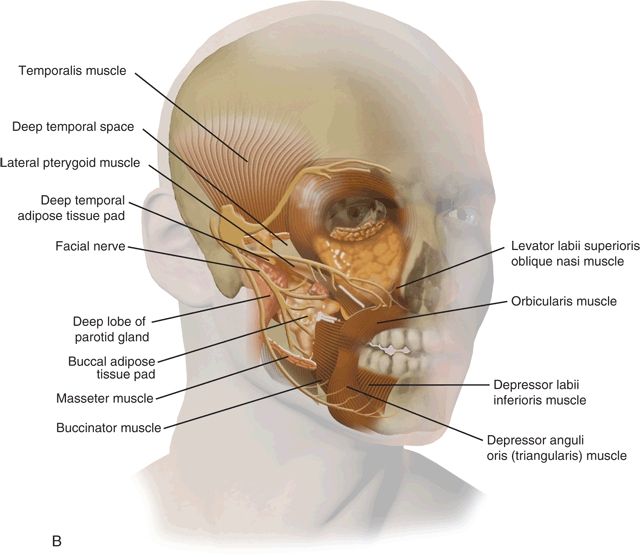
Figure 31.1 Anatomical description of the right ITF. A. Lateral view of the skull. B. Anterolateral view of the soft tissue structures.
Less than 1% of all head and neck neoplasms originate in the ITF. These can be either primary tumors or secondary tumors that invade or metastasize to the ITF. Primary ITF tumors can originate from any tissue within this compartment: nerve, vessels, muscle, bone, cartilage or connective tissue. These tumors may go undetected for a long period of time, after which they usually present as a symptomatic mass in the temporal area. Primary benign tumors that may involve the ITF include meningioma, juvenile angiofibroma, neurofibroma, schwannoma, fibroma, osteoma, and fibrous dysplasia. Malignant tumors include chordoma, soft tissue sarcomas, nasopharyngeal carcinoma, and sinonasal carcinomas. Tumors that may invade this space include carcinomas of the skin, sinonasal mucosa, or minor salivary glands.
The complex anatomy of the ITF accounts for the diversity of surgical approaches used to remove tumors from this anatomic area. The surgical approach is tailored according to the anatomical extent of the tumor, its histologic type (benign or malignant), and the patient’s past medical history (previous surgery or radiation treatment).
Large tumors that involve the ITF can be approached extracranially and intracranially depending on the primary origin of the tumor and its extensions. The contemporary surgical technique for resection of tumors arising in the ITF is based on the classical approach developed by Fisch and Mattox that involved a retroauricular incision and transposition of the entire facial nerve. The classical type-C Fisch ITF approach provides access from the sigmoid sinus to the parasellar region, cavernous sinus, and Meckel’s cave. The main limitation of this approach is that it imminently leads to conductive hearing loss and facial nerve neuropraxia, which are rarely encountered in the modern approach. Other variations of the Fisch approach are the lateral facial and lateral transtemporal sphenoid approaches, which allow limited superior access to the middle cranial fossa. The lateral facial approach provides access to small tumors of the middle fossa and is limited by the inferior displacement of the zygomatic arch and temporalis muscle (Fig. 31.2). Removal of the zygomatic arch in the lateral temporal sphenoid approach allows wider exposure of the subtemporal region and allows intracranial and extracranial removal of the tumor without rerouting the facial nerve.


Figure 31.2 Lateral facial approach to the cranial base. This approach allows limited access to the subtemporal area without removal of the zygoma. A. A question mark incision is used to expose the temporalis muscle and the lateral orbit (ribbon retractor). B. A pterional craniotomy is performed. Retraction of the temporal lobe dura reveals branches of the trigeminal nerve and attachment of the pterygoid plate at the base of the sphenoid bone.
The more common subtemporal–preauricular infratemporal fossa approach developed by Sekhar, Janecka, and Schramm is a combination of the lateral transtemporal sphenoid approach and the transparotid approach to the parapharyngeal space, in addition to temporal craniotomy (Fig. 31.3). It is also known as the lateral transtemporal infratemporal fossa approach. This approach affords wide exposure to the structures of the middle cranial base using a combination of transparotid, lateral transtemporal sphenoid, and temporal craniotomy approaches. This approach allows access to various anatomical areas including the temporal and infratemporal fossa, temporal lobe, parasellar region, retro-orbital region, nasopharynx, retromaxillary space, pterygopalatine space, masticatory space, retromaxillary fissure and pterygoid plates, sphenoid ridge, and trigeminal nerve. The main advantages of this technique are excellent exposure of the middle cranial fossa and infratemporal compartments and minimal sensory–motor morbidity. This chapter describes the technique of the preauricular ITF approach and its combination with various other important techniques used in surgery of the cranial base.
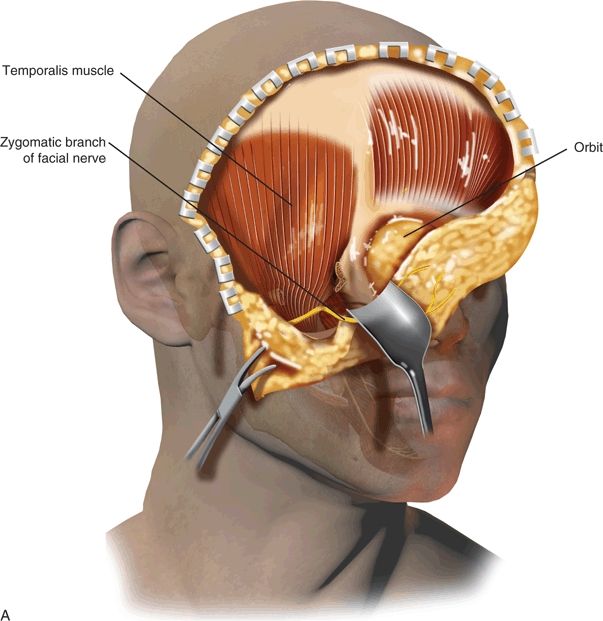
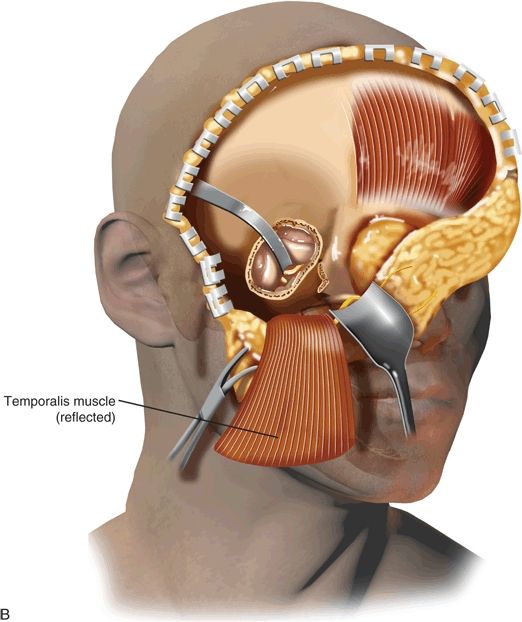
Figure 31.3 Subtemporal–preauricular and infratemporal approach to the cranial base as described by Sekhar and Janecka. A. Initial exposure is similar to the lateral facial approach shown in Figure 31.2. The caudal exposure is extended by removal of the zygomatic arch. Figure 31.3(Continued ) B. The temporalis muscle has been reflected inferiorly after removing the zygomatic arch, the mandibular condyle has been resected, and a subtemporal craniectomy has been performed.
HISTORY
The clinical presentation of ITF tumors varies greatly and relates directly to the location and rate of growth of the lesion. A thorough history of the present illness as well as past medical and surgical histories are obtained. In addition to the relevant risk factors, the patient is questioned regarding symptoms of cranial nerve dysfunction, head and ear aches, trismus, bleeding from the ear, and otorrhea. Signs and symptoms can often be misleading and may initially be interpreted as being infectious and benign diseases. Common symptoms and signs suggestive of tumors of the ITF include the following: (1) facial swelling and asymmetry that can result from tissue destruction and advancement of the tumor into the soft tissues of the head and neck; (2) palpable metastatic adenopathy, a possible indication of advanced disease; (3) hearing loss usually resulting from extension of the tumor and obstruction of the eustachian tube or middle or inner ear, (4) numbness of the face or pain as a manifestation of tumor invasion into various branches of the trigeminal nerve; and (5) neurologic or ocular manifestations, such as diplopia, exophthalmos, and multiple cranial nerve palsies, that suggest invasion of the nerves at the skull base or cavernous sinus. Pain is a significant adverse symptom suggestive of a malignant tumor. The classical triad of signs of cancer of the temporal bone includes otorrhea, pain, and bleeding. The usual comorbidities should be identified in addition to mental disorders and active alcohol, drug, or tobacco abuse. In addition to the above criteria, potential candidates must be well-informed about surgery, must be motivated, and should be prepared to accept long-term postsurgical follow-up.
PHYSICAL EXAMINATION
Physical examination should include a meticulous survey of the temporal area and auricular and preauricular skin. The neck and parotid gland are palpated in search of lymph node metastases. The function of the facial and other cranial nerves is evaluated. Otoscopy is used to define the extent of the tumor in the external auditory canal. If the tympanic membrane can be seen, its integrity is verified. Jaw movement and trismus are examined as a potential sign of extension of the tumor into the temporomandibular joint (TMJ). Cranial nerve function is evaluated.
The comprehensive physical examination should always include an endoscopic evaluation of the nose, sinuses, nasopharynx, and oropharynx. Masses should be examined for friability, vascularity, bleeding, and signs of necrosis, possibly suggesting malignancy and necessitating additional investigation. Different entities may display specific and pathognomonic findings on physical examination, for example a vascular mass arising from the hypotympanum on otoscopic examination. However, most tumors are similar in their initial and late symptoms and demand a high level of suspicion in order to reach the correct final diagnosis. This type of tumor will silently advance in size and extent until it has infiltrated a cranial nerve or grown sufficiently to obstruct the nasopharynx. The most common findings on physical examination include the following: (1) nasal, paranasal, or nasopharyngeal mass. (2) Proptosis, the mild protrusion of the eye, may be consistent with tumor compression of the periorbita without frank invasion. (3) Cranial nerve deficits are always considered to be indicators of advanced disease and a poor prognosis. For example, invasion of the cavernous sinus by cancer, as can be suspected from signs of involvement of the abducens nerve, can be an absolute contraindication for surgery. (4) Any abnormal findings on the neurologic examination should raise the suspicion of involvement of the dura and brain. (5) A suspicious mass in the neck suggests the presence of a malignant tumor that has already undergone regional lymph node metastasis. (6) Unilateral middle ear effusion is an uncommon finding that mandates a thorough examination of the nasopharynx to rule out eustachian tube obstruction. Fiberoptic evaluation of the upper aerodigestive tract is an integral part of the physical examination. Sites of potential donor tissue to be used for reconstruction are examined.
INDICATIONS
Indications for surgery include extirpation of benign and malignant tumors that originate in the ITF or that invade this compartment from neighboring structures. Rarely, this approach is performed for treatment of infectious diseases including local abscess or necrotizing fasciitis. Tailored treatment should take into consideration the fact that survival after recurrent or residual disease, as well as prior radiotherapy, is lower compared to primary treatment, and that the main cause of death is local recurrence rather than regional or distant metastases. For these reasons, an aggressive effort toward complete extirpation should be made whenever cure is the goal of the treatment or for palliation of intractable pain. Cosmesis and function are addressed by an adequate reconstruction plan.
When contemplating treatment of a specific patient, the following key questions need to be addressed: What is the goal of the treatment? What is the appropriate extent and nature of surgical resection? Is postoperative adjuvant therapy with radiation or chemoradiation anticipated? And finally, what reconstruction techniques will be employed?
CONTRAINDICATIONS
Contraindications for surgery include the diagnosis of tumors amenable to chemoradiation therapy (lymphoma, carcinomas of oropharyngeal or nasopharyngeal origin) and evidence of distant metastases. An exception is adenoid cystic carcinoma or single metastases of specific tumors (e.g., melanoma and sarcomas) that are amenable to excision. Cancer invasion of the prevertebral fascia, encasement of the carotid artery, invasion of the cavernous sinus, and considerable brain involvement are also considered contraindications for surgery. Stable small paragangliomas or schwannomas can be followed radiographically with magnetic resonance imaging (MRI). Severe comorbidities, marked debilitated status, or demented patients are considered to be potential contraindications for surgery.
PREOPERATIVE PLANNING
Imaging Studies
Imaging should always be used prior to surgery since it can influence decision making. A contrast computerized tomographic (CT) scan and a basic MRI study with fat suppression should be used for preoperative evaluation and decision making regarding treatment. A T2-weighted MRI study with fat suppression is usually added (Fig. 31.4). Visualization of a vascular flow void on an MRI study is usually sufficient for the diagnosis of a vascular tumor such as a paraganglioma, but magnetic resonance angiography may be added for a more precise diagnosis. Malignant tumors usually demonstrate a soft tissue mass invading intracranial or adjacent spaces, accompanied by bone destruction. The CT may show mild enhancement, and T1-weighted MRI may demonstrate strong postcontrast enhancement. Application of a fat suppression technique, such as short tau inversion recovery and frequency-selected fat suppression, eliminates strong signals from adipose tissue. In addition, the definition of normal anatomic structures is significantly improved, enhancing lesions become clearer, and the margins of a lesion are better defined when suppression of fat is used in combination with contrast enhancement. MRI 3D reconstruction enables multiplanar imaging of tumor extension and vessel encasement. These features can be established in tumors as small as 10 mm in diameter. If a malignant tumor is suspected, radiologic staging of the patients is completed by using a positron emission tomography–CT hybrid for assessing the presence of regional and distant metastases. Most of the malignant tumors arising in the ITF can invade the intracranial compartment, maxilla, mandible or TMJ, orbit and auditory canal, or skin. Other routes of spread include hematogenous, lymphatic, or perineural invasion along cranial nerves. Perineural invasion is common in adenoid cystic carcinoma and is the pathway to the intracranial space so that imaging studies should be directed toward the foramen ovale and rotundum, the cavernous sinus, orbital apex, trigeminal ganglion, and dura. In addition, the radiologic evaluation must include the neck in any case of suspected malignancy to evaluate for lymph node metastasis. Patients with suspected paragangliomas will require preoperative embolization a few days prior to surgery.
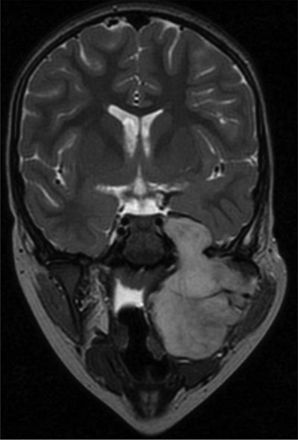
Figure 31.4 Magnetic resonance imaging of the ITF. A coronal T2 MR image of a child with a large rhabdomyosarcoma of the ITF.
Tissue Diagnosis
Tissue diagnosis should be an integral part of preoperative evaluation. Although radiologic imaging could provide indications regarding the type of neoplasm, tissue diagnosis is sensitive to differences between benign and malignant lesions. Fine needle aspiration (FNA) biopsy can be performed via ultrasound but frequently will require CT-guided FNA, which is technically challenging. Radiologic imaging should precede FNA if a vascular tumor is suspected to avoid potential bleeding. Some exceptions to preoperative biopsy include juvenile angiofibroma and paragangliomas.
SURGICAL TECHNIQUE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


