CHAPTER 53 Management of the Frontal Sinuses
Acute Frontal Sinusitis
Frontal sinusitis can be complicated by periorbital cellulitis or the formation of a periorbital abscess. The indications for an urgent computed tomography (CT) scan are the presence of signs of central nervous system involvement, inability to assess vision accurately, gross proptosis, ophthalmoplegia, deteriorating visual acuity or color vision, bilateral edema, no improvement or deterioration after 24 hours, and a spiking pyrexia not resolving within 36 hours.1 Intracranial complications include a subdural empyema, intracerebral abscess, extradural abscess, meningitis, and, more rarely, cavernous and superior sagittal sinus thrombosis. It is important to be aware that almost 50% of patients with intracranial complications present with a periorbital cellulitis or frontal swelling. Therefore it does not follow that a collection of infection that spreads around the orbit excludes any intracranial involvement.2 It is important to look for the symptoms or signs of intracranial involvement—namely, an altered mental state, headache, vomiting, seizure, neck stiffness, papilledema, unilateral weakness, and signs of cranial nerve involvement. If there is intracranial involvement, sinus surgery has a role in obtaining pus for culture as well as draining the collection if the sinus is in continuity with the intracranial collection.
Chronic Frontal Sinus Disease
Jurasz was the first surgeon to describe an intranasal approach to the frontal sinus. Ogston3 in the late 1880s and Luc4 in the next decade described trephination and widening of frontonasal duct through the anterior ethmoid sinuses. Brieger5 first described the osteoplastic operation in the 1890s. Riedel6 described a technique in 1889 wherein he removed its anterior and inferior walls. This technique resulted in a cosmetic deformity that would require a second operation if an improvement in cosmesis was sought. In 1908 Knapp7 advocated an extensive ethmoidectomy through the medial orbital wall, leaving the anterior wall of frontal sinus intact but removing the diseased mucosa and enlarging the frontonasal duct. Lothrop8 in 1912 resected the frontal floor between the frontal recesses and the intersinus septum along with the upper aspect of nasal septum after an ethmoidectomy via an external approach as described by Lynch. By 1921 Lynch9 and Howarth10 had surgically entered the frontal sinus through an external approach via the medial orbital wall and, like Knapp, removed sinus mucosa and left a stent in position to try to maintain a patent duct. The osteoplastic flap with fat obliteration then became popular for the treatment for persistent frontal sinus disease. Macbeth11 and Bosley12 later postulated that fat obliteration is not necessary, as they claimed that the cavity is filled by osteoneogenesis. However, I and others have found that, unless the frontal sinus is obliterated in this procedure, loculated areas within the sinuses are more likely to form, which may become infected or form mucoceles.
In the medical treatment of bilateral chronic rhinosinusitis without purulent secretions, there is growing evidence that some antibiotics work not only through their antibacterial action but also by down-regulating inflammation.13 Long-term (12 weeks to 6 months), low-dose therapy with erythromycin, clarithromycin, and other macrolides along with douching has been shown to be beneficial.14 The efficiency with which an antibiotic disperses biofilms may also be of importance.
Indications for Surgery in Chronic Frontal Sinusitis
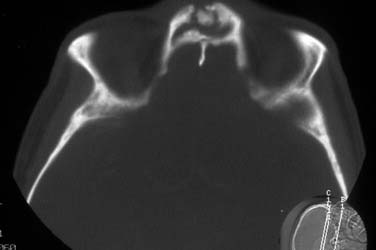
There are few other reasons for operating on the frontal recess before trying a partial anterior ethmoidectomy along with medical treatment; these reasons include the presence of fungal disease in the frontal sinus, barotrauma, mucocele (Figs. 53-1 to 53-3), an osteoma causing obstruction with evidence of mucosal disease, and other pathology, such as osteomyelitis (Fig. 53-4) and tumors.

Figure 53-3. Postoperative view of patient in Figure 53-1 after endoscopic marsupialization of the right frontoethmoid mucocele.
The normal frontal recess is narrow, raising a question as to the role of anatomic variations in the pathogenesis of rhinitis. The frequency of such “variations” and anatomic “restrictions” appears to be no higher in a control population than in a patient with proven rhinosinusitis.15 It seems likely that the primary problem is the mucosal pathology or a patient’s immunity—the reason why one individual experiences chronic rhinosinusitis and another does not.
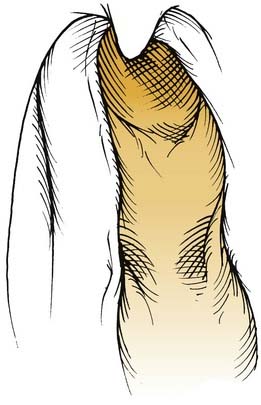
The variability of the anterior ethmoid air cells makes them a fascinating subject on their own. In more than 94% of people there are anterior ethmoid air cells over the lacrimal bone or adjacent to the anterior aspect of the middle turbinate; these are called agger nasi cells. A high anterior ethmoidal cell that has pneumatized into the frontal bone, known as the bulla frontalis, can displace the frontal recess posteriorly and medially. The bulla frontalis can be so large that it can mimic the frontal sinus, almost forming a sinus within a sinus. Not infrequently a supraorbital cell—that is, a posterior cell in the anterior ethmoid complex that is well pneumatized—can extend laterally into the frontal bone over the orbit and also can narrow the frontal recess by pushing it forward. Occasionally air cells exist within the frontal sinus itself, the ostia of these cells draining within the frontal sinus.16 Another variation is the intersinus septal cell that may extend into the crista galli; this cell often drains into the frontal recess. The prevalence of these variations does not appear to correlate with the presence or absence of frontal sinus disease.
Endoscopic Frontal Sinusotomy
One method of accessing the frontal recess involves removing the superior remnant of the uncinate process with a 45-degree through-cutting forceps or a punch. A 45- or 70-degree endoscope is then used to examine the area. Careful palpation, not prodding, with a ball probe next to the middle turbinate reveals a crevice between the middle turbinate and the agger nasi cells. The aim is to open this crevice, which will turn out to be the pathway to the frontal recess and the frontal sinus, by “deflating” the cells. This is best done by passing the ball probe well above them and gently fracturing them to one side. The shaft of a Kuhn curette works well for this maneuver (Figs. 53-5 and 53-6). If visibility is good, it may be possible to do this by submucosal dissection. Fragments of bone are removed, with care taken not to grab the mucosa, because doing so might leave bone exposed and predispose to scar tissue and stenosis.
When they are opened, agger nasi cells, the terminal recess, and the ethmoid bulla can all form concave domes of a variable size and give the appearance of the frontal sinus, but the sinus itself has a convex posterior surface that is distinctive. It is possible to confirm that an instrument is actually in the frontal sinus by using a ball probe, a Kuhn curette, or a curved sucker as a sound, passing it into the area in question and then registering the angle and length of this ball probe in relation to the maxillary spine. To ensure that the instrument is within the frontal sinus, the surgeon can grip the shaft of the ball probe between the thumb and the index finger next to the nasal spine, noting the angle of the instrument at the same time. The surgeon then withdraws the instrument and places it alongside the outside of the nose, at the same angle it had in the sinus and with the pinch grip placed alongside the nasal spine (Figs. 53-7 and 53-8). If the end of the ball probe is then higher than the eyebrow line, the instrument was probably in the frontal sinus. If the instrument is around or just above the medial canthus, then the ball probe is likely not within the frontal recess but is within an agger nasi cell. If the handle of the ball probe is noted to have been turned laterally when it passes up through what is thought to be the frontal recess, it may have been channeled in this direction by a bulla frontalis or a supraorbital cell, and the surgeon should correlate this possibility with the CT scan.

Figure 53-7. Confirming location of instrument in the frontal sinus. The surgeon “pinches” the instrument against the maxillary spine, noting the angle of the instrument. (See Figure 53-8.)

Figure 53-8. Confirming location of instrument in the frontal sinus (see Figure 53-7). The surgeon then aligns the instrument outside the nasal airway at the same angle, keeping the fingers at the same place on the instrument against the nasal spine. If the end of the probe is well above the medial canthus, it is likely to be within the frontal sinus when reinserted. (The exception is a large bulla frontalis, presence of which can be checked for on the computed tomography scan.)
Lynch-Howarth External Ethmoidectomy
The Lynch-Howarth external ethmoidectomy has largely been replaced by endoscopic techniques because stenosis developed in approximately a third of patients who underwent the procedure.17,18 An external scar, the necessary loss of bone lateral to the frontal recess, and loss of mucosa often result in scar tissue and stenosis of the frontal recess.
It is possible to support and reconstruct the lateral wall of the frontal recess to prevent its collapsing or to deal with collapse of that area. The problematic circumstances affecting this area are large mucoceles and previous surgery in the area, particularly when an external ethmoidectomy has led to a loss of bone lateral to the frontal recess (Fig. 53-9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree