CHAPTER 24 Reconstruction of Facial Defects
Most facial defects result from ablation of cutaneous malignancies, and most cases can be repaired by primary wound closure or with a local cutaneous or musculocutaneous flap. Because the topic of facial reconstruction is extremely broad and complex, this chapter discusses only local flaps and grafts in the repair of facial cutaneous defects with the occasional appropriate reference to the repair of skeletal deficiencies. Other publications better address the use of regional flaps in facial reconstruction.1–3
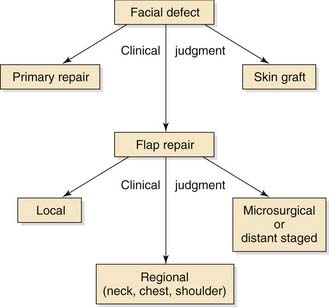
The face can be divided into aesthetic facial units, which include the forehead, cheeks, eyelids, nose, lips, auricles, and sometimes the scalp. Reconstruction of some of these areas of the face is discussed elsewhere in this textbook. A multitude of different flaps and grafts can be used to repair a given facial defect; thus several techniques for repair of a given aesthetic facial unit are discussed. The algorithm in Fig. 24-1 displays an approach for analyzing and developing a management plan for surface defects of the face and neck. The selection of a specific flap depends on the location and size of the defect and the intrinsic properties of the flap. Larger defects of the face and neck may be difficult to resurface with local flaps without considerable impairment in form or function. In such circumstances, the surgeon should select a regional flap or skin graft that might be aesthetically less pleasing but will provide a functional repair. These decisions are determined by clinical judgment. The greater the experience of the surgeon, the better will be the clinical judgment.
Classification of Local Flaps
Several methods are used to classify cutaneous flaps4,5: (1) by arrangement of their blood supply (e.g., random vs. arterial); (2) by configuration (e.g., rhomboid, bilobe); (3) by location (e.g., local, regional, distant); and (4) by the method of transferring the flap. Local cutaneous flaps are designed immediately adjacent to or near the location of the defect. When classified by method of transfer (Box 24-1), local flaps are divided into pivotal, advancement, and hinged categories. A fourth method of tissue movement is microsurgical, although this method does not apply to local flaps. In reality, most local flaps are moved through a combination of pivoting and advancement. For example, most pivotal flaps are aided in tissue movement by using the intrinsic elasticity of the flap through stretching (advancement). Thus surgeons often speak of combined mechanisms of tissue movement, such as advancement rotation flap. For classification purposes, however, the major mechanism of tissue transfer should dictate the term given to describe a particular flap, unless both mechanisms are of approximately equal importance, in which case the terms describing both mechanisms should be used.
Pivotal Flaps
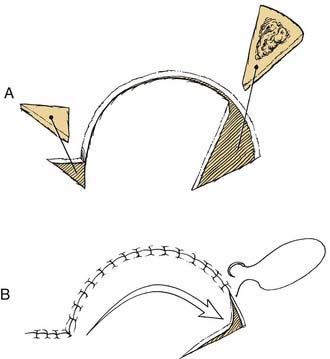
The three types of pivotal flaps are rotation, transposition, and interpolated (see Box 24-1). All pivotal flaps are moved toward the defect by rotating the base of the flap around a pivotal point. Except with island axial flaps, which have been skeletonized to the level of the nutrient vessels, the greater the degree of pivot, the shorter the effective length of the flap (Fig. 24-2). This is because the pivotal point is fixed in position and the base of the flap is restricted when pivoting around this point because of the development of a standing cutaneous deformity (dog ear). A pivotal flap should be designed to account for this reduction in effective length which may be as much as 40% with flaps that are pivoted through an arc of 180 degrees.
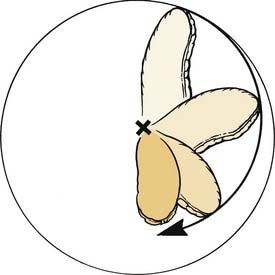
Figure 24-2. The effective length of a pivotal flap moving through an arc of 180 degrees is reduced 40%.
(Adapted from Gorney M. Tissue dynamics and surgical geometry. In: Kernakian DA, Vistnes LM, eds. Basic Concepts of Reconstructive Surgery. Boston: Little, Brown; 1977.)
Rotation Flaps
Rotation flaps are pivotal flaps that have a curvilinear configuration. They are designed immediately adjacent to the defect and are best used to close triangular defects (Fig. 24-3). Rotation flaps are usually random in their vascularity but, depending on the position of the base of the flap, may be axial. Because a rotation flap has a broad base, its vascularity tends to be reliable. When possible, the flap should be designed to be inferiorly based, which promotes lymphatic drainage and reduces flap edema. Rotation flaps are useful in repairing medial cheek defects located near the nasofacial sulcus or nasal sidewall. The curvilinear border of the flap can often be positioned along the infraorbital rim, which represents an important border of aesthetic units (eyelid and cheek). Positioning the incision for the flap along this border enhances scar camouflage.
Large rotation flaps are particularly useful for reconstruction of sizable posterior cheek and upper neck defects. Large medial, inferiorly based rotation flaps are a flexible means of transferring large amounts of tissue from the remaining cheek and upper cervical regions. Incisions for the flap are placed in a preauricular crease and can extend for some distance along the anterior border of the trapezius muscle to facilitate rotation of upper cervical skin toward the area of the posterior cheek. A Z-plasty at the base of the flap facilitates closure of the secondary defect. Chin reconstruction can often be readily accomplished with rotation flaps, occasionally using two flaps to optimize the use of the aesthetic border of the submental crease to camouflage incisions. Smaller rotation flaps can also be used for repair of defects located in the glabellar area. Because rotation flaps are less dependent on tissue elasticity for movement than most local flaps, they are particularly useful for scalp defects because scalp skin is quite inelastic. In addition, curvilinear configuration of rotation flaps adapts well to the spherical shaped cranium. Thus scalp defects in general are best reconstructed with one or more rotation flaps. A rotation scalp flap must be quite large relative to the size of the defect, with the width of the pedicle being twice the width of the defect.6
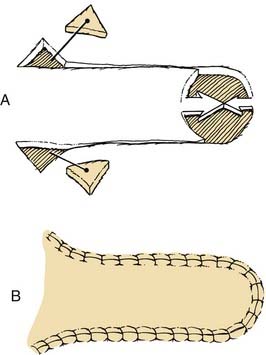
Transposition Flaps
In contrast to rotation flaps, transposition flaps have a linear axis (Fig. 24-4). Both are pivotal flaps moving around a pivotal point. A transposition flap can be designed similar to a rotation flap so that a border of the flap is also a border of the defect. However, it may also be designed with borders that are removed from the defect, with only the base of the flap contiguous with the defect. The ability to construct a flap at some distance from the defect with an axis that is independent of the linear axis of the defect is one of the greatest advantages of transposition flaps. This advantage enables the surgeon to recruit skin at variable distances from the defect, selecting areas of greater skin elasticity or redundancy. In addition, the ability to select variable sites for harvesting a flap ensures that the donor site scar by its location and orientation will best be camouflaged.
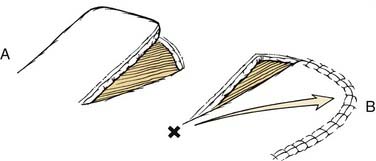
Figure 24-4. A, Transposition flaps have a linear configuration. B, The flap turns about a pivotal point at the base.
(A, Adapted from Baker SR, Swanson N. Local Flaps in Facial Reconstruction. St. Louis: Mosby; 1995.)
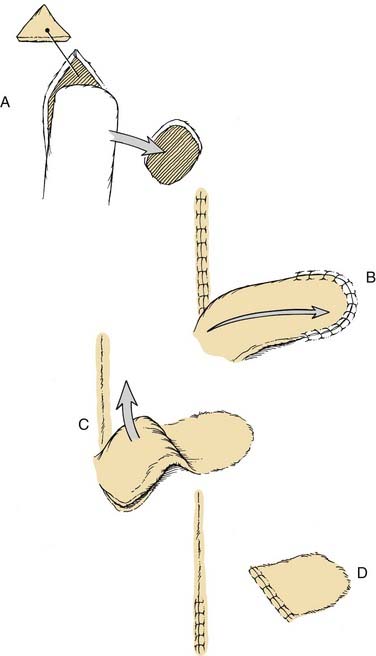
Interpolated Flaps
The interpolated flap is a pivotal flap that has a linear configuration, but it differs from transposition flaps in that its base is located at some distance from the defect (Fig. 24-5). Thus the pedicle must pass over or under intervening tissue. If the pedicle passes over intervening tissue, the flap should subsequently be detached in a second surgical procedure. This is perhaps the greatest disadvantage of these flaps. On occasion, the pedicle can be de-epithelialized or reduced to subcutaneous tissue only and brought under the intervening skin as an island flap to allow a single-stage reconstruction.
Common interpolated flaps used in the repair of facial defects are the vertically oriented midforehead flaps, which include median and perimedian flaps.7 These flaps are highly effective in reconstruction of the midface because of their excellent vascularity and because their skin color and texture superbly match the skin of the nose. The high success rate, reliability, and popularity are primarily the result of a dependable axial blood supply. Based on the supratrochlear artery and its anastomoses to surrounding vessels, midforehead flaps are axial flaps with excellent vascularity that can be transferred without delay. The excellent vascularity allows for the incorporation of cartilage or tissue grafts, which can then act as support structures or lining tissue for nasal reconstruction. Careful removal of muscle and subcutaneous fat from the distal portion of a midforehead flap makes it thin, pliable, and easily contoured to fit any defect of the midface. The frontalis muscle and fascia are included with the distal flap when more stiffness and bulk are required to fit defects of greater depth.
The close proximity of forehead skin to the midface provides a source of skin with excellent color and texture match to the central face. Modern use of the midforehead flap has been expanded beyond nasal reconstruction to include any soft tissue defect of the midface that the flap can be designed to reach.8 Defects of the medial canthal region, upper and lower eyelids, medial cheek, melolabial region, and upper lip can be repaired with midforehead flaps. These flaps can also be used in combination with other flaps for the reconstruction of complex facial defects; for example, a midforehead flap can be combined with a scalping flap for total nasal reconstruction.
Advancement Flaps
Unipedicle Advancement Flap
A unipedicle advancement flap is created by parallel incisions that allow the tissue to “slide” in a single vector toward a defect (Fig. 24-6). The movement is in one direction, and the flap advances directly over the defect. As a consequence, the flap should be developed adjacent to the defect, and one border of the defect becomes a border of the flap. Repair with an advancement flap involves primary and secondary tissue movement. In primary movement, the incised flap is pushed or pulled forward by stretching the skin. Secondary movement of surrounding skin and soft tissue immediately adjacent to the defect occurs in a direction opposite the movement of the advancing edge of the flap. This secondary movement may help in repair by providing less wound closure tension, or it may be detrimental, displacing nearby facial structures.
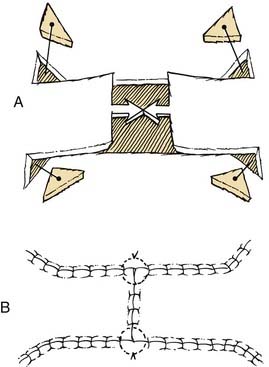
Complete undermining of the advancement flap, as well as of the skin and soft tissue around the pedicle, is important to enhance tissue movement. Standing cutaneous deformities are created with all advancement flaps and may require excision. Excision of standing cutaneous deformities (Burow’s triangles) may also facilitate movement of the flap. Unlike the pivotal flap, in which a single standing cutaneous deformity develops at the base, deformities develop on both sides of the base of advancement flaps. However, they may be excised anywhere along the length of the flap and not necessarily adjacent to the base. Selection of the best location for excising tissue is based on where it can be placed within relaxed skin tension lines or long aesthetic borders. Bilateral Z-plasties performed at the base of the flap often eliminate or reduce the need for excision of standing cutaneous deformities. Occasionally, if the flap is sufficiently long, standing cutaneous deformities can be subdivided into multiple smaller puckers of tissue that need not be excised but merely can be “sewn out” by sequentially suturing the wound lengths in one half. On the face, pedicle advancement flaps work especially well in the forehead (particularly in the vicinity of the eyebrow), helical rim, upper and lower lips, and medial cheek. Mucosal advancement flaps are also useful for vermilion reconstruction. Bilateral advancement of unipedicle flaps is commonly used to close large defects, resulting in H- or T-shaped repairs, depending on the configuration of the defect (Fig. 24-7). Repair in this manner is often referred to as an H-plasty or T-plasty. In both cases, advancement flaps are designed on opposite sides of a defect and advanced toward each other, each responsible for reconstructing a portion of the defect. In such cases, standing cutaneous deformities are often excised partly in the area of the defect and partly along the linear axis of the two flaps. The two flaps harvested from either side of the defect do not necessarily have to be of the same length. The length of each flap is determined primarily by the elasticity and redundancy of the donor resource.
V-Y Advancement Flap
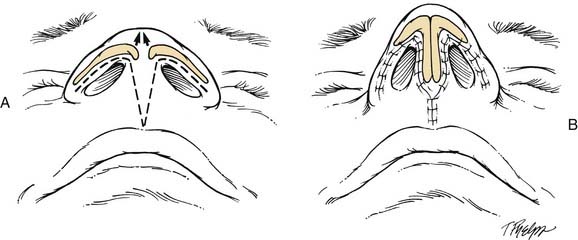
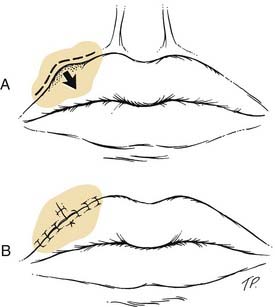
V-Y advancement is useful when a structure or region requires lengthening or release from a contracted state. The technique is particularly effective in lengthening the columella in the repair of cleft lip nasal deformities in which a portion or all of the columella is underdeveloped (Fig. 24-8). A V-Y advancement flap is elevated, recruiting skin from the midportion of the lip between the philtral ridges. The length of the columella is augmented by advancing the flap upward into the base of the columella. The secondary donor defect is approximated by closing the remaining lip skin together in the midline. V-Y advancement is also helpful in releasing contracted scars that distort adjacent structures, such as the eyelid or vermilion. An example is the correction of an ectropion of the vermilion caused by scarring (Fig. 24-9). The segment of distorted vermilion is incorporated into the V-shaped flap and advanced toward the lip to restore the natural topography of the vermilion-cutaneous junction. The skin edges on both sides of the secondary defect are then advanced toward each other and sutured. The suture line becomes the vertical or common limb of the Y configuration.
Hinge Flaps
Hinge flaps are commonly used for repair of full-thickness nasal defects in which the remaining adjacent nasal skin is sufficient to develop a hinge flap for internal nasal lining. Hinge flaps can also be used to close mature sinofacial and salivary fistulas anywhere in the upper aerodigestive tract. Hinge flaps consisting of subcutaneous tissue, and sometimes muscle without overlying skin, can be used to fill in contour deficits.9 Hinged flaps consisting of nasal mucosa (with or without attached septal cartilage) are frequently used for internal lining in the repair of full-thickness nasal defects. These mucosal flaps are axial and do not require a thick base to ensure adequate vascularity.