by following the tegmen posteriorly (Fig. 7.3B,C). The goal is to completely exteriorize the cholesteatoma sac. As drilling progresses, a round, beveled cavity is created. In a sclerotic ear, the surgeon can use a diamond burr to contour the bone to create a cavity of manageable shape and size. This requires beveling or saucerizing the cortical bony edges and lowering the facial ridge to the level of the fibrous annulus. It is possible to do this without separating the annulus or entering the middle ear. In sclerotic mastoids, the mastoid tip is usually not developed and does not need to be opened. The resulting surgical exposure allows complete removal of the disease under direct vision. This can be done without removing the incus or disrupting the incudostapedial joint, if the disease has not involved these structures. Closure of the cavity is done by draping the conchomeatal flap along the sinodural angle; fascial grafting of the medial attic wall is optional. The postoperative appearance is a compact cavity with an intact tympanic membrane (TM), and the attic is exteriorized (Fig. 7.3D). This has a low chance of recurrence or postoperative drainage. The hearing results are generally very good. The compact cavity permits the use of a hearing aid without fear of drainage or maceration. The Bondy operation is not suitable for cases of middle ear cholesteatoma. An illustrative example is a young man who had a previous canal wall down mastoidectomy for large cholesteatoma in the right ear that resulted in a dry cavity, but with a large conductive hearing loss. Second-stage ossicular reconstruction was unsuccessful because of middle ear fibrosis. The patient returned 1 year later with hearing loss and a single episode of drainage from the opposite ear. Examination revealed a cholesteatoma sac in the left middle ear (Fig. 7.4A). The disease was removed via transmeatal approach, raising a tympanomeatal flap and performing a limited atticotomy until sufficient exposure was gained. The scutum was reconstructed with tragal cartilage, and the hearing remained normal. After 5 years, the patient developed a recurrence beneath the cartilage graft. This was reexcised via a transmeatal approach. Figure 7.4B shows the middle ear disease traveling lateral to the incus to the Prussak space; this was removed completely, with mirror confirmation (Fig. 7.4C) and the scutum again closed with tragal cartilage. The patient maintained normal hearing after the revision procedure after 8 more years of follow-up. Simultaneous bilateral cholesteatoma presents a challenge. Generally one ear will be more symptomatic, with active drainage and worse hearing, and this ear should be operated on first. The less symptomatic ear can be dealt with in a staged fashion, once the first ear heals and is stable. If the second side is the better-hearing ear, it may be tempting to defer surgery as long as possible, or the patient may not wish to have the second operation, but this may be just delaying the inevitable. If the cholesteatoma grows or becomes infected it may compromise the hearing in the better ear and make the ossicular reconstruction more difficult. Some case examples follow. A 65-year-old man presented with refractory bilateral chronic ear drainage for 3 years. The right ear had copious purulent drainage and squamous material emerging from the attic; the left ear had a small attic retraction with moderate drainage. CT showed bilateral compact mastoids with soft tissue densities and erosion of the lateral semicircular canal on the right. Audiometry showed severe mixed hearing loss in the right ear and moderately severe loss on the left. He underwent right radical mastoidectomy first, because this was the more problematic and poorer-hearing ear, with the plan of performing staged surgery on the left ear at a later date. At surgery, an infected cholesteatoma was removed, and a lateral semicircular canal fistula was identified, unroofed, and sealed with periosteum. Cultures yielded Pseudomonas. Postoperatively he developed an anacoustic ear and vertigo that resolved slowly despite treatment with intravenous (IV) antibiotics. Four months later, he developed right facial paralysis. He was hospitalized for presumed Pseudomonas osteitis and given IV imipenem. The facial paralysis, imbalance, and otorrhea resolved completely, but profound sensorineural hearing loss remained. The left ear continued to drain intermittently, even during IV antibiotic therapy. Pseudomonas was also confirmed by culture. It was decided that surgical treatment could no longer be avoided. Because this was now an only hearing ear, a modified radical mastoidectomy was performed through an endaural approach (Fig. 7.5A,B). The goal was to do the least invasive operation that would control the disease, minimize the risk of further hearing loss, and minimize the need for postoperative packing. The ear healed well, with an intact tympanic membrane and an open attic-antral cavity. Because he received limited benefit from a hearing aid, a bone-anchored cochlear stimulator (BAHA, Cochlear Americas, Centennial, CO) was later implanted on the right side. The patient was very happy with the hearing that this afforded him, and both ears have remained dry and stable. A 48-year-old man presented with sudden sensorineural hearing loss in the right ear and failed to recover any hearing despite treatment with oral steroids, antivirals, and diuretics. His final hearing level was 80 dB PTA, with poor speech discrimination, hyperacusis, and distorted hearing with amplification. He had a history of chronic otitis media in his left ear and had a posterior pars tensa retraction pocket with a natural myringostapediopexy. His hearing was normal on the left side. He had intermittent otorrhea from the left ear that would cause a decline in hearing. The problem cleared quickly after the use of antibiotic drops. Over time, the episodes of otorrhea increased in frequency, and the hearing loss became more persistent. Endoscopic exam of the ear revealed a deep retraction pocket in the attic in addition to the middle ear (Fig. 7.6). There was pus but no squamous debris present. CT revealed focal thickening of the tympanic membrane in the middle ear and in the attic. The patient developed a retraction pocket cholesteatoma in his better-hearing ear. The opposite ear was not aidable. The remaining options include continued conservative management or surgical treatment. He was advised to have surgery because of the progressive nature of the disease and because of the persistence of infection. He delayed his decision to have surgery for fear of losing more hearing. In this case, a Bondy operation would take care of the disease in the attic but not the middle ear. A cartilage tympanoplasty is desirable for the posterior pars tensa retraction, but it would be difficult to perform without separating the myringostapediopexy and risking postoperative hearing loss. The patient has chosen to temporize and has avoided further episodes of otorrhea by exercising strict dry ear precautions. There is no guarantee that he will develop disease progression that will make surgery unavoidable in the future. Hearing is an important issue in cholesteatoma surgery and one that affects surgical decision making. When an intact ossicular chain is encountered, it can sometimes be preserved, but complete removal of the disease must take precedence over preserving ossicular continuity. When cholesteatoma occurs in the better-hearing ear or in an only hearing ear, the surgical strategy must take hearing outcome into account, and a Bondy procedure is favored when appropriate. In cases of bilateral cholesteatoma, the more symptomatic ear is operated on first, again considering the eventual hearing outcome when planning the surgical strategy. 1. Smouha EE, Javidfar J. Cholesteatoma in the normal hearing ear. Laryngoscope 2007;117 (5):854–858 2. Sakagami M, Seo T, Node M, Fukazawa K, Sone M, Mishiro Y. Cholesteatoma otitis media with intact ossicular chain. Auris Nasus Larynx 1999;26 (2):147–151 3. Tarabichi M. Endoscopic management of limited attic cholesteatoma. Laryngoscope 2004;114 (7):1157–1162 4. Edelstein DR, Parisier SC. Surgical techniques and recidivism in cholesteatoma. Otolaryngol Clin North Am 1989;22 (5):1029–1040 5. Lin V, Daniel S, James A, Friedberg J. Bilateral cholesteatomas: the hospital for sick children experience. J Otolaryngol 2004;33 (3):145–150 6. Vartiainen E. Fate of patients with bilateral cholesteatoma. Am J Otolaryngol 1993;14 (1):49–52 7. Murphy TP, Wallis DL. Hearing results in pediatric patients after canal-wall-up and canal-wall-down mastoid surgery. Otolaryngol Head Neck Surg 1998;119 (5):439–443 8. Wazen JJ, Spitzer J, Ghossaini SN, Kacker A, Zschommler A. Results of the bone-anchored hearing aid in unilateral hearing loss. Laryngoscope 2001;111 (6):955–958
♦ Intact Ossicular Chain

♦ Cholesteatoma in the Better-Hearing Ear
Bilateral Cholesteatoma Presenting Sequentially
Bilateral Cholesteatoma Presenting Simultaneously
Cholesteatoma Developing in an Only Hearing Ear

♦ Conclusion
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


