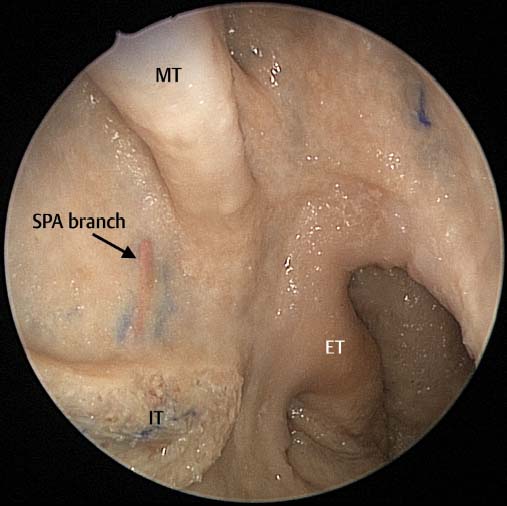
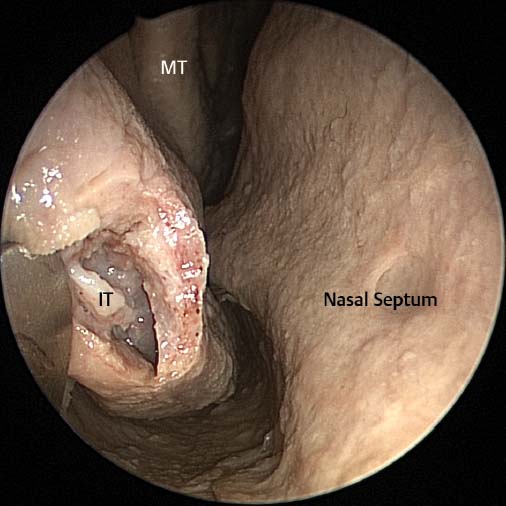
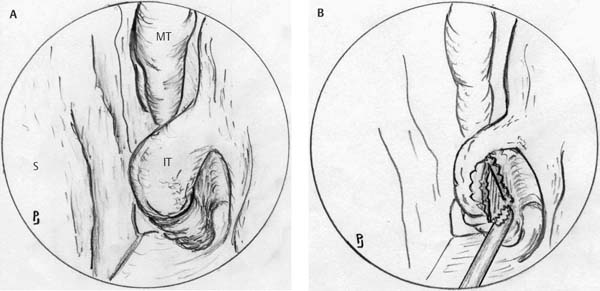
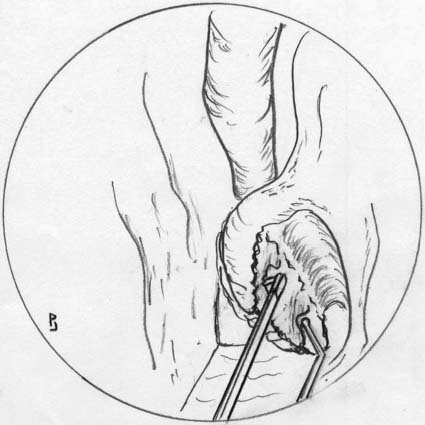
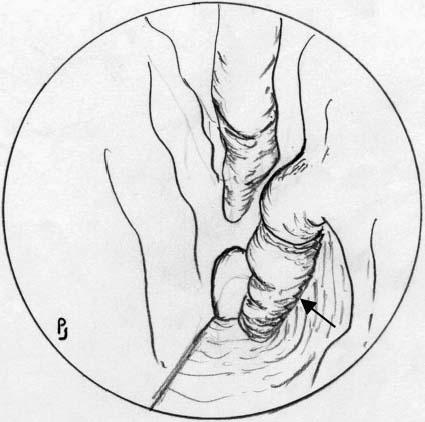
4 Turbinectomy is seldom required in patients with chronic sinusitis because successful surgical management of the sinuses will in most cases result in normalization of the mucosa of the inferior turbinates. The inflammatory cytokines and cells contained within the mucus emanating from the diseased sinuses causes an inflammatory response from the mucosa of the inferior and middle turbinates. Once the sinuses are properly aerated and this inflammatory exudate resolves, the edema of the turbinate mucosa subsides. However, in patients with ostiomeatal complex disease or minimal maxillary mucosal thickening as their only computed tomography (CT) findings, who have nasal obstruction as their main nasal symptom, turbinoplasty with mini functional endoscopic sinus surgery (FESS) may be needed to resolve these patients’ symptoms. In addition, there are some patients without sinus disease who have intractable inferior turbinate hypertrophy (nonresponsive to treatment), and in which turbinate reduction can improve the patient’s nasal airway and quality of life. There have been many techniques described for inferior turbinate reduction and these include submucous turbinoplasty, partial turbinectomy, complete turbinectomy, and diathermy (usually performed in the submucosal plane).1–5 Arguments against complete removal of the inferior turbinates cite the risk of the patient developing atrophic rhinitis, especially in hot and dry climates.1 In addition, amputation of the turbinate flush with the lateral nasal wall will inevitably result in a significant bleed at the time of surgery as the branch of the sphenopalatine artery to the inferior turbinate is cut6 (Fig. 4.1). This may require diathermy of the bleeder and this again increases the amount of necrotic tissue and results in significant postoperative crusting. Partial turbinectomy may also result in significant bleeding and require diathermy for control. Submucosal turbinoplasty and diathermy, although initially effective, does not appear to have the same long-term success as partial or complete turbinectomy.1,7 In addition we are all aware of the patients who have undergone turbinectomy and have a capacious nasal airway but still have the sensation of nasal obstruction.1 This may be due to the removal or destruction of airflow receptors on the medial and superior aspect of the inferior turbinate. However, this remains to be proven. The other significant problem patients suffer from after turbinectomy or diathermy (not submucous turbinoplasty) is crusting on the cut surface of turbinate.6–8 This problem increases if diathermy has been used to control bleeding. These crusts can be uncomfortable and cause nasal obstruction. In addition, hemorrhage may occur when they either fall off or are removed.1,3 In the group of patients undergoing submucosal diathermy and to a lesser extent submucosal turbinoplasty, they have significant postoperative swelling of the inferior turbinate which obliterates the nasal cavity and makes the first 3 weeks after surgery very uncomfortable for the patient who is usually unable to breathe through their nose.7 Powered inferior turbinoplasty was designed to preserve the medial wall of the inferior turbinate thereby preserving the airflow receptors. In addition the technique allows the inferior turbinate to be reduced in size by ~50% without leaving a raw surface for crusts to form in the postoperative period. Under general or local anesthetic the anterior end of the inferior turbinate is infiltrated with lidocaine 2% and 1:80 000 or 1:100 000 adrenaline. A spinal needle attached to a 2-mL syringe is used to infiltrate along the posterior inferior border of the inferior turbinate. The turbinate is fractured medially allowing space for the endoscope (zero degree) and powered microdebrider to be placed. A 12-degree or straight blade is used in oscillate mode to remove the soft tissue from the lateral aspect of the vertical portion of the inferior turbinate (Fig. 4.2). The debrider is then set on forward mode and the majority of the bone removed with the rotating blade. If the oscillate mode is used for bone removal this may result in bone and portions of the medial surface of the turbinate being removed. If possible this should be avoided as the medial portion of the turbinate should be preserved so it can be rolled upon itself at the end of the procedure (Fig. 4.3). Any residual bony fragments are dissected free with a ball probe (Fig. 4.4). The inferior turbinate bone often thickens considerably as the dissection is continued anteriorly. It is often useful to use the pediatric backbiter to facilitate the dissection of this bone. It is critical that this bone is removed as it is in this region that the nose is narrowest and where the greatest degree of benefit of the operation will be achieved. Fig. 4.1 Cadaveric dissection of the right posterior lateral nasal wall demonstrating the inferior turbinate (IT) branch of the sphenopalatine artery (SPA). Note the relationship between the posterior attachment of the middle and inferior turbinates to the sphenopalatine foramen and palatine bone. Fig. 4.2 Mucosa from the head of the inferior turbinate (IT) has been removed with the straight microdebrider demonstrating the underlying inferior turbinate bone. MT, middle turbinate. Once all the lateral mucosa and bone has been removed the remaining mucosa is rolled upon itself covering the raw area. The Freer elevator is used to roll the mucosa and, if necessary, fracture the horizontal portion of the remaining inferior turbinate laterally. This reduces the size of the turbinate by ~50% (Fig. 4.5). Fig. 4.3 (A) The inferior turbinate (IT) has been sufficiently mobilized to allow the microdebrider and endoscope to pass underneath it into the inferior meatus. The middle turbinate (MT) and septum (S) are seen. (B) The microdebrider blade is used to remove the tissue and some of the vertical bone from the lateral aspect of the inferior turbinate. Fig. 4.4 The ball probe is used to remove the more posterior bony fragments and the backbiter used for the thicker more anterior bone. The before and after pictures taken during surgery are presented in Fig. 4.6. It can clearly be seen that the size of the inferior turbinate is reduced by around 50%. A rectangular sheet of Surgicel (Ethicon, Somerville, NJ) is placed over the rolled turbinate to keep it in place and prevent the mucosa from unrolling (Fig. 4.7). It also provides a degree of hemostasis. No other packing is placed in the nose.
Powered Inferior Turbinoplasty and
Endoscopic Septoplasty
 Powered Endoscopic Inferior Turbinoplasty (Video 1)
Powered Endoscopic Inferior Turbinoplasty (Video 1)
Surgical Technique (Video 1)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree