Fig. 1016 Obliteration of the cavity using anorganic bovine bone behind a Palva flap and a fascia (Härmä and Koskinen). The ossiculoplasty is performed using a columella. Fascia is placed as an underlay graft, covering the lateral part of the Palva flap. Laterally, the granules are covered with Gelfoam
Ethylenediamine removes all the organic substances from the bovine cancellous bone, leaving only the inorganic material, closely resembling the currently used hydroxyapatite granules.
Obliteration with Methacrylate
As early as 1962, Mahony published on “tympanoacryloplasty,” i. e., filling the cavity with methacrylate. Meuser (1980, 1982, 1984) further elaborated on this method by filling the cavity with a nonresorbable methacrylate Sulfix-6 plastic material (manufactured by Sulzer Brothers, Winterthur, Switzerland). With a retroauricular approach, the epithelial lining of the cavity is carefully elevated, preserving as much of the skin as possible. The cavity walls are polished with a diamond burr, and an ossiculoplasty is performed. In order to separate the ear canal from the cavity, a large piece of autogenous conchal cartilage is placed on the medial wall of the attic (Fig. 1017), and the cavity is filled with methacrylate. The position of the cartilage is secured by fibrin glue. The methacrylate is made by mixing liquid and powdered components, and this mixture is put into a syringe and injected into the mastoid cavity behind the cartilage. It adapts precisely to the cavity. As it hardens, Sulfix-6 produces heat, which can be conducted away by irrigation with a cold saline solution for about eight minutes. Meuser (1982) called this material “plastic bone cement.” Early results using this method on 16 ears showed good healing, but in one ear subsequent reobliteration was required. As well as removal of a large piece of conchal cartilage, a meatoplasty is performed, thus widening the ear canal (Fig. 1017). The acrylic bone cement is not biocompatible, and acts in the long term as a foreign body. In the short term, however, the cement is able to plug the cavity effectively and prevent recurrent cholesteatoma.
No other surgeons have apparently used this method, and Meuser himself later used allogenous costal cartilage for obliteration of the cavity (Meuser 1989, 1993).
Ceramics
Ceramics are inorganic crystalline materials. Over the last 15 years, they have been used in otology, initially as an ossiculoplasty material, and over the last eight years as a material for reconstructing the ear canal wall and obliterating the cavity.
Some ceramics, such as alumina ceramics (Friolit and Bioceram, Vol. 1, pp. 289–291) are nondegradable and bioinert, having no biochemical influence on the surrounding tissue. These ceramics are used in ossiculoplasty.
Most ceramics are bioactive. They provoke bone formation on contact with the cavity walls. Calcium sulfate ceramic material (plaster of Paris) is used in obliteration, but it resorbs more rapidly as the newly formed bone appears. The calcium phosphate ceramics are used both in obliteration and ossiculoplasty. Porous tricalcium phosphate ceramics and calcium phosphate ceramics are used only in obliteration. They have a slow degradation rate, and are replaced after 12–18 months by newly formed bone.
Bone minerals consists of several calcium phosphate salts, of which the most important is hydroxyapatite. Together with calcium and phosphorous in serum, they form a dynamic equilibiium. Due to an interaction with hydroxyapatite (the calcium–phosphorous system), implants of calcium phosphate soon develop a thin layer of biological apatite, which forms a solid bond between the implants and the bony tissue of the host. Various calcium phosphate ceramics degrade in different ways, depending on their different crystal and chemical makeup, their structure, and the biological activity of the host tissue. Hydroxyapatite implants have shown good biocompatibility (Kuijpers 1984). The outcome of obliteration using pieces of resorbable tricalcium phosphate ceramics has not been conclusive (Zöllner and Brüssing 1986).
Glass ceramic contains silicon dioxide, which is a fine-grained material composed of alkaline silicates and calcium phosphate. Even though it is not degradable, it results in direct bone contact between the implant surface and the host bone through the leaching of calcium and phosphate ions. This material has been used in middle ear reconstructions, for example in Ceravital (Xomed) (Reck 1985).
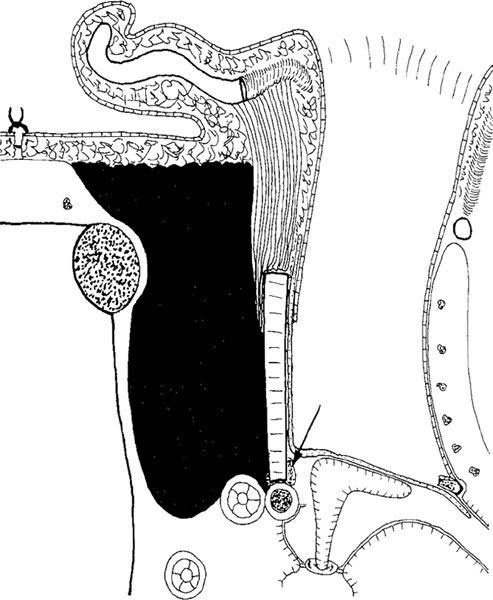
Fig. 1017 Obliteration of the cavity using methacry-late or plastic bone cement (Meuser). The ear canal wall is reconstructed using autogenous conchal cartilage, sealed to the bony cavity walls with fibrin glue (arrow). The Palva flap is placed laterally. The ossiculoplasty is performed with a columella. Fascia covers the drum perforation as underlay graft. Bone cement is placed behind the reconstructed ear canal. The conchal cartilage is removed, enlarging the ear canal
Plaster of Paris
Plaster of Paris is a biodegradable ceramic material prepared from calcium sulfate, which when mixed with water makes a paté that solidifies within minutes, producing a certain amount of heat as it does so. It is easily applied to the cavity, and its subsequent transformation into a firm block enhances the reconstruction of the posterior ear canal wall.
Plaster of Paris was occasionally used by orthopedic surgeons and dentists in the 1930s and 1940s, with variable results. In 1980, Coetzee obliterated the mastoid cavity using plaster of Paris behind a reconstructed ear canal wall made of allogenous septal cartilage.
In a series of experimental studies on guinea-pig ears, Högset and Bredberg established that plaster of Paris is gradually absorbed and incapable of thermal damage. The tissue response to plaster of Paris in guinea-pig bullae is as benign as that to autologous bone, indicating excellent biocompatibility (Högset and Bredberg 1986). It does not damage the inner ear or cause sensorineural hearing loss (Högset and Bredberg 1988). It has a bone-stimulating capacity, and the bone formed in its presence has a normal structure. Four to six milliliters of plaster of Paris are needed to obliteratate a radical mastoidectomy cavity that does not exceed the physiological range.
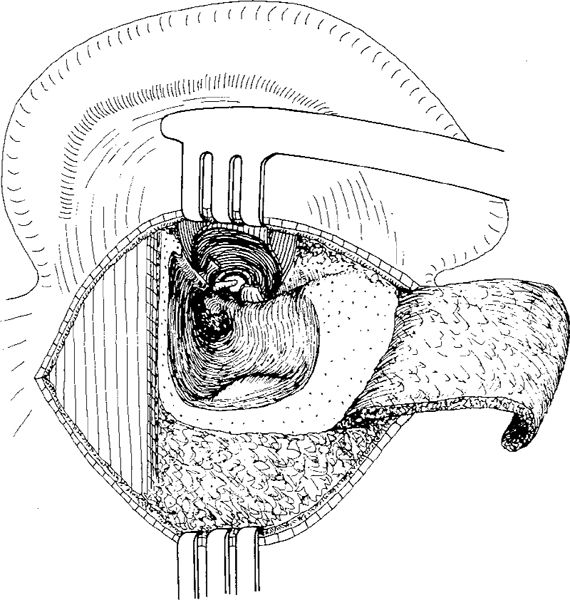
Fig. 1018 Obliteration of the cavity using plaster of Paris (Högset and Bredberg). An inferiorly-based subcutis–muscle–periosteum flap is raised, inferior and superior ear canal skin flaps are elevated, and a canal wall–down mastoidectomy is performed
The following technique has been used in 20 patients (Högset and Bredberg 1992). With a retroauricular incision, an inferiorly-pedicled flap is raised from the periosteum, muscle, and subcutaneous tissue overlying the mastoid cortex (Fig. 1018). The flap is later rotated into the external ear canal. The meatal skin is elevated and displaced anteriorly, creating inferior and superior ear canal skin flaps, as well as a lateral flap. After removal of the pathological lining of the mastoid cavity and polishing of the cavity walls, the ear canal wall is reconstructed. Along the superior cavity wall and the facial ridge, grooves are made in order to place pieces of cortical bone tightly in position. One to three large pieces of cortical bone are used to reconstruct the ear canal wall. The new bony meatal wall is fixed posteriorly with plaster of Paris, easily injected with a syringe because of its initial fluid, paté-like state (Fig. 1019). Approximately 4–6 ml are used to obliterate the cavity (Fig. 1020). The bony defect in the mastoid surface is covered with pieces of cortical bone supported by the plaster (Fig. 1021). After ossiculoplasty, the perforation is closed with a large fascial graft extending over the reconstructed ear canal wall, as well as the musculoperiosteal flap (Figs. 1022, 1023).
Postoperative follow-up of 20 patients for at least one to five years (mean three years) after surgery revealed slight discharge from one ear; the rest were dry. Six patients developed retractions located posterolaterally in the ear canal close to the auricle. In one patient, pieces of bone and plaster of Paris, as well as a protruding bony rim, were removed postoperatively. The five patients with persistent retraction underwent revision surgery during the first two years. It was found that the lateral retractions corresponded to small defects in the most lateral part of the reconstructed posterior bony ear canal wall. The reconstructed bony ear canal wall had grown thicker, except laterally. It was also shown that the plaster of Paris had totally disappeared in three cases which were revised within eight months, and the mastoid cavity was partly obliterated by bony tissue. Thirty-seven percent of patients maintained an ear canal of normal size postoperatively, 40% had a widened ear canal, and 25% developed cavities. Högset and Bredberg consider that filling the mastoid cavity with plaster of Paris solves the problem of fixation of the autogenous bone when reconstructing the ear canal wall. Plaster of Paris stimulates bone formation, but is resorbed and only partially replaced by bone. The problem of progressive and potentially dangerous retraction behind a firmly reconstructed ear canal wall, — described by the authors at follow-up, would therefore appear to be unavoidable.
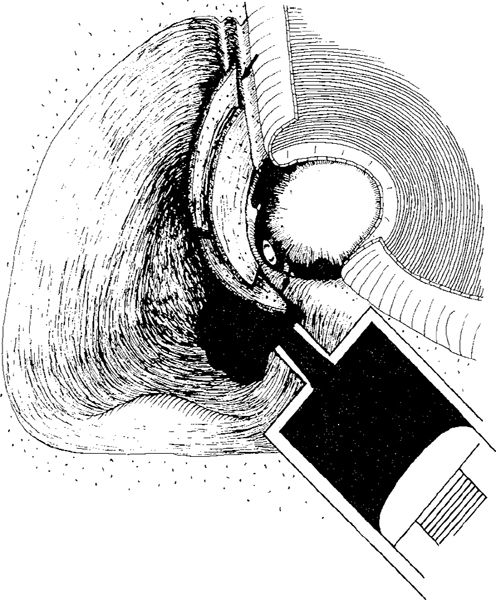
Fig. 1019 The ear canal wall is reconstructed with one to three curved pieces of bone placed in a groove drilled along the zygomatic root and facial ridge (arrows) into the cavity. The pieces of bone are fixed with plaster of Paris introduced into the cavity with a syringe
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


