CHAPTER 178 Intraoperative Monitoring of Cranial Nerves in Neuro-otologic Surgery
The advent of sensitive diagnostic techniques and the refinement of microsurgical procedures have brought about a marked reduction in mortality rates for posterior fossa surgery; accordingly, increasing emphasis has been placed on preservation of cranial nerve function. This goal has in turn stimulated the development of techniques for monitoring cranial nerves during surgery. Seventh nerve monitoring during acoustic neuroma surgery has now become routine at most major medical centers, and anatomic preservation of the facial nerve has been achieved in more than 95% of the cases in some series.1 Although facial motility often is compromised in the immediate postoperative period, the long-term prognosis is good if the nerve can be electrically stimulated after tumor removal. Preservation of hearing has been more difficult to achieve because of the more intimate relationship of such tumors with the cochleovestibular nerve but is now often achieved in smaller tumors with the aid of eighth nerve monitoring. Furthermore, the techniques developed for facial nerve monitoring are now readily adapted for monitoring other cranial motor nerves. We have reviewed these topics in greater detail elsewhere.2
The emphasis in this chapter is on the practical aspects of instrumentation, electrode placement, different neurophysiologic techniques used, artifact identification, types of responses encountered, and the relationship between intraoperative recordings and clinical outcome. Somatosensory evoked potential (SEP) recording3 is not treated here, although SEP monitoring can be useful in monitoring large posterior fossa tumors with significant brainstem compression; discussions of SEP monitoring can be found in textbooks by Nuwer4 and Møller.5 This chapter is based primarily on the experience of the senior author with more than 700 posterior fossa procedures, as well as a review of the literature through 2007; also described are the methods currently available for cranial nerve monitoring, emphasizing facial and cochlear nerve monitoring during acoustic neuroma surgery but also including extension of these techniques to other nerves encountered in a variety of skull base procedures.
Neurophysiology in the Operating Room
Technical Considerations
Recording Electrodes: Type and Placement
Intramuscular hook wire electrodes, which are inserted with a hypodermic needle, also have been used.6 These are more delicate and have higher impedance, so the simpler needle electrodes are preferred, except in situations in which the electrodes cannot be easily fastened with tape, as in procedures involving the tongue, or when the use of insulated needles is desirable to avoid crosstalk from overlying muscles. An example of the latter case is recording from extraocular muscles, for which the electrodes must pass through the orbicularis oculi muscle and will therefore respond to facial nerve activity as well.
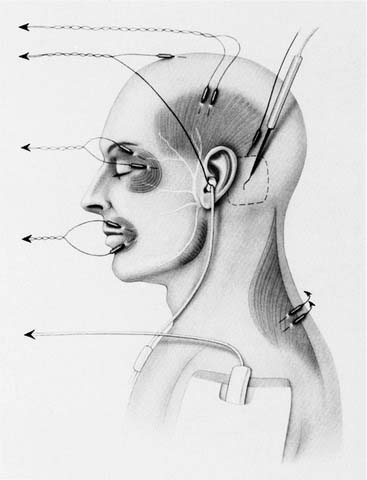
Figure 178-1 shows the positioning of recording electrodes for a middle fossa or retrosigmoid craniotomy for acoustic neuroma resection with a goal of hearing preservation. For a translabyrinthine approach, the same configuration is used, with the exception of the earphone and electrodes for ABR recording, because hearing conservation is not possible with this approach. Two channels are devoted to the facial nerve itself, with electrode pairs placed in orbicularis oculi and orbicularis oris muscles. One of the electrodes in the orbicularis oculi pair is placed at the lateral canthus, where it also will record volume-conducted activity in the lateral rectus muscle (from the sixth cranial nerve). One channel is used to record from the masseter or temporalis muscle (V3m) using hookwire electrodes, rather than subdermal needles, to reduce crosstalk, and the fourth channel is connected to electrodes in the ipsilateral trapezius muscle (eleventh nerve). The latter two channels serve two functions: First, larger tumors may expand to involve these nerves, so monitoring may help in their identification and preservation. Second, even with smaller tumors, the extra channels serve as a control for nonsurgical causes of increased EMG activity, particularly light anesthesia.
Stimulating Electrodes
Both monopolar and bipolar stimulating electrodes have been used for intraoperative electrical stimulation. In theory, a bipolar electrode can provide more precise localization, with less current spreading from the electrode to adjacent structures. In practice, however, the threshold for bipolar stimulation depends strongly on the orientation of the two contacts with respect to the axis of the nerve.7 Maintenance of a specific bipolar orientation is difficult in the close confines of the posterior fossa. Furthermore, if the stimulus intensity is near the threshold level (see later), a spatial resolution of less than a millimeter is easily obtained even with monopolar stimulation. Monopolar electrodes are therefore more commonly used; however, Schekutiev and Schmid8 and Dankle and Wiegand9 have described coaxial bipolar electrodes that may eliminate the problem of orientation.
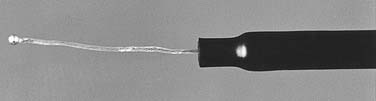
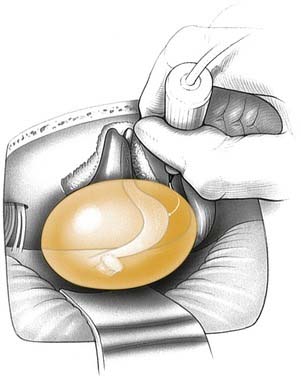
The monopolar electrode should be connected to the cathode of the stimulator; the anodal return usually is a needle inserted into the periphery of the wound, preferably on the posterior margin of the incision to minimize stimulus artifact. This is particularly important in recording from extraocular muscles, which yield small-amplitude and short-latency responses that can easily be swamped by electrical artifacts. Several types of monopolar electrodes are available. Prass and Lüders10 developed a malleable electrode, with the insulation continuous to a flush-tip that could be bent so that only the central portion of the tip contacted the desired tissue. They showed that this design minimized the spread of current to adjacent structures. Yingling and Gardi11 developed a probe with a flexible platinum-iridium tip, insulated except for a 0.5-mm ball on the end (Fig. 178-2). This electrode can be used to stimulate within dissection planes or even behind the tumor, out of the surgeon’s view, without concern for inadvertently damaging unseen neural or vascular structures (Fig. 178-3). With this probe, the facial nerve frequently can be located electrically even before it can be seen; dissection can then proceed in the most advantageous manner to avoid neural damage. Kartush and coworkers7 developed a set of Rhoton-type dissecting instruments that are insulated except at the cutting surface, allowing simultaneous dissection with constant stimulation. These “stimulus dissectors” are particularly useful for removing the last portions of tumor capsule that are closely adherent to a nerve.
Anesthesia
Cortical evoked potentials are notoriously sensitive to many anesthetic agents, so careful adjustment of anesthesia levels is necessary in applications such as spinal cord monitoring with SEPs. Fortunately, the ABR and EMG responses that are used for cranial nerve monitoring are essentially unaffected by any commonly used anesthetics. The major anesthetic consideration is a contraindication to the use of muscle relaxants, because blockade of the neuromuscular junction interferes with monitoring of EMG activity. A few reports12–14 have suggested that partial blockade can be used to prevent patient movement without blocking the ability to elicit EMG responses with facial nerve stimulation. However, in our experience, although electrically evoked EMG is relatively preserved, both spontaneous and mechanically elicited EMG activity tends to be suppressed by these agents. Therefore, no paralytic agents should be used during surgery with cranial nerve monitoring, other than short-acting agents such as succinylcholine given to facilitate intubation. Because the ABR and EMG are not significantly affected by routine concentrations of common anesthetics, no other constraints on anesthetic technique generally are necessary.
Finally, if local anesthetic is used at the incision site, care must be taken to avoid injection near the stylomastoid foramen to avoid anesthetizing the facial nerve. Alternatively, epinephrine 1 : 100,000 without any local anesthetic may be used to aid hemostasis.15
Facial Nerve (Seventh Nerve) Monitoring
Acoustic Neuroma and Other Cerebellopontine Angle Tumors
Facial nerve (seventh nerve) monitoring is routinely used in procedures to remove acoustic neuromas and other cerebellopontine angle tumors. Several techniques for facial nerve monitoring have been developed, including the use of sensitive detectors mounted on the face to detect facial nerve activity,16–19 intraoperative EMG, recording of compound nerve action potentials (CNAPs) from the facial nerve,20–22 intraoperative recording of nasal muscle F-wave,23,24 and video analysis to detect facial movements.25,26
Electromyography
Because of its higher sensitivity6,7,11,16,27–46 and easy application, EMG has by far overshadowed the other aforementioned methods and has become the most widely used modality for routine facial nerve monitoring. EMG recordings are used for monitoring cranial motor nerve activity in two distinct ways. First, intracranial electrical stimulation is used to identify and map the course of the nerves with evoked EMG activity and to determine the functional integrity of a nerve. Second, spontaneous EMG activity is continuously monitored to detect changes related to mechanical, thermal, or electrical irritation of the nerves by intraoperative maneuvers such as retraction,47 tumor dissection, use of electrocautery or lasers,48,49 or ultrasonic aspiration.
Activity Evoked by Electrical Stimulation
Assessment of Functional Status of Nerves after Tumor Removal
The primary use of intraoperative stimulation is in localizing and mapping the course of cranial nerves in relation to cerebellopontine angle tumors. However, electrical stimulation also is used to determine changes in the functional status of these nerves and is a useful predictor of postoperative function. In general, facial EMG responses elicited by low-threshold stimulation of the seventh nerve at the brainstem after total tumor resection constitute a good but not infallible predictor of postoperative function, because transient or delayed-onset facial palsies may be seen even when a low threshold is obtained at the end of the operation.50–53 Conversely, a substantially elevated threshold or the inability to elicit a response with stimulation up to 1 V carries a significant likelihood of postoperative facial dysfunction, particularly in the short run.51
Methods based on measurement of the compound muscle action potential (CMAP) amplitude after tumor removal also have been used to quantify the functional status of the seventh nerve.32,54 Absolute amplitude is quite variable between patients, however, and may be partially determined by nonspecific factors such as precise electrode placement, amount of subcutaneous fat,29 facial nerve dimensions, and muscle mass.55 These variations have led some investigators to use ratios rather than absolute values for assessment of postoperative facial nerve function. Taha and associates56 measured the ratio of CMAP amplitudes to stimulation at the brainstem proximally and at the internal auditory meatus distally after tumor excision and found that proximal-to-distal amplitude ratios greater than 2 : 3 were associated with excellent outcome. Similarly, Isaacson and colleagues57 analyzed proximal-to-distal amplitude ratios and reported that a higher ratio reflected good immediate postoperative facial nerve function. Lin and coworkers55 used the ratio between proximal amplitude measurement after tumor dissection and supramaximal amplitude measurement in response to transcutaneous facial nerve stimulation and found that a CMAP ratio greater than 50% of maximum had a 93% positive predictive value when measured at 0.3 mA.
Prediction of long-term rather than short-term facial nerve function is the surgeon’s major concern, because this would allow for better patient counseling and planning of rehabilitative treatment.58 It has been suggested that low threshold recorded at the brainstem after tumor resection is a good predictor of long-term facial nerve function50,59–61; however, the ability of threshold to accurately predict long-term function has been questioned by some.62,63 Neff and colleagues64 evaluated a combination of threshold and amplitude and found that a minimum threshold of 0.05 mA together with a CMAP amplitude greater than 240 µV predicts a good postoperative outcome 1 year postoperatively. Fenton and associates65 concluded that a more reliable predictor of long-term facial nerve is the clinical grade of early postoperative facial function. They also demonstrated that all patients with a recordable EMG response to proximal stimulation after tumor dissection, irrespective of the threshold or amplitude, recovered to a follow-up grade III or better facial nerve function. Although this correlation has been previously reported,53,54,61,66,67 its importance has gone unnoticed. Therefore, it is now accepted that whenever a recordable response to electrical stimulation of whatever amplitude or threshold can be demonstrated, the facial nerve is most likely to show signs of improvement with follow-up, and intervention is therefore not recommended within the first year.65 On the other hand, the absence of response to stimulation at the end of surgery does not doom the patient to a bad outcome. If the nerve is anatomically preserved, even with an immediate postoperative palsy, there is still a good possibility of eventual return of function as functional nerve fibers regenerate. Partial recovery of function in patients with unrecordable responses after surgery has been previously reported.68 The earlier the onset of recovery, the better its quality; however, ifevidence of recovery is lacking at 12 months, then it is unlikely to occur.69
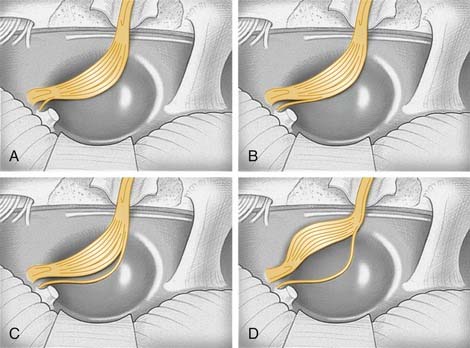
Intraoperative Identification of the Nervus Intermedius
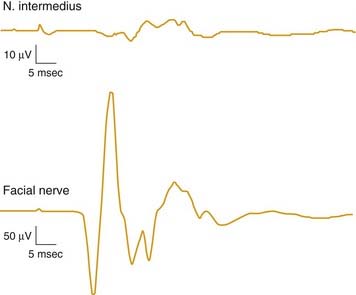
Anatomic identification of the nervus intermedius during cerebellopontine angle surgery is important in order to prevent confusing this nerve with the facial nerve itself. Electrical stimulation of the nervus intermedius during cerebellopontine angle surgery was found to produce a characteristic response in the orbicularis oris channel only: long latency, low amplitude, and higher in threshold than the facial nerve response70 (Fig. 178-4). Initial confusion between the nervus intermedius and a facial nerve strand at the time of stimulation is possible, because the entire course of the facial nerve may not be visually apparent to the surgeon as it passes anterior to the tumor—most common surgical approaches are from the posterior. Furthermore, tumor growth causes the facial nerve to be stretched and widened, so it often cannot be identified as a solitary trunk but rather is seen as a wide ribbon. The surgeon must recognize that stimulation of the nervus intermedius can cause EMG activity in the facial nerve monitoring channels (at least the orbicularis oris) but that the main trunk of the facial nerve may lie in an entirely different location within the cerebellopontine angle (Fig. 178-5). To protect this critical structure, it is imperative for the surgeon to locate the facial nerve itself by stimulation.
Spontaneous and Mechanically Evoked Activity
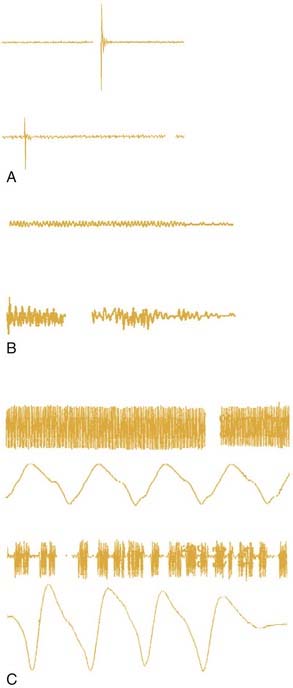
Patterns of Mechanically Evoked Electromyographic Activity
Prass and Lüders6 distinguished two types of EMG activity associated with intraoperative events: burst and train activity. These investigators suggested that the phasic “burst” pattern, characterized by short, relatively synchronous bursts of motor unit potentials, corresponded to a single discharge of multiple facial nerve axons, and was associated with direct mechanical nerve trauma, free irrigation, application of pledgets soaked with lactated Ringer’s solution over the facial nerve, or electrocautery. When burst activity occurs, it usually indicates that the facial nerve is being stimulated enough to result in depolarization and production of EMG response but not necessarily to the point of injury.71 It generally is accepted that the occurrence of burst activity of small amplitude (less than 500 µV in amplitude) is not of major concern, and accordingly, the surgeon need not be warned each time such activity occurs.72,73 On the other hand, the occurrence of large-amplitude burst activity (greater than 500 µV in amplitude) during the critical stages of dissection or final stages of drilling usually indicates a degree of facial nerve injury, the extent of which differs with the force and number of impacts.
As described by Prass and Lüders,6 the second pattern, tonic or “train” activity, consisted of episodes of prolonged asynchronous grouped motor unit discharges that lasted up to several minutes. These episodes were most commonly associated with facial nerve traction, usually in the lateral to medial direction. The investigators further divided such train activity into higher-frequency trains (50 to 100 Hz), dubbed “bomber potentials” because of their sonic characteristics, and lower-frequency discharges (1 to 50 Hz), which were more irregular and had a sound resembling popping popcorn. The onset and decline of “popcorn” activity were more gradual than the more abrupt onset and decline of “bomber” activity.
Subsequently, Romstock and coworkers72 classified train activity into three distinct patterns: A, B, and C trains. A trains are characterized by a sinusoidal symmetrical sequence of high-frequency and low-amplitude signals that have a sudden onset; B trains are regular or irregular sequences of repeated spikes or bursts with maximum intervals of 500 msec; and C trains are characterized by continuous irregular EMG responses that have many overlapping components. Although B and C trains did not correlate with postoperative function, the authors suggested a relation between the occurrence of A trains and poor postoperative facial nerve function.
Nakao and colleagues74 classified train activity that occurred during the last stage of tumor resection into an irritable pattern with frequent EMG responses to the slightest stimuli, a silent pattern with few or no EMG responses, a stray pattern with persistent train responses up to 20 minutes despite temporary discontinuance of surgical manipulation, and an ordinary pattern related to mechanical stimulation of the nerve but not easily elicited. These workers found an association between the occurrence of silent or stray EMG patterns and poor postoperative outcome. The occurrence of train activity does not always imply an impending nerve injury but indicates the proximity of the facial nerve to the region of dissection and thus should be considered a reassuring sign denoting an intact and responsive nerve.71 However, train activity of large amplitude (greater than 500 µV in amplitude) has been linked to postoperative nerve injury of variable degree,75,76 and such events require prompt warning to the surgeon. The absence of large-amplitude train activity, on the other hand, does not always mean safe dissection, especially with large tumors producing significant facial nerve compression. The nerve axons become stretched, partially damaged, and less responsive than healthy ones, generating little EMG activity despite significant manipulation.77 Therefore, spontaneous EMG activity may not be a reliable warning sign in large tumors, and the frequent use of electrical stimulation is important to map the tumor surface and measure any change of threshold from baseline to assess the condition of the nerve. Figure 178-6 shows representative samples of different types of EMG activity often encountered in vestibular schwannoma removal.
Limitations of Electromyographic Monitoring
Despite the wide use of intraoperative EMG monitoring, it still has its limitations. A major problem with EMG monitoring is its relatively low specificity. EMG channels can easily pick up artifacts, and the distinction between them and true EMG activity may sometimes be difficult. An example is artifacts produced by bimetallic potentials as a result of contact between surgical instruments made of different metals; because these may be associated with intraoperative events similar to those producing true EMG responses, they can be difficult to recognize. Some useful criteria include the fact that artifacts typically are higher in frequency content than EMG activity and thus sound more “crackly” than true EMG activity, which has more of a “popping” sound; and the tendency for artifacts to appear simultaneously on several channels, which is unlikely for EMG activity (Fig. 178-7). Experienced monitoring personnel are in an optimal position to make such decisions, rather than surgeons, who are focused on the operative field. Another limitation of EMG monitoring is that it is virtually useless during electrocautery, when the facial nerve is potentially at high risk. Attempts to reduce the artifact from bipolar cautery have met with limited success, because such devices generate high-amplitude, broadband noise that is difficult to filter out. Techniques based on detection of motion, which are not subject to electrical interference, such as video monitoring, may provide an important adjunct to EMG monitoring despite their relatively lower sensitivity. In our experience, the practical way to deal with this problem is to use electrical stimulation before bipolar electrocoagulation to confirm that the area to be cauterized is free from facial nerve fibers. The absence of a response to higher levels of electrical stimulation (up to 1 V) in an area about to be cauterized is an indication that electrocautery can proceed safely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree