Chapter 1 Otologic Instrumentation
Sophisticated micro-otosurgical techniques mandate that the otologic surgeon and surgical team have an in-depth understanding of the operating room (OR) layout and surgical instrumentation. This chapter describes in detail different surgical procedures. The OR setup and instruments necessary for the various types of otologic procedures are described. Appendix 1 provides a comprehensive list of instruments and equipment.
OPERATING ROOM
The OR for otologic surgery requires features that differ from ORs used for nonotologic surgery. The following sections elaborate on the general environment of the OR designed for ear surgery. A word about the sterile field is in order. Respecting the sterile field is vital during routine otologic surgery, and takes on special significance during neurotologic procedures. Maintaining the proper environment means limiting traffic through the OR, and keeping the number of visitors to a minimum. It is preferable for observers to be in a remote room watching the procedures on video. Individuals allowed in the OR should be experienced in sterile technique and should wear jackets over scrubs so that all skin surfaces are covered (Fig. 1-1).
The first piece of OR equipment to be discussed is the operating table. The surgeon must be comfortable while performing microsurgery. Adequate leg room under the table can be achieved with older OR tables by placing the patient 180 degrees opposite the usual position; in other words, the patient’s head is where the feet would normally be (Fig. 1-2). Newer electric tables easily accommodate the patient and surgeon. Because most otologists spin the OR table 180 degrees after the induction of anesthesia, the new tables allow for spinning the table without unlocking it. Nonetheless, after the patient is properly positioned, the table must be firmly locked in place.
All ORs are equipped with wall suction. Standard suction devices are acceptable for otologic surgery. It is preferable, however, to use a multiple-canister suction setup, minimizing the number of times the bottles must be emptied (Fig. 1-3). Suction systems have several locations where the amount of suction can be varied, but the surgeon should also employ a control clamp on the suction tubing on the sterile field (Fig. 1-4).
High-speed drills capable of doing most of the bone work in the temporal bone include the Fisch, Midas Rex, and Anspach drill systems. These drills generally are unsuitable for work in the middle ear, especially around the stapes footplate. For the latter purposes, a microdrill, such as the Skeeter drill or Synergy, is suitable (Fig. 1-5). Whatever drill is used in the middle ear, it must have a variable speed control and a wide array of drill bits.
Most larger otologic drills are equipped with straight and angled handpieces. Most surgeons prefer straight handpieces for early gross removal of the mastoid cortex, switching to angled handpieces for working deeper in the temporal bone. The Anspach drill system has a handpiece that can be converted from straight to angled simply by rotating the connection. A full complement of cutting and diamond burrs is mandatory. Figure 1-6 shows the Anspach drill system. Most drill systems have attachments that vary in shape, diameter, and length. It is the surgeon’s responsibility to be intimately familiar with the drill system and to have all of the attachments and burrs that might be needed.
The otologic drill should be held in the hand like a pencil, with the hand resting comfortably on the sterile field. The side of the burr should be used to provide maximum contact between the bone and the flutes of the burr, affording safer and more efficient drilling (Fig. 1-7). The newer drills are remarkably reliable, but, similar to other tools, may malfunction. Drill systems require proper care and inspection before use. A backup system should be readily available.
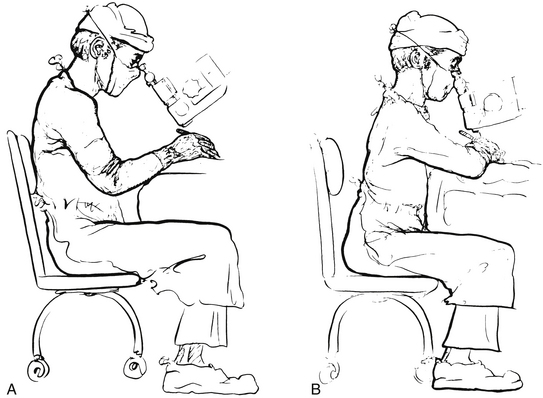
Proper posture at the operating table is crucial. To perform microsurgical procedures, rule number one is that the surgeon must be comfortable. The surgeon should be seated comfortably in a proper chair with the back support at the correct height. Both feet should be resting comfortably on the floor. Fatigue is avoided by assuming a restful position in the chair, rather than a rigid upright posture (Fig. 1-8).
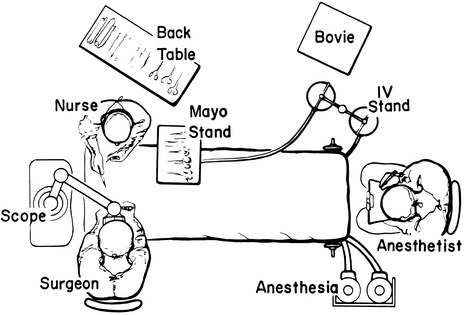
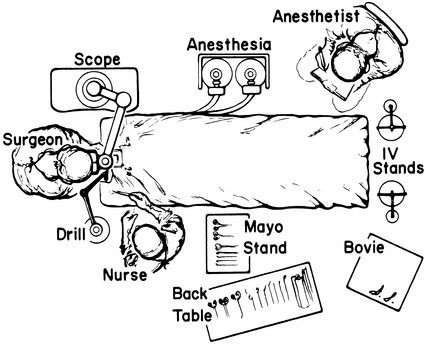
The overall OR setup for routine otologic surgery is shown in Figure 1-9. For neurotologic surgery, more space must be available for additional equipment. Middle cranial fossa procedures require some modifications to the OR setup (Fig. 1-10). Basically, the surgeon and the microscope trade places such that the surgeon is seated at the head of the table. Cooperation and careful orchestration between the surgeon, nursing personnel, and anesthesiologist are required for otologic surgery. The needs of the otologist are best served by having the anesthesiologist at the foot of the bed and the scrub nurse opposite the surgeon. Space for the facial nerve monitoring equipment and personnel is reserved.
STAPES SURGERY
About 30 minutes before the operation, the patient is brought to the preoperative holding area. If the surgeon routinely harvests a postauricular graft, this area is now shaved. A plastic aperture drape is applied to the operative site and trimmed so as not to cover the patient’s face (Fig. 1-11). An intravenous line is started, and the patient is now ready to go to the OR. When the patient is on the OR table, the monitors are placed on the patient by the nursing or anesthesia staff. Minimal monitoring includes pulse oximetry, automatic blood pressure cuff, and electrocardiogram electrodes. The ear and plastic drape are scrubbed with an iodine-containing solution, unless the patient is allergic to iodine. A head drape is applied, and the ear is draped with sterile towels so as not to cover the patient’s face; this can be facilitated by supporting the drapes with a metal bar attached to the OR table, or by fixing the drapes to the scrub nurse’s Mayo stand (Fig. 1-12).
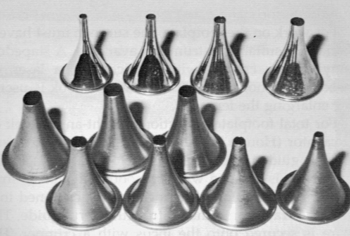
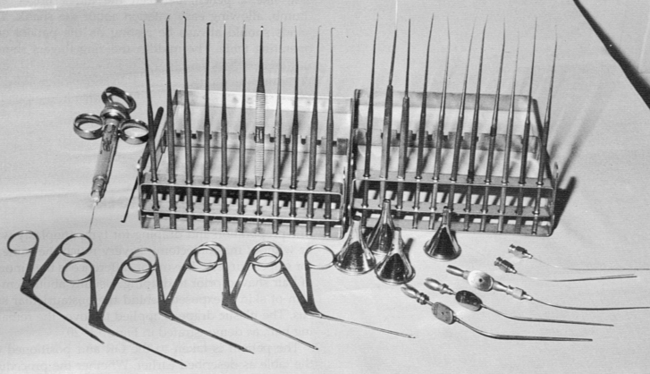
Various ear specula should be available in oval and round configurations. Sizes typically range from 4.5 to 6.5 mm (Fig. 1-13). It is desirable always to work through the largest speculum that the meatus permits, without lacerating canal skin. Some surgeons prefer to use a speculum holder for stapes and other middle ear procedures. The tympanomeatal flap is started with incisions made at the 6 and 12 o’clock positions with the No. 1, or sickle, knife. These incisions are united with the No. 2, or lancet, knife. This instrument actually undermines the vascular strip instead of cutting it. The strip is cut with the Bellucci scissors. The defined flap is elevated to the tympanic annulus with the large round knife, known as the large “weapon.” When properly identified, the annulus is elevated superiorly with the Rosen needle, and inferiorly with the annulus elevator, or gimmick. Figure 1-14 shows a typical set of stapes instruments, including suction tips.
Adequate exposure usually requires removal of the bony ledge in the posterosuperior quadrant. This can be initiated with the Skeeter microdrill and completed with a stapes curette (Fig. 1-15).
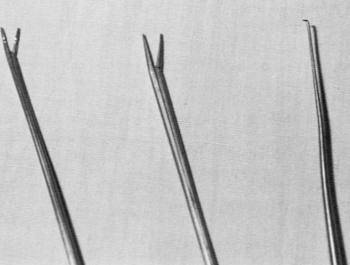
For total footplate extraction, a right angle hook or excavator (Hough hoe) is used. The harvested graft is guided into place with a footplate chisel. The prosthesis is grasped with a smooth alligator or strut forceps and placed on the incus. It is positioned on the graft, or into the fenestra, with a strut guide. The wire is secured onto the incus with a crimper, or wire-closing forceps. The McGee crimper is useful, especially if followed by a fine alligator forceps for the last gentle squeeze. A small right angle hook may be necessary to fine-tune the position of the prosthesis (Fig. 1-16).
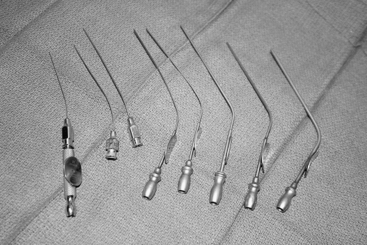
Suction tubes for stapes surgery include Nos. 3 to 7 Fr Baron suctions plus Rosen needle suction tips (18 to 24 gauge) with the House adapter (Fig. 1-17). The Rosen tips are useful when working near the oval window, with the surgeon’s thumb off the thumb port.
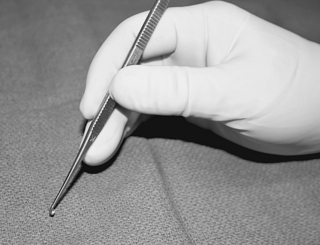
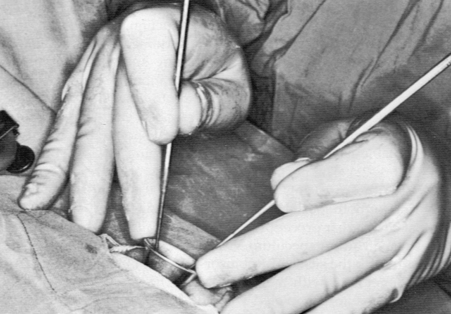
For all middle ear procedures, the surgeon should hold the instruments properly. The instrument should rest, like a pencil, between the index finger and thumb, allowing easy rotation around the shank. The hands should always be resting on the patient and the OR table. The middle and ring fingers should rest on the speculum so that the hand moves as a unit with the patient. Proper hand position and holding of instruments should afford the surgeon an unimpeded view (Fig. 1-18).
TYMPANOPLASTY AND TYMPANOPLASTY WITH MASTOIDECTOMY
The preparation and draping for tympanoplasty with or without mastoidectomy are much the same as for stapes surgery. The major difference is the amount of hair shaved before draping. Usually, enough hair is shaved to expose about 3 to 4 cm of skin behind the postauricular sulcus. The plastic drape is applied to cover the remaining hair (Fig. 1-19).
The patient is positioned on the OR table as described earlier. Whether the procedure is performed under local or general anesthesia depends on the extent of the surgery, the surgeon’s preference, and the desire of the patient. After appropriate sedation or induction of anesthesia, the ear and plastic drape are scrubbed with the proper soap or solution. Some surgeons place a cotton ball in the meatus if a perforation exists, preferring not to allow the preparation solution to enter the middle ear. The field is draped as described earlier, the head is rotated toward the contralateral shoulder, and the table is placed in slight Trendelenburg position (Fig. 1-20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree