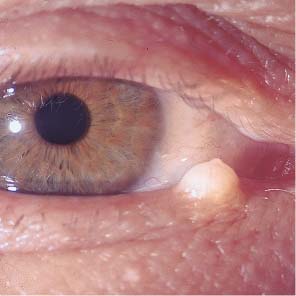
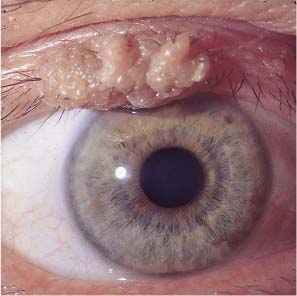
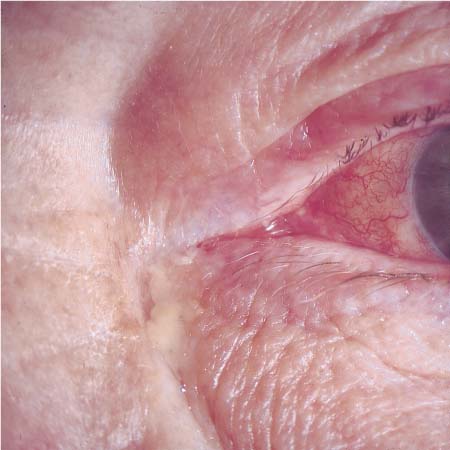
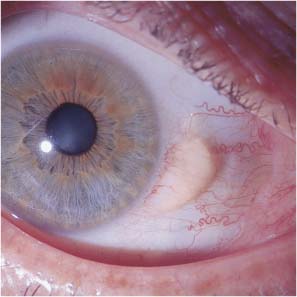
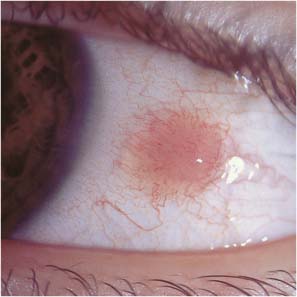
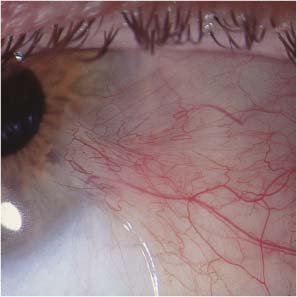
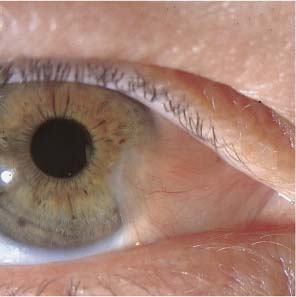
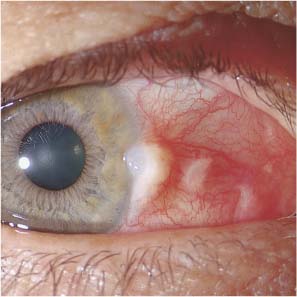
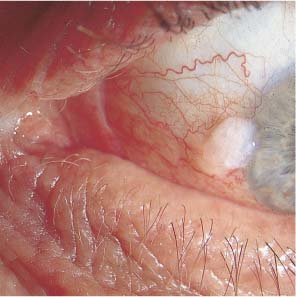
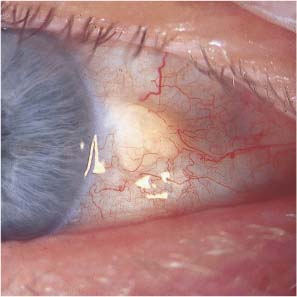
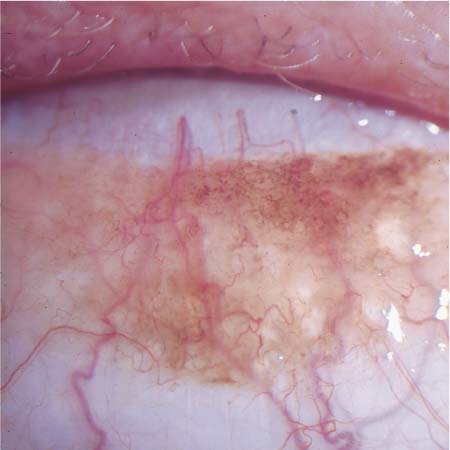
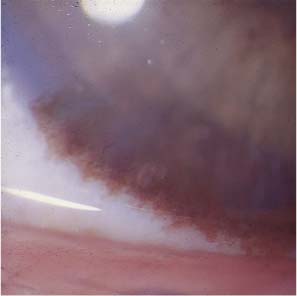
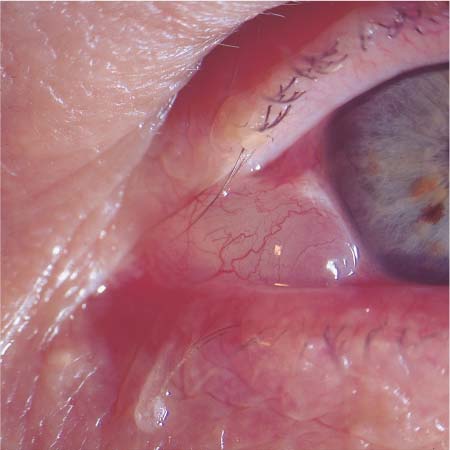
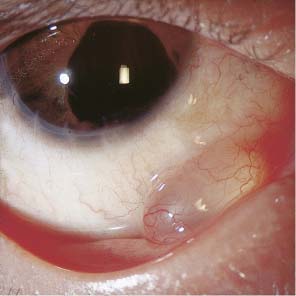
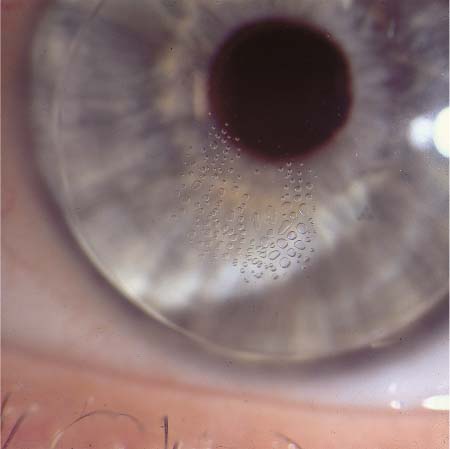
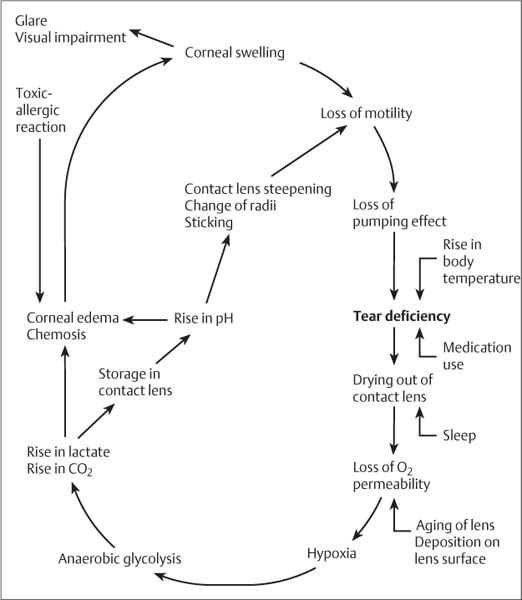
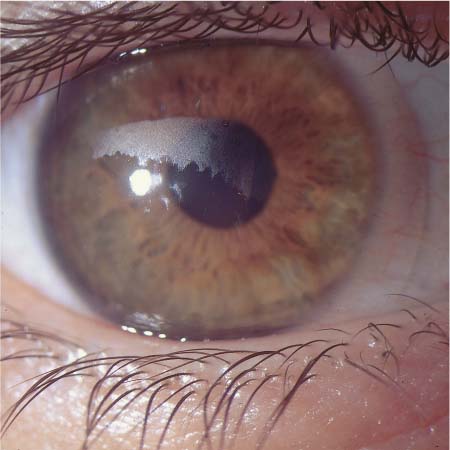
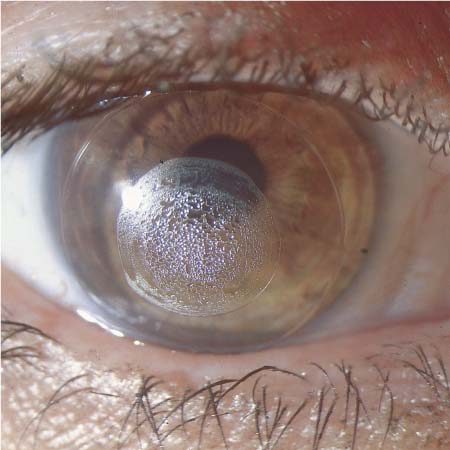
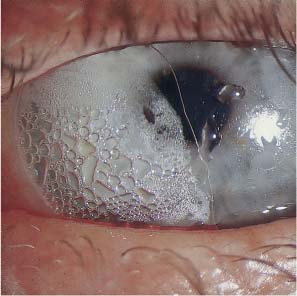
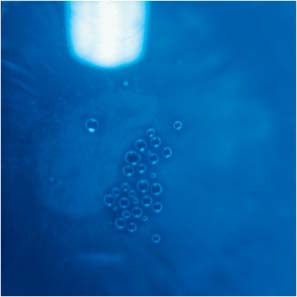
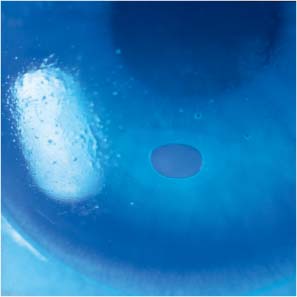
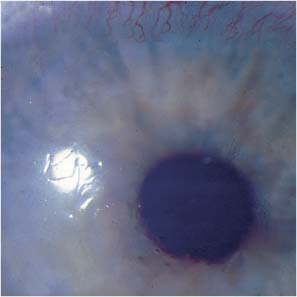
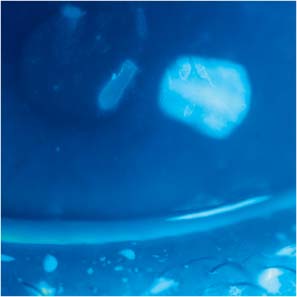
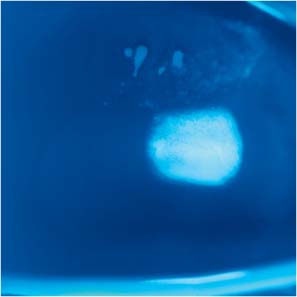
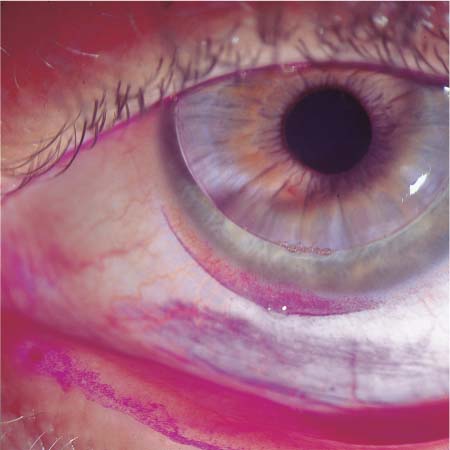
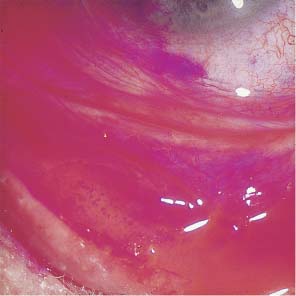
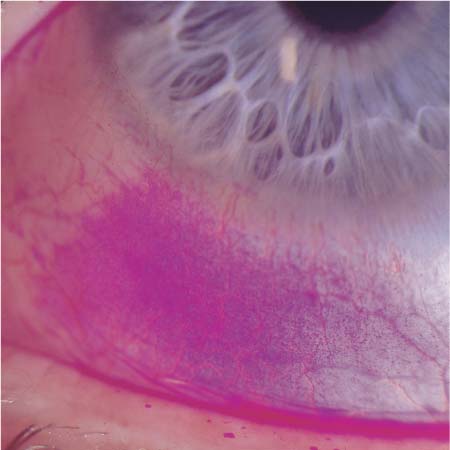
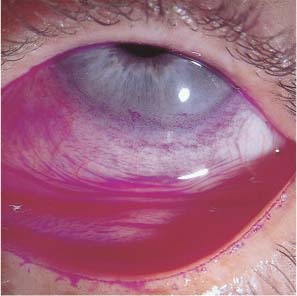
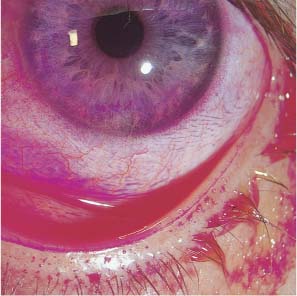
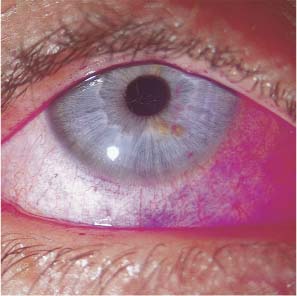
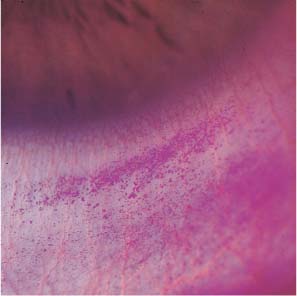
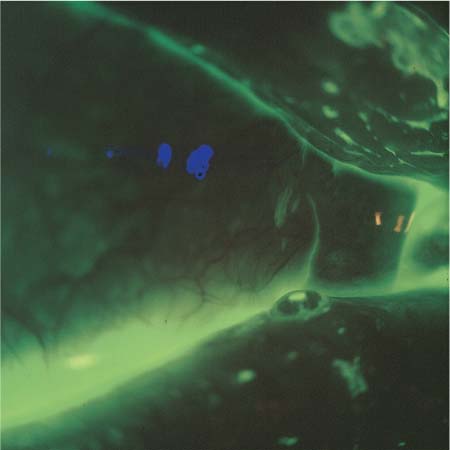
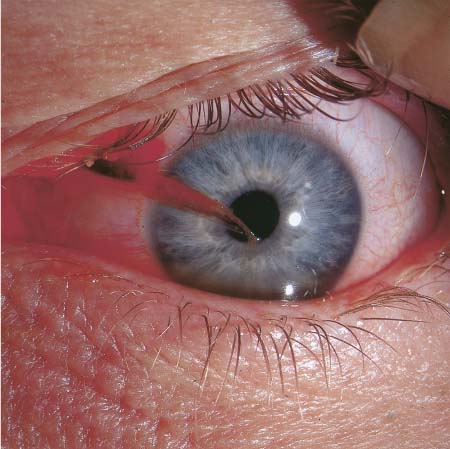
7 Primary Fitting and Wearing Problems Febrile Illnesses, Immune Compromise, Medication Use Tear Deficiency, Disorders of Lacrimation, Dry Eye Many systemic illnesses first manifest themselves in the eye or affect the eye secondarily. Many orally and parenterally administered medications gain access to the eye through the tear fluid and can adhere to the contact lens surface, accumulate in the hydrophilic stroma of soft lenses, and interact with the polymers of which the lenses are composed. Fever elevates not only the core temperature, but also the temperature of the anterior ocular segment. Two consequences of this are a need for an increased amount of tear fluid and an alteration of the conjunctival flora. The normal temperature in the cul-de-sac is 35.6 ± 0.2°C; a rise of as little as 1–2°C creates a favorable environment for the growth of Pseudomonas, which explains why contact lens wearers are much more likely to develop Pseudomonas conjunctivitis or keratitis when suffering from a febrile illness, such as the common cold. Respiratory diseases such as bronchitis or bronchial pneumonia raise the incidence of acanthamoebal, fungal, and pneumococcal corneal ulcers in contact lens wearers. Immune compromise of various causes, including AIDS, leukemia, and antineoplastic chemotherapy, predisposes to ocular infection. It is thus critical that contact lenses are not worn in such situations. Contact-lens-related complications are also more frequent in the presence of systemic diseases affecting the quality and quantity of tears, including thyroid, parathyroid, and other metabolic disorders and renal failure. Florid hepatitis may necessitate discontinuation of contact lenses, as may pregnancy or nursing, in rare cases. Many orally or parenterally administered medications enter the tear fluid and affect wearing comfort. Beta-blockers and hormones are the most prominent examples. The effects of oral contraceptives have already been discussed (p. 5). Coagulopathies or therapeutic anticoagulation can result in massive conjunctival hemorrhage during lens insertion or removal, or indeed while the lenses are worn, after minor trauma to blood vessels of the anterior segment. In patients with active or even latent diabetes mellitus, there is a significantly more frequent colonization of the cornea and conjunctiva with fungi such as Candida and Aspergillus, and a correspondingly higher frequency of fungal infection. Any allergic predisposition may complicate the wearing of contact lenses. Patients who are allergic to synthetic materials in general usually cannot tolerate any type of contact lens material. Patients with ectopic dermatitis may rapidly develop blepharitis after contact lenses are inserted, while patients with allergic vasomotor rhinitis may develop allergic blepharoconjunctivitis or keratopathy. Those who suffer from hay fever can rarely wear their lenses comfortably at the critical times of year. Many ocular diseases can complicate the wearing of contact lenses. The contact lenses themselves, as well as lens care products and wetting solutions, may evoke an allergic response. Ocular infections can become more severe in the presence of contact lenses or be spread by the contact lenses to critical areas of the cornea. It is unknown at present whether premalignant ocular lesions are more likely to transform into malignancy when contact lenses are worn, but unnecessary risks should not be taken; thus, any pigmented spots on the lids or conjunctiva should be noted and photographically documented before fitting, and followed up at regular intervals thereafter. Tear deficiency causes innumerable complications in contact lens wearers; if severe, tear deficiency absolutely contraindicates contact lens wear. The diagnosis and treatment of dry eye is not always a simple matter. The most important acute and chronic ocular diseases that may affect contact lens wear are listed in Tables 27 and 28. Acute infections of the lids, conjunctiva, and cornea complicate contact lens wear. Hordeolum and (more rarely) lid abscess necessitate temporary discontinuation of contact lenses, as the lenses might otherwise be a vector for the spread of pathogenic bacteria to the cornea. Chalazion, in its early infectious phase, poses the same risk to the contact wearer as hordeolum and necessitates temporary discontinuation of contact lenses. In its inactive phase, after healing and encapsulation, it may still be a mechanical hindrance to contact lens wear. Chronic blepharitis is a major problem. Of the many etiological forms of chronic blepharitis, allergic squamous blepharitis is the most likely to develop in contact lens wearers because of an allergy to the lenses or to lens care products. Regardless of treatment, such patients hardly ever tolerate their lenses well over the long term. Chronic, recurrent lid edema of any cause interferes with the lie of the lens on the eye. Contact lens wearers with this problem complain of a foreign body sensation and generally cannot wear contact lenses over the long term. The lie of the lens is also disturbed by ectropion or entropion, as well as by post-traumatic or postsurgical alterations of lid function. Scarring of the lid margin after trauma or infection, lid paresis, or malposition of the punctum can interfere with the flow of tears and thereby complicate contact lens wear. Patients with these problems usually have to stop wearing contact lenses soon after the initial fitting because of a pronounced foreign body sensation and frequent lens loss. Lid trauma New or infected piercing Purulent blepharitis Lid herpes Hordeolum Stye Bacterial, fungal, and viral conjunctivitis Conjunctival trauma Corneal trauma Toxic keratopathy Bacterial, fungal, or viral keratitis Intraocular infection Acute glaucoma Previous eye surgery Lid scarring Malposition of the lids Defects of the lid margin Extensive pinguecula Chalazion Chronic recurrent hordeola Chronic conjunctivitis Conjunctival malformations or neoplasia Filter blebs Recurrent keratitis or uveitis Eyelashes that point inward scrape the cornea and conjunctiva with each lid movement, irritating the anterior ocular segment. If a contact lens is worn, they push it back and forth over the cornea. This condition must be excluded or, if present, corrected before contact lenses are fitted. Lid function and the lie of the contact lens can be adversely affected by any malignant or benign mass of the eyelid, such as a papilloma or sebaceous cyst. Before contact lenses are fitted, such masses should be excised. Fig. 391 Hordeolum, upper lid. Fig. 392 Ulcerated chalazion on the upper lid, infectious process. Fig. 393 Herpes, upper lid margin. Fig. 394 Herpes simplex, upper lid. Fig. 395 Conjunctival cyst, tarsal conjunctiva of lower lid. Fig. 396 Cyst, inner surface of lower lid. Fig. 397 Internal chalazion, lower lid. Fig. 398 Benign tumor of the lower lid margin. Fig. 399 Lid margin papilloma, center of upper lid. Fig. 400 Milium, inner canthus, lower lid. Fig. 401 Wart, central upper lid margin. Fig. 402 Entropion, lower lid. Fig. 403 Ectropion, lower lid. Acute or chronic conjunctivitis of any etiology absolutely contraindicates contact lens wear. Wearing contact lenses in this situation would not only create an intense foreign body sensation but would also be likely to exacerbate the disease process by provoking additional inflammation. Innumerable cases of corneal ulceration in contact lens wearers have occurred on the background of prior bacterial, fungal, or viral conjunctivitis. Conjunctival cuts, hemorrhages, edema, or lesions should be allowed to heal completely before lens wear is resumed. Conjunctival growths, such as pingueculae or pigmented spots, often cause mechanical problems. It remains an unresolved question whether the mechanical irritation caused by a contact lens can promote the transformation of a pigmented spot to a malignant process (melanoma). It would seem prudent to remove any nevus that might be touched by a contact lens before the lens is fitted. Fig. 404 Distichiasis, lash abrading the cornea, foreign body sensation. Fig. 405 Dacryocystitis, occlusion of lacrimal pathway. Fig. 406 Dacryocystitis, occlusion of lacrimal pathway. Fig. 407 Chronic bacterial conjunctivitis. Fig. 408 Pinguecula, conjunctival erosion from the edge of a hard contact lens, stained with rose bengal. Fig. 409 Conjunctival phlyctena. Fig. 410 Pseudopterygium from keratitis. Fig. 411 Pseudopterygium from alkali burn. Fig. 412 Pterygium. Fig. 413 Conjunctival papilloma adjacent to the limbus. Fig. 414 Conjunctival tumor adjacent to the limbus. Fig. 415 Conjunctival tumor adjacent to the limbus. Fig. 416 Conjnctival nevus, benign. Fig. 417 Conjunctival nevus. Fig. 418 Conjunctival nevus, vascularized. Fig. 419 Conjunctival melanosis. Fig. 420 Conjunctival melanoma. Fig. 421 Conjunctival cyst after a perforation of the bulb, aphakia. Fig. 422 Conjunctival cyst. Fig. 423 Conjunctival cyst with extension to the retrobulbar space. Fig. 424 Conjunctival cyst after perforation of the bulb. Fig. 425 Prolapsed conjunctival fatty tissue. Corneal infections and acute corneal processes of any other type contraindicate the wearing of contact lenses. All contact lenses impair the metabolism of the cornea to some extent; though the disturbance is well tolerated by a healthy eye when modern lens systems are used, it is likely to contribute to the progression of any corneal disease that may be present. Within a few hours of being covered by a contact lens, keratitis can develop into a corneal ulcer, and corneal herpes can develop into metaherpetic keratitis. The situation is somewhat different in deformities or degenerative diseases of the cornea, which are often, in fact, a medical indication for contact lenses. They may, however, give rise to major fitting problems, for example in the case of irregular astigmatism or keratoconus. If adequate centration and stabilization of the contact lens cannot be achieved, corrective corneal surgery may be required. Recurrent corneal erosions contraindicate contact lens wear for cosmetic or optical indications, as contact lenses—particularly hard lenses—can repeatedly shear the poorly anchored epithelium from the underlying tissue, causing severe pain. Nonetheless, soft, ultra-thin bandage lenses are an excellent form of treatment for chronic recurrent erosions, as well as for bullous keratopathy, which is often accompanied by endothelial dystrophy. In summary, patients with these conditions should only wear contact lenses for therapeutic indications. Symptoms: Feeling of dryness and grittiness; eye-rubbing; increased ocular temperature; glare. Clinical findings: Persistent conjunctival injection; blurred vision; irregular changes of refractive error while lenses are worn. The tear film serves multiple essential functions for normal vision, as listed in Table 29. Most important is the delivery of nutrients to the avascular cornea and the preservation of physiological and biochemical homeostasis. As shown by recent basic research, the problems associated with tear deficiency that limit lens wear result primarily from nutrient deficiency of the cornea and conjunctiva. Protection against drying Heat exchange, temperature regulation Transport of oxygen, carbon dioxide, nutrients Wetting of the anterior corneal surface Maintenance of optical transparency Optical correction of corneal surface irregularities Disposal of foreign bodies Defense against infection Dry environment: automobile, airplane, workplace Hormone treatment (oral contraceptives, thyroxine, cortisone) Pregnancy, nursing Rheumatic diseases (Sjögren syndrome) Aging, degeneration of the lacrimal glands Chronic conjunctivitis Thyroid and parathyroid disorders Antibiotic treatment Chronic infections, immune deficiency Febrile illness Diabetes mellitus, renal failure, adrenal dysfunction Incomplete lid closure, malformed lids Wearing contact lenses Tear deficiency syndrome and its chief symptom, dry eye, have become increasingly common in recent years, particularly among contact lens wearers. The commonest cause of chronic conjunctivitis, it is a problem frequently encountered in the contact lens clinic. The causes of tear deficiency syndrome are listed in Table 30; its increased frequency today is partly explained by greater levels of environmental pollution and stress, and by longer life expectancy. Tear deficiency syndrome in a contact lens wearer should not be written off as a normal response to environmental pollution or as a psychosomatic manifestation requiring no treatment. Most patients experiencing discomfort with their contact lenses in fact have a demonstrable abnormality of tear function. Nor are the ill effects of tear deficiency syndrome limited to subjective discomfort: any quantitative or qualitative disturbance of the tear fluid can cause metabolic damage to the anterior segment. Absolute lack of tear fluid causes very severe trophic changes of the lids, conjunctiva, and cornea. Fig. 426 Dry eye in a wearer of hard contact lenses, dull lens surface, relative tear deficiency, qualitative deficit, wetting problem. Fig. 427 Dry eye in a wearer of hard contact lenses, air bubbles in the tear lens, quantitative tear deficit. Fig. 428 Dry eye in a wearer of hard contact lenses, air bubbles under the contact lens, quantitative tear deficit. Fig. 429 Dry eye in a wearer of hard contact lenses, bubbles in the tear lens from steep fitting, relative quantitative tear deficit. Illustration 10 Impairment of corneal metabolism by tear deficiency in the contact lens wearer. Tear deficiency leads to elevation of the temperature of the anterior corneal surface and thus to drying out of the contact lens, which thereby becomes less permeable to oxygen (lower Dk). The cornea is then forced to switch to anaerobic glycolysis, as a result of which lactate and pyruvate build up in the tear fluid. Corneal edema ensues, which further impairs lens motility, blocking exchange of the tear film and completing the vicious circle of corneal metabolic decompensation. Tear deficiency in contact lens wearers promotes recurrent infection of the anterior ocular segment with impairment of vision, as well as drying out and sticking of the contact lenses and—mainly in soft hydrophilic lenses—a change in their refractive power. Protracted tear deficiency leads to a collapse of corneal metabolism by a vicious-circle mechanism, as illustrated in Illustration 10. Thus, any clinically documented tear deficiency in a contact lens wearer requires prompt treatment, which should include the elimination of exogenous irritants, endogenous stimulation of lacrimation, reconstitution of a patent tear passageway if necessary, and/or substitution of tear fluid with a suitable artificial tear solution. The tear deficiency syndrome often develops gradually over several years and may be misdiagnosed at first, as its symptomatic presentation is more variable than that of many other ophthalmological conditions. At first, patients usually complain only of itching, burning, and the need to rub the eyes. The patient’s report that the lids are stuck together in the morning and difficult to open is often the first indication of a disturbance of tear function. The foreign body sensation becomes progressively intense as contact lenses are worn, and visual problems develop, such as reduced contrast or increased glare. The patient must blink much more frequently. If tear deficiency syndrome in its early stages is not treated, or treated by the patient himself in unsupervised fashion with nonprescription eye drops, chronic conjunctivitis may ensue. Fig. 430 Dry eye in a wearer of soft contact lenses, wetting problem, mucin deficiency, transient central clouding after each blink. Fig. 431 Tear deficiency, piggyback system, deficit of aqueous phase, inadequate tear lens under a hard contact lens. Fig. 432 Dry eye, hard contact lens, air bubble under the lens, deficit of aqueous phase. Fig. 433 Dry eye, hard contact lens, hydrophobic lens surface, mucin deficiency. Fig. 434 Tear deficiency, soft contact lens, drying evident after 8 hours of wear, bubbles under the lens. Fig. 435 Tear deficiency, soft contact lens, bubbles under the lens after 8 hours of wear, surface wetting problem. Fig. 436 Tear deficiency, soft contact lens, collection of bubbles under the lens, epithelial damage. Fig. 437 Dried out soft lens, bubble under the lens, poor wetting of the lens surface. Fig. 438 Tear deficiency. Dried out, deformed soft lens of high water content. Fig. 439 Tear deficiency. Dried out, deformed soft lens of high water content, bubbles under the lens, epithelial lesion. Dry eye can be worsened by air conditioning or by heating, particularly in an enclosed space such as an automobile. The eyes and contact lenses dry out rapidly in such situations. At first, visual acuity is little affected, but glare is increased. Dry eyes in the contact lens wearer are often accompanied by mild lid swelling and by bulbar conjunctival injection near the limbus at the 3-o’clock and 9-o’clock position, which may be grossly visible. The symptoms and signs of tear deficiency in the contact lens wearer are listed in Table 31. Hard contact lenses, if examined while still on the eye in tear deficiency syndrome, show a dull surface with dry areas, possibly with adherent remnants of pigment from eye make-up. Soft lenses have plaques and may be deformed; changes of the central corneal curvature are best detected with an ophthalmometer or keratometer. Visual acuity is decreased and is not improved by over-refraction, yet transiently normalizes upon instillation of artificial tears in the lower cul-de-sac. Foreign body sensation Eye-rubbing Burning Itching Visual impairment Glare Reduced contrast Haloes, veiled vision Deformation of gel contact lenses Slit-lamp examination always reveals evidence of acute or chronic conjunctivitis, that is, diffuse, brick-red bulbar conjunctival hyperemia, possibly accompanied by bulbar conjunctival folds parallel to the lid margin. The gross appearance of the cornea is normal, but fluorescein staining reveals sporadic, fine, stippled epithelial defects, which (like conjunctival hyperemia) are somewhat more pronounced along the horizontal than along the vertical axis. In mild cases, fluorescein staining after lens removal shows no more than a barely detectable corneal edema. In more severe cases, cellular metaplasia and other defects are present and readily visible with rose bengal staining, and pachymetry reveals that the dried-out cornea is somewhat thinner than normal. Decompensated tear deficiency syndrome in the contact lens wearer is characterized by multiple epithelial defects, stromal swelling, and endothelial changes, all of which indicate a collapse of corneal metabolism. There may be clinical progression to chronic conjunctivitis or tight lens syndrome (TLS). In the most severe cases, tear deficiency may lead to keratitis; when tears are totally absent, as in lagophthalmic keratitis, corneal ulceration may occur, leading to permanent corneal damage and loss of visual function. Type B keratoconus also seems to have a causal relationship to tear deficiency, as a significant tear deficiency is always present in the early stage of the disease. The symptoms of tear deficiency syndrome are more pronounced in contact lens wearers than in spectacle wearers, because the comfort of contact lens wear essentially depends on the presence of adequate tear fluid. A dry, dull lens surface, air bubbles between the lens and the cornea after long periods of wear, and immobility of the lens during blinking or saccadic movements are sure signs of tear deficiency or inadequate wetting. Fluctuating refractive power, or instability of the cylinder axis, in wearers of soft lenses also indicates that the lens is not fully moistened by the tear fluid. Fig. 440 Corneal erosion in a soft lens wearer with tear deficiency, diminished corneal reflex from drying. Fig. 441 Corneal erosion, incipient bullous separation, tear-deficient soft lens wearer, diminished corneal reflex caused by drying of the corneal surface. Fig. 442 Corneal edema and epithelial damage due to tear deficiency, hard contact lens, deficit of aqueous phase. Fig. 443 Epithelial and stromal edema due to tear deficiency, hard contact lens, deficit of the wetting component of tears. Fig. 444 Decreased slit-lamp reflex from the anterior surface of a soft contact lens, inadequate wetting of the lens material. Fig. 445 Decreased slit lamp reflex from the anterior surface of a soft contact lens, staining shows stippling of the lens surface, lens desiccated. Fig. 446 Poor wetting, instability of the tear film on the anterior surface of a hard lens, mucin deficiency. Fig. 447 Poor wetting, instability of the tear film on the anterior surface of a soft lens. Fig. 448 Normal BUT: tear film intact at 10 seconds. Fig. 449 Borderline BUT, break in film at 8 seconds. Fig. 450 Pathological BUT, break in film at 5 seconds. Fig. 451 Highly pathological BUT, break in film at 2 seconds. Fig. 452 Tear deficiency, hard contact lens, rose bengal staining, abrasion below the limbus caused by the lens because of tear deficiency. Fig. 453 Perilimbal traces of abrasion from wearing hard contact lenses, relative tear deficiency, staining with rose bengal. Fig. 454 Traces of abrasion from the overlying hard contact lens, tear deficiency, rose bengal staining. Fig. 455 Hard lens wearer with severe tear deficiency, absolutely unable to wear contact lenses. Fig. 456 Severe tear deficiency syndrome, absolute contra-indication for contact lenses. Fig. 457 Tear deficiency, rose bengal test after 8 hours of wearing a RGP lens. Fig. 458 Tear dysfunction, soft contact lens wearer, traces of conjunctival abrasion, rose bengal staining. Fig. 459 Tear deficiency, soft lens wearer, traces of abrasion at the limbus, rose bengal staining. Fig. 460 Tear dysfunction, soft lens wearer, traces of abrasion on the cornea and conjunctiva, rose bengal staining. Fig. 461 Tear deficiency, soft lens wearer, traces of abrasion in the region covered by the lens haptic, rose bengal staining. Fig. 462 Corneoscleral lens wearer with dry eye, conjunctival epithelial lesions with marked staining at the limbus, poor fitting, loss of lens. Fig. 463 Dry eye, aphakia, tear deficiency syndrome. Lens worn without difficulty after insertion of a flow-controller in the lower punctum. Fig. 464 Blunt trauma from a squash ball in a wearer of soft lenses. Fig. 465 Perforating wound from a screwdriver; RGP lens wearer. Fig. 466 Perforating wound from a glass shard; soft contact lens wearer. The diagnosis of tear deficiency syndrome is established by quantitative and qualitative clinical testing of tear function. Testing is difficult in routine practice, however, because of the small volumes concerned, as compared to other bodily secretions: the average normal daily production of tear fluid is only about 1.0 ml. Thus, tear deficiency syndrome cannot always be reliably diagnosed in its early stage. A single test does not suffice to establish the diagnosis of tear deficiency, as there may be an isolated disturbance of the volume of tear production or of wettability, and there are also combined disorders that cannot be reliably diagnosed with the Schirmer test or by measurement of the break-up time (BUT). Therefore, when there is clinical suspicion of tear deficiency syndrome, the use of multiple tests of the types described here is recommended. The more important tests are listed in Tables 32 and 33. The simplest way to estimate the amount of tear flow is by the Schirmer I test (without local anesthetic) and the Schirmer II test (with a local anesthetic such as proparacaine), which, however, like most other methods of direct measurement, provide only an inexact estimate of the total secreted volume. All direct methods elicit reflex tearing through contact with sensitive tissue, and may thus yield artificially high values; on the other hand, the relative hypesthesia induced by contact lens wearing sometimes diminishes reflex lacrimation, leading to artificially low values. Contact lenses must not be worn for at least 24 hours before the test. A normal finding in Schirmer I or Schirmer II is wetting of at least 10 mm of the test strip in 5 minutes. Schirmer I test Schirmer II test (with local anesthetic) BUT Warm air provocation test Fluorescein staining Rose bengal staining Meniscus test Pachymetry Thermometry Iron Sodium Potassium Calcium Immunoglobulins Rheumatoid factors Blood glucose The quality of the tear film is most easily assessed while the lens is on the eye by measurement of the lens tear-film BUT, which, unlike BUT measurement in the eye without a contact lens, is best performed without fluorescein. After spontaneous opening of the lids, the tear film on the anterior surface of the contact lens must remain intact for at least 10 seconds before breaking up. Values of 6–9 seconds are considered possibly abnormal; values less than 6 seconds are definitely abnormal and contraindicate the wearing of either hard or soft lenses for cosmetic reasons. Measurement of the height of the tear meniscus at the center of the lower lid is performed with a reticle in one of the slit lamp eyepieces and, like BUT measurement, requires no contact with the anterior ocular segment. It is easily carried out during routine follow-up examination of the contact lens wearer. The result may, however, be difficult to interpret: values less than 0.2 mm are clearly abnormal, but higher values do not rule out tear deficiency syndrome, as dryness of the eye may be masked in the examining situation by reflex tearing. Staining with a 2% solution of the vital dye rose bengal provides a much more accurate assessment of the state of the anterior ocular segment in dry eye syndrome. This test is primarily useful in advanced stages of the condition, as it stains necrotic epithelial cells; it is typically positive only when the Schirmer II test result is less than 3 mm and the BUT is less than 6 seconds. The contact lens must be removed before the dye is instilled in the inferior cul-de-sac, as it may otherwise be irreversibly stained. The dye is irritating, but the eye should not be pretreated with local anesthetic as this may produce false-positive results. Like rose bengal, this dye stains necrotic epithelial cells, with the advantage that it does not sting. This is a simple and easy provocative test for dry eye in the contact lens wearer. A stream of warm air from an electric hair drier is directed at the patient’s open eyes from a distance of 1 m. Patients complaining of an uncomfortable foreign body sensation or dryness within 10 seconds usually suffer from a tear disorder. Pachymetry and (better still) micropachymetry are the most accurate diagnostic tests for tear deficiency syndrome in contact lens wearers and enable differentiation of its various stages and clinical types. The central corneal thickness (CCT) is normally 545 ± 20 μm. Values less than 525 μm indicate thinning of the cornea through desiccation, tissue loss, or both; in such cases, the average CCT over the course of the day is below 500 μm. On the other hand, absolute or near-absolute lack of tears can cause marked corneal swelling, to a CCT well over 600 μm. When interpreting CCT values, however, one must remember that the corneal thickness is subject to the influence of various mechanical and metabolic factors when contact lenses are worn. It is therefore advisable to measure the CCT several times over the course of the day. Another, easier way to test for tear deficiency syndrome is to measure the CCT before and after instillation of a drop of artificial tear fluid in the conjunctival sac; if the CCT remains constant over the ensuing 20 minutes, then tear function is adequate. Measuring the temperature of the anterior segment is a further aid to the diagnosis of tear deficiency syndrome. Infrared thermography of the cornea and conjunctiva provide the clearest documentation of temperature changes, but it requires specialized equipment that is not usually available in routine clinical practice. Instead, the temperature of the anterior segment can be measured with a hand-held thermistor placed on the fold of the closed upper lid. The normal temperature is 35–36°C; elevations are due to relative or absolute tear deficiency. This method can be used to assess the efficacy of treatment for dry eye with eye drops, gels, sprays, or ointments: the longer the decline in temperature persists after one of these products is applied, the more effective the treatment. Note: The cause of dry eye should be determined before treatment is initiated; underlying disease processes, if found, should be treated first. Artificial tears should be used as little as possible, in order not to suppress lacrimation. Gels and ointments are contraindicated while contact lenses are worn.
Systemic Disease
Febrile Illnesses, Immune Compromise, Medication Use
Allergy
Primary Ocular Disease
Lid Diseases
Conjunctival Diseases
Corneal Diseases
Tear Deficiency, Disorders of Lacrimation, Dry Eye
Pathophysiology
Clinical Course
Clinical Testing
Schirmer I and II Tests
Measurement of Break-up Time
Meniscus Test
Rose Bengal Test
Lissamine Green Test
Warm Air Provocation Test
Pachymetry
Thermometry
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ento Key
Fastest Otolaryngology & Ophthalmology Insight Engine