CHAPTER 171 Intratemporal Facial Nerve Surgery
Surgical Anatomy
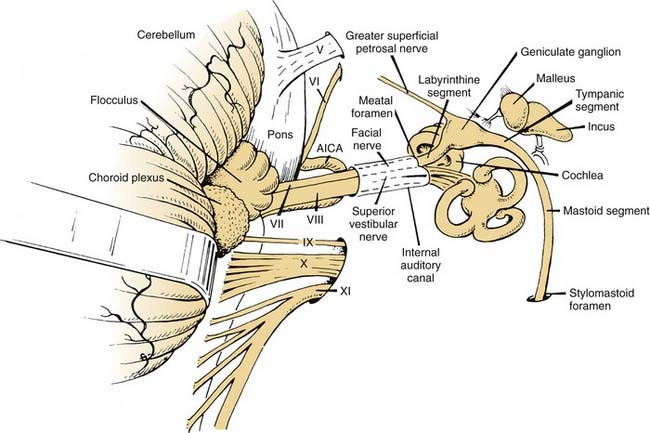
Thorough knowledge of the intricate, convoluted course of the facial nerve and its anatomic relationship to other vital structures is essential to the surgeon who plans to operate in this area. The facial nerve (cranial nerve VII) exits the brainstem at the pontomedullary junction approximately 1.5 mm anterior to the vestibulocochlear nerve (cranial nerve VIII). The facial nerve is smaller in diameter (approximately 1.8 mm) than the oval cranial nerve VIII (approximately 3 mm in the longer diameter). A third, smaller nerve, the nervus intermedius, emerges between cranial nerves VII and VIII and eventually becomes incorporated within the sheath of cranial nerve VII. After leaving the brainstem, cranial nerve VII follows a rostrolateral course through the cerebellopontine cistern for 15 to 17 mm, entering the porus of the internal auditory canal of the temporal bone (Fig. 171-1). Other important structures in the cerebellopontine cistern include the anterior inferior cerebellar artery (AICA) and the veins of the middle cerebellar peduncle. The AICA passes near or between cranial nerves VII and VIII; the veins are more variable in position and number. On entering the IAC, the facial nerve occupies the anterosuperior quadrant of this channel for 8 to 10 mm. Then it enters the fallopian canal at the fundus of the internal auditory canal. The internal auditory canal is anterior to the plane of the superior semicircular canal, with which it subtends an angle of approximately 60 degrees. At the entrance of the fallopian canal (meatal foramen), cranial nerve VII narrows to its smallest diameter, 0.61 to 0.68 mm.1 Only the pia and arachnoid membranes form a sheath around the nerve at this point, because the dural investment terminates at the fundus of the internal auditory canal. Some investigators2,3 identify the small diameter of the meatal foramen as an important contributory etiologic factor in facial paralysis associated with certain diseases, such as Bell’s palsy and Ramsay Hunt syndrome.
General Surgical Technique
Whenever the facial nerve is to be surgically exposed, several technical principles should be observed. First, a system for monitoring facial nerve function during the operation should be used.4 One of the simplest monitoring methods is visual observation during critical stages of the operation. Needle electromyography also can be used if the equipment is available. No matter which monitoring technique is used, it is essential that the side of the face on which the nerve is to be exposed be draped in a manner that allows visual observation. The patient’s forehead, eye, mouth, and chin should be visible. The endotracheal tube should be secured to the opposite side without taping on the side of the mouth to be observed. Towels drape the posterior, superior, and inferior margins; a fourth towel is placed along the anterior profile. An abdominal transparent plastic drape is placed over the face and operative area (Fig. 171-2). An observer can thus see the entire face during the procedure and determine whether any of the muscles move in response to surgical manipulation of the nerve. If the surgeon asks for observation during critical periods of the procedure, the circulating nurse is the best observer.
More precise intraoperative monitoring can be achieved using commercially available needle electromyographic systems (Fig. 171-3). Electromyographic needles are placed in the orbicularis oculi and orbicularis oris muscles, as shown in Figure 171-4. Stimulation of the facial nerve during the operation provides accurate localization of the nerve if the anatomy is distorted by a disease process or congenital abnormality. Constant current or constant voltage stimulators can be used. These systems allow auditory monitoring of facial nerve activity and alert the surgeon when the nerve has been stimulated. Auditory monitoring is especially useful during the removal of tumors adjacent to the facial nerve.
Surgical Approaches
Retrolabyrinthine Approach: Brainstem to Internal Auditory Canal Porus
Technique
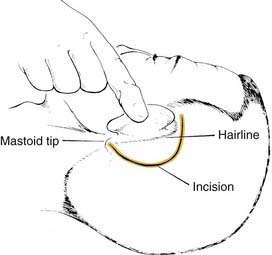
The patient is positioned on an operating table similar to that used for a mastoidectomy. Endotracheal anesthesia is administered, and the anesthetist is positioned at the foot of the table, allowing the surgical nurse to be opposite the surgeon. The hair is removed 4 cm superiorly and postauricularly, and the ear and the left lower abdominal quadrant (for the harvest of fat if necessary) are prepared and draped. An osmotic diuretic (250 mL of 20% mannitol) is administered intravenously at the start of the skin incision. The skin incision is made in the hairline 3 to 4 cm posterior to the postauricular crease and extended down over the mastoid tip (Fig. 171-5). Posterior placement of the skin incision provides access for occipital bone removal, which is necessary for posterior retraction of the sigmoid sinus.5
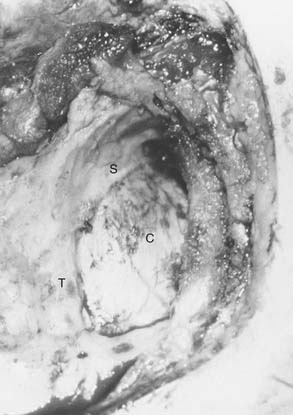
A complete mastoidectomy is performed. In addition, bone is removed over the sigmoid sinus from the sinodural angle to its most inferior extent. The dome of the jugular bulb also is identified. A large diamond burr and suction-irrigation are essential to prevent injury to the sinus and the posterior fossa dura. The cerebellar plate is removed from the tegmen mastoideum to the jugular bulb. Anteromedially, the posterior semicircular canal is identified, and inferior to the labyrinth (retrofacial area) the endolymphatic sac is exposed (Fig. 171-6). In a well-aerated mastoid, 2 to 3 mm of bone can be removed between the posterior semicircular canal and the cerebellar dura with the use of small diamond burrs. If the posterior canal is not evident, it should be blue-lined to locate its exact position.
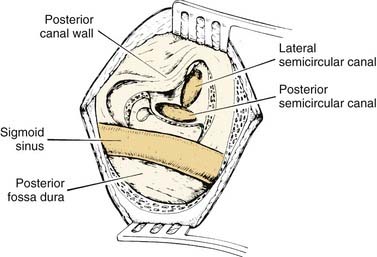
Figure 171-6. Exposure obtained through the left retrolabyrinthine approach before retraction and dural incision, as viewed by the surgeon.
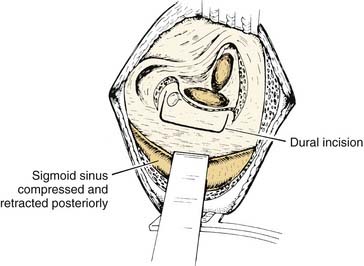
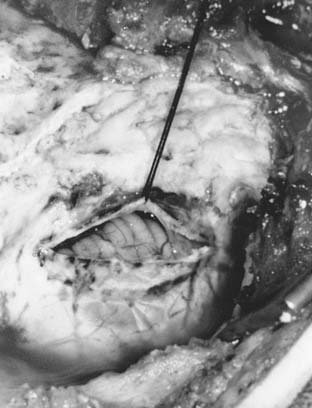
An anteriorly based trapdoor cerebellar dural flap is fashioned with a sharp microscalpel and microscissors (Fig. 171-7). Care should be taken not to injure the small cerebellar arachnoid vessels when the dura is opened. A cuff of dura should be left adjacent to the bony margins, sigmoid sinus, and superior petrosal sinus for placement of sutures during closure. Sutures placed at the corners of the dural flap serve to retract it anteriorly. A malleable self-retaining retractor is used to retract the sigmoid sinus posteriorly. The cerebellum usually falls away from the temporal bone, and minimal, if any, retraction is required. Hyperventilation, in addition to an osmotic diuretic, is useful in obtaining brain shrinkage.
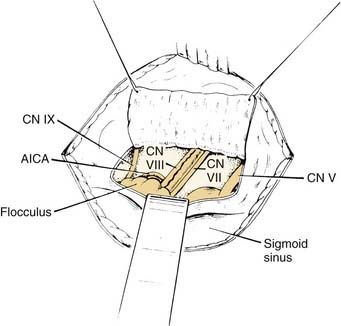
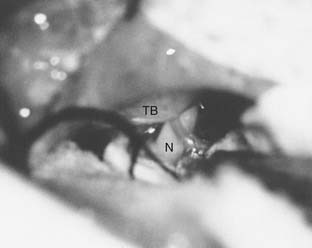
The cochleovestibular facial nerve complex is seen 2 to 3 mm inferior and parallel to Donaldson’s line (a line extending posterior from the plane of the lateral semicircular canal). The arachnoid is incised sharply, releasing the cerebrospinal fluid (CSF) from the cistern. Other visible nerves are the trigeminal nerve (cranial nerve V) superiorly and the glossopharyngeal nerve (cranial nerve IX) and possibly the vagus nerve (cranial nerve X) inferiorly (Fig. 171-8). Visualization of cranial nerve VII may be completely blocked by cranial nerve VIII. Cranial nerve VII usually arises 1.5 mm directly anterior to cranial nerve VIII. A Buckingham mirror aids identification of the facial nerve. The rostral division of the AICA may pass between cranial nerves VII and VIII, along with one or more veins. Approximately 15 mm of the nerve can be inspected in the cerebellopontine cistern.
Retrosigmoid Approach
Technique
Another option for exposure of the facial nerve from the brainstem to the internal auditory canal is through a small retrosigmoid craniotomy. The preparation and incision are similar to those in the retrolabyrinthine approach (see Fig. 171-5). Instead of a complete mastoidectomy, the bone over the sigmoid sinus is removed to identify the posterior margin of the sinus. Bone is removed 4 cm posterior to the sigmoid sinus, exposing the posterior fossa dura (Fig. 171-9). The outline of the transverse sinus is exposed superiorly. A curvilinear incision in the posterior fossa dura is created to expose the cerebellum (Fig. 171-10). Care is taken to incise the dura without injuring the arteries and veins on the cerebellum. Cottonoid sponges lined with rubber glove strips are placed on the cerebellum. Slow, gentle retraction of the cerebellum over 5 to 10 minutes allows exposure of the posterior fossa face of temporal bone and internal auditory canal. Once the cerebellum has been slowly retracted, no external retraction is necessary. The cerebellum should fall away from the temporal bone, allowing viewing of the flocculus, choroid plexus, and the cranial nerve VII and VIII bundle (Fig. 171-11). The posterior lip of the internal auditory canal porus can be removed for additional lateral exposure, but the position of the posterior semicircular canal and its relationship to the posterior lip of the porus acusticus should be ascertained by CT.
Middle Cranial Fossa (Transtemporal) Approach: Internal Auditory Canal Porus to Tympanic Segment
The middle cranial fossa approach6 is used to expose the internal auditory canal and labyrinthine segments of the facial nerve when preservation of existing auditory function is desirable. The geniculate ganglion and tympanic portions of the nerve also can be decompressed using this approach.
Technique
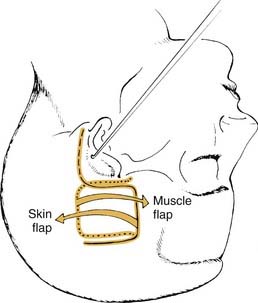
A 6 cm × 8 cm posteriorly based trapdoor incision is marked in the hairline above the ear (Fig. 171-12). If exposure of the mastoid is necessary, the inferior limb of the incision can be extended postauricularly. The skin flap is elevated to expose the temporalis muscle. A 4 cm × 4 cm temporalis fascia graft is harvested for use during closure of the internal auditory canal dural defect. An anteriorly based trapdoor incision is used to elevate the temporalis muscle and periosteum. Staggering the levels of the muscle and skin incisions provides for a double-layer watertight closure at the end of the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree