Chapter 56 Petrosal Approach
Petroclival tumors arise from or involve the petroclival junction cephalad from the jugular tubercle, medial to the trigeminal nerve, and anteromedial to the internal auditory canal (IAC).1,2 Tumors of the petroclival area are a particular challenge because these tumors often involve the middle and posterior cranial fossae, cause significant brainstem compression, invade the cavernous sinus, and abut or surround the upper cranial nerves and basilar artery. The complex anatomy requires an individualized surgical approach for each patient based on tumor origin, area of tumor extension, and preoperative neural function.3
The term combined petrosal approach actually describes numerous surgical approaches to the petroclival area well suited for these tumors. The term combined refers to the fact that this approach combines the middle fossa approach with a variation of a posterior fossa approach. The combination of these approaches allows for excellent exposure of the medial petrous bone and clivus from the cavernous sinus to the foramen magnum. First described by Decker and Malis,4 this combination allows the surgeon to take advantage of the strengths of each approach to minimize brain retraction. The middle fossa approach gives the surgeon good exposure of the petrous bone and clivus superior to the IAC, whereas the posterior approach provides surgical exposure inferior to the IAC. A tumor that is superior to the IAC can be accessed by a middle fossa approach alone. A tumor that is inferior to the IAC and tentorium cerebelli can be addressed with a posterior approach alone. It stands to reason that tumors involving both areas are best treated with a combination of these surgical procedures.
COMBINED PETROSAL VARIATIONS
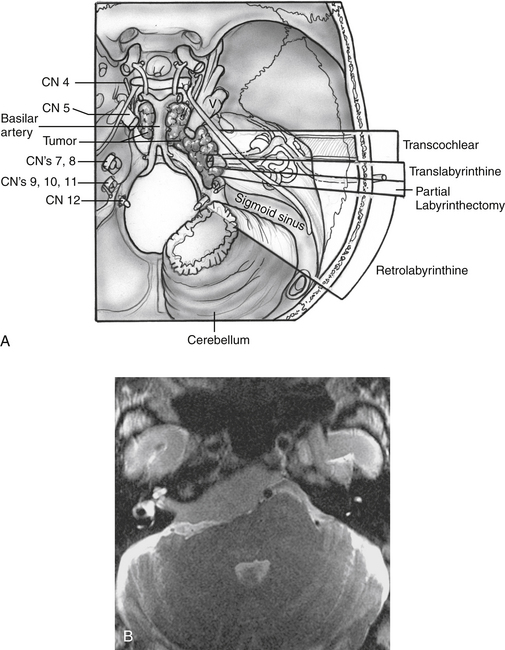
All of the combined petrosal approaches include similar middle fossa exposure as a component of the procedure. The variations of the combined petrosal approach are classified by the type of posterior approach used. Traditionally, three variations of the combined petrosal approach were described: the retrolabyrinthine, translabyrinthine, and transcochlear approaches.5,6 The fourth variation described by Sekhar and colleagues,7 which provides exposure in between the retrolabyrinthine approach and the translabyrinthine approach, uses a partial labyrinthectomy for the posterior approach. This approach removes most of the labyrinth, while preserving functional hearing in 80% of patients. These four approaches give different degrees of anterior petrous bone exposure, which changes the level of brainstem and clivus exposure. The narrow angle between the anterior brainstem and clivus is the major factor influencing the level of visualization across both of these structures. Generally, further anterior removal of the otic capsule allows a more direct angle across the clivus, allowing improved medial exposure to the brainstem, basilar artery, and central clival depression. More aggressive anterior otic capsule removal secondarily provides improved access to the ipsilateral medial petrous bone as well (Fig. 56-1A).
The choice of posterior approach depends on tumor location and size, preoperative hearing level, and extent of brainstem compression. The translabyrinthine and transcochlear approaches sacrifice residual hearing. The transcochlear approach also includes posterior facial nerve transposition, leading to a temporary facial paralysis and risking permanent injury. The translabyrinthine approach is used when preoperative hearing is poor, and the transcochlear approach is reserved for the largest of tumors that cross the midline of the clivus. Tumor effect on the brainstem is also an important consideration. Sometimes larger tumors need a less radical posterior approach because the posterior compression of the brainstem opens the angle between the clivus and brainstem. The tumor in Figure 56-1B was addressed with a translabyrinthine variation of the combined petrosal approach despite involvement of the contralateral clivus. The posterior displacement and contralateral displacement of the brainstem kept the angle between the tumor-involved clivus and brainstem open, obviating the need for a transcochlear approach.
PREOPERATIVE EVALUATION
Important temporal bone arterial and venous variations can often be detected from MRI; however, angiography with venous phase should be considered for each patient in whom a combined petrosal approach is being contemplated. Important venous anomalies exist that may result in catastrophe if not recognized before surgery.8 The main venous drainage of the temporal lobe is through the vein of Labbé, a single tributary that runs along the inferior surface of temporal lobe and typically anastomoses into the transverse sinus. The vein of Labbé may run through the tentorium, however, and insert into the superior petrosal sinus, rather than the transverse sinus. Because superior petrosal vein and tentorium transection is a key component of the combined petrosal approach, the vein of Labbé would be at risk if this anatomic variation is present. Accidental transection can lead to venous infarction of the temporal lobe with particularly grave consequences to the patient, especially if it occurs in the dominant hemisphere. A dominant sigmoid sinus should also be recognized before surgery. The surgeon must exercise extra caution not to injure a dominant sigmoid sinus because the contralateral venous drainage may be insufficient or absent, leading to a high risk of venous infarction.