27 Learning from Two Difficult Cases: Transmaxillary Approaches to the Pterygopalatine Space Prior to advances in instrumentation for endoscopic sinus surgery, access to the middle cranial skull base behind the maxillary sinus was difficult, often involving facial incisions and/or neurosurgical access. Disease processes ranging from cerebrospinal fluid (CSF) leak, infections, and various neoplasms are occasionally found in anatomic spaces behind the posterior wall of the maxillary sinus, including the pterygopalatine space (PPS) and the lateral sphenoid recess (LSR), a pneumatization of the sphenoid sinus lumen into the pterygoid root. Traditional approaches to the retromaxillary spaces include midfacial degloving or lateral rhinotomy with medial maxillectomy, Caldwell–Luc, and subtemporal craniotomy. Endoscopic transmaxillary approaches with image guidance provide a superior visualization while being less invasive and more aesthetically favorable. The special anatomic relationship of the PPS and the LSR allow endoscopic approaches to these regions through the posterior wall of maxillary sinus and indications for endoscopic techniques continue to broaden. This chapter will illustrate surgical techniques of transmaxillary approaches to the PPS as adaptations of those previously described for the LSR. The posterior wall of the maxillary bone articulates medially with the palatine bone. The PPS is a small space bounded anteriorly by these structures and posterosuperiorly by the sphenoid. The PPS has free connections to the orbit, palate, skull base, infratemporal fossa, and nasal cavity, thus providing a path of least resistance to various disease processes. The sphenopalatine foramen, found between sphenoid and palatine bone, contains the sphenopalatine artery, which is the main blood supply to the posterior nasal cavity. The inferior orbital fissure, at the junction of sphenoid and maxillary bone, opens to the orbital floor and transmits the distal branch of the maxillary nerve as the infraorbital nerve. Transmaxillary approaches offer access to the extradural skull base up to the foramen rotundum (containing the maxillary nerve) and pterygoid canal (containing the Vidian nerve). The pyramidal process of the palatine bone makes up the floor with its greater and lesser palatine foramina as the communications of the PPS inferiorly (Table 27.1).1 Occasionally, pneumatization of the lateral portion of the sphenoid bone, either the greater wing or the pterygoid process, occurs forming an LSR. This is observed in up to 25 to 48% of patients2 and is extensively pneumatized in 8% of cases. In this case, the roof of the sphenoid sinus lies directly beneath the middle cranial fossa and temporal lobe. Defects in the skull base in the LSR or the infratemporal fossa can be accessed via transmaxillary approaches as well.
 Anatomy
Anatomy
Foramina/Fissures | Location within PPS | Contents |
|---|---|---|
Inferior orbital fissure | Anterosuperior wall (roof) | Infraorbital nerve |
Pterygomaxillary fissure | Lateral wall | Internal maxillary artery |
Sphenopalatine foramen | Medial wall | Sphenopalatine artery |
Greater palatine foramen | Floor | Greater palatine nerve/artery |
Lesser palatine foramen | Floor | Lesser palatine nerve/artery |
Pterygoid canal | Posterior wall | Vidian nerve |
Foramen rotundum | Posterior wall | Maxillary nerve |
 Pathology That May Be Encountered in the Pterygopalatine Space
Pathology That May Be Encountered in the Pterygopalatine Space
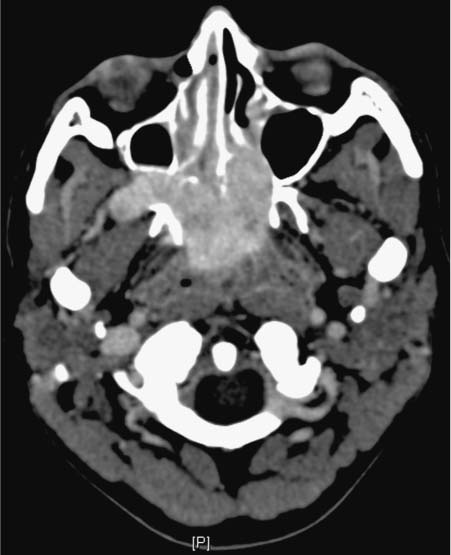
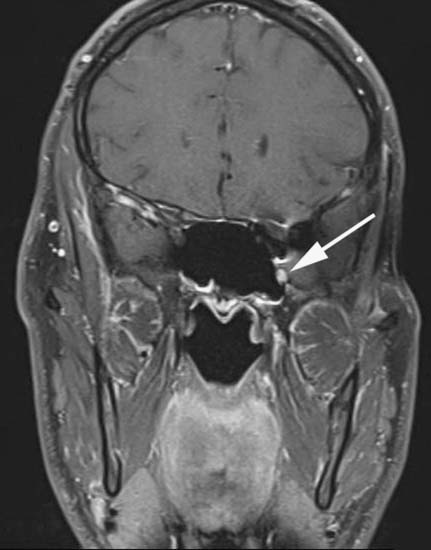
Juvenile nasopharyngeal angiofibroma (JNA) is the most common lesion in the PPS. It is thought to originate from the aperture of sphenopalatine foramen. Although a benign neoplasm, it is a locally invasive and a high vascular tumor. Radiologically, the pathognomonic sign is the Holman–Miller sign, where there is an anterior displacement of the posterior wall of maxillary sinus wall due to mass (Fig. 27.1). Angiography is performed to evaluate for the feeding vessel, the most common vessel being the branches of internal maxillary artery. For smaller tumors, an endoscopic approach is ideal.3,4 Schwannoma is another lesion that can involve the maxillary division of the trigeminal nerve in the PPS. It is a slowly growing tumor and they can expand through thin parts of bone and widen the natural ostium (Fig. 27.2). Traditionally, these tumors in the PPS were removed through lateral rhinotomy or facial degloving approach. In a benign mass where en bloc resection is not necessary, endoscopic surgery is well suited.5 Other pathologies such as mucocele, invasive fungal infection, lymphoma, and inverting papilloma can extend to the PPS as well. Biopsies can be performed to confirm diagnoses of such conditions, and formal surgical resection may be indicated.
Fig. 27.1 Computed tomography scan of sinus, axial cut showing right-sided juvenile nasopharyngeal angiofibroma in the pterygopalatine space, displacing the posterior wall of the maxillary sinus anteriorly.
Fig. 27.2 Computed tomography scan of sinus, coronal cut showing right-sided schwannoma widening foramen rotundum (arrow).
Rarely, the temporal lobe can herniate into the PPS or LSR through a congenital or traumatic skull base defect, causing CSF rhinorrhea, recurrent meningitis, and possibly seizures. Traditionally, several invasive measures were used such as anterior subtemporal craniotomy or facial degloving. Bolger et al popularized the transpterygoid approach to the LSR and described this in detail through cadaver studies.6 Bolger and Osenbach reported six patients treated for encephalocele of the LSR endoscopically with up to 25-month follow-up, without recurrence or significant complications.7 Transmaxillary access to the PPS is an adaptation of these approaches to the LSR, involving removal of the ascending process of the palatine bone and posterior maxillary sinus wall via a wide antrostomy.
Fig. 27.3 Magnetic resonance image of the neck, coronal cut showing left enlargement V2 nerve, in recurrent adenoid cystic carcinoma of lacrimal gland with perineural invasion (arrow).
Occasionally, tumors spread beyond the bony confines of the PPS via the previously described foraminal portals. A classic example of this is reflected by perineural invasion by adenoid cystic carcinoma, which can track intracranially along nerves of the cavernous sinus wall. The palatine branch of the maxillary nerve innervates the mucosa of the hard palate, which contains many minor salivary glands and can also harbor neoplasm. As tumors pass through foramina, they enlarge these bony openings, creating a characteristic appearance on imaging studies (Fig. 27.3).8
 Surgical Technique
Surgical Technique
The two cases presented (see Videos 27.1 and 27.2) illustrate the transmaxillary approach to the pterygopalatine space. Case 1 describes a patient with a history of lacrimal adenocarcinoma previously treated with orbital exoneration, chemotherapy, and radiation. He presented with lip numbness, and MRI suggested perineural recurrence along the second division of the trigeminal nerve. After consultation with the multispecialty tumor board, excisional biopsy was advocated. This was performed via a transmaxillary approach to the pterygopalatine space through a wide maxillary antrostomy, takedown of the palatine process and posterior maxillary wall, and identification of the neural foramen and canal in the posterior-superior compartment of the space. Case 2 presents a patient with cerebrospinal fluid rhinorrhea whose preoperative imaging revealed a large meningocele arising from the left temporal region, filling the pterygoid space posterior to the pterygoid plate, splaying the pterygoid plates. This was accessed via a transmaxillary approach to the pterygopalatine space through a wide maxillary antrostomy, takedown of the palatine process and posterior maxillary wall, and identification of the attenuated bone of the pterygoid root. Opening of the latter layer of bone exposed the meningocele sac, which was resected and decompressed. The defect was closed with a fascia lata flap and bulk from the flap was also utilized to obliterate dead space in the pterygoid and pterygopalatine spaces.
When approaching the pterygopalatine fossa, depending on the pathology, it may be prudent to anticipate the need for transfusion, given proximity to the internal maxillary arterial system and pterygoid plexus of veins. Preoperative angiography and embolization is necessary in certain cases such as JNA. Neurosurgical consultation is a significant consideration, particularly in the setting of encephalocele or CSF leak. MRI and CT should both be obtained and image-guided surgical navigation is useful intraoperatively.
The usual preparations for the endoscopic sinus surgery are undertaken. Nasal cavities are topically vasoconstricted and anesthetized with pledgets soaked with 4% cocaine and oxymetazoline. Needle injection with 1% lidocaine with 1:100,000 epinephrine is applied to the axilla of the middle turbinate and the region of the sphenopalatine foramen. Intraoral injection of the greater palatine foramen can also be employed.
Zero-degree telescopic visualization is utilized throughout the initial stages of the dissection. First, uncinectomy is done, and middle meatal antrostomy is performed through the natural ostium. This is enlarged posteriorly into the region of the posterior fontanel using through-cut forceps as well as a microdebrider. A wide antrostomy is the first key to the procedure. For extended lesions, anterior and posterior ethmoidectomy may be required with identification of the skull base in the posterior ethmoid. Then sphenoidotomy is begun by identifying the root of the superior turbinate, followed by resection of the lower third of the turbinate body to expose the rostrum. The natural ostium will be posterior and just medial to the resected portion of the turbinate body. The sphenoid is entered using a curette and the ostomy is enlarged using a combination of Kerrison forceps, as well as through-cut forceps and/or the microdebrider. The sphenoidotomy is lowered toward the floor of the sinus. During this maneuver, it is often necessary to control the posterior septal branch of the sphenopalatine artery, which courses along the rostrum inferior to the sphenoid os.
The mucosa is then elevated in a submucoperiosteal plane, from the posterior wall of the maxillary sinus. Next, using the 4-mm diamond choanal atresia burr, the ascending process of the palatine bone, as well as the bone from the posterior wall of the maxillary sinus is removed, thus opening the anteromedial walls of the PPS. The sphenoidotomy is enlarged laterally and brought into communication with the soft tissue of the sphenopalatine foramen and medial pterygopalatine space. Using a combination of the drill, and Blakesley and Kerrison forceps, the opening into the posterior wall of the maxillary sinus is further enlarged laterally to expose the soft tissue in the pterygopalatine space. Angled telescopes (30- and 45-degree) are useful in this process, but occasionally, it is necessary to perform a Caldwell–Luc antrostomy to augment lateral access from an anterior trajectory. One should recall the pathologic process can significantly thin the posterior wall. Branches from the internal maxillary artery in the pterygopalatine space should be identified and bleeding controlled using electrocautery and/or surgical clips. Dissection using endoscopic microscissors through the pterygopalatine space fat can be performed to tease vascular branches away from the area of pathology, which can be confirmed with stereotactic correlation.
Dissection should proceed from inferomedial to superolateral until the foramen rotundum is encountered. The nerve within the foramen rotundum can be identified. Using an elevator, dissection can proceed in a subperiosteal plane along the uppermost aspect of the pterygoid root. If further dissection is necessary, the diamond drill can be utilized to remove bone along the medial hemisphere of the foramen rotundum, allowing dissection of the nerve along the body of the lateral sphenoid wall to the point of the cavernous sinus. Adequate biopsy specimen or resection of mass concludes the procedure.
Additional visualization in the region of the internal maxillary arterial branches should confirm hemostasis in this location. A small amount of absorbable hemostat can be placed over cauterized areas or venous plexi. In patients with defects of the floor of the middle cranial fossa, grafts are utilized to reconstruct the defect, support the temporal lobe, and obliterate the dead-space in the PPS. The displaced mucosa of posterior maxillary wall is then redraped; in cases where a CSF leak or cranial base defect was repaired, it is necessary to bolster the closure with a pack or Foley balloon within the maxillary sinus.
 Conclusion
Conclusion
The literature describes multiple alternatives for the management of lesions behind the posterior maxillary sinus wall, including JNA, schwannoma, carcinoma with perineural invasion, and CSF leak with meningocele.9,10 Here we illustrated how management of these pathologies can be successfully and safely accomplished through an endoscopic maxillary antrostomy. In our experience, the use of image guidance and meticulous exposure are critical to the procedure.
To accomplish the meticulous exposure, the following are needed:
• Wide antrostomy
• Identification of the orbital process of the palatine bone
• Control of internal maxillary arterial branches
• Use of a drill, when necessary, to address dense bone of the pterygoid root
• Consideration of a Caldwell–Luc if enhanced lateral exposure is required