CHAPTER 136 Interventional Neuroradiology of the Skull Base, Head, and Neck
Materials and Techniques
Angiographic Equipment
It is essential during endovascular interventional procedures to define the blood supply of a lesion with the highest possible resolution in all projections. Arteries or their collateral channels act as conduits for embolic material to the lesion. Of equal importance is the visualization of the many dangerous collateral vessels leading to the intracranial circulation or to the blood supply of the cranial nerves. Superb visualization and an excellent knowledge of the vascular anatomy are of paramount importance, as is an understanding of the potential clinical symptoms from embolization into an unwanted vascular territory and occlusion of the blood supply to normal tissues.1
Embolic Agents
Two commonly used particulate materials are Gelfoam (Upjohn Pharmaceuticals, Kalamazoo, MI) and polyvinyl alcohol (PVA) (PVA Foam, Cook, Inc., Bloomington, IN; Trufill, Cordis Endovascular Systems, Miami Lakes, FL; Ivalon, Inc., San Diego, CA; Contour Emboli, Boston Scientific/Target Therapeutics, Inc., Fremont, CA).2,3 Gelfoam breaks down 72 hours after embolization, and this lack of permanence detracts from its efficacy if surgery is not performed within a few days after the procedure. Gelfoam has been used as a preoperative embolization material for neoplasms that are to be operated on within 48 hours, and for patients with epistaxis in whom the goal is to slow the bleeding sufficiently so that the body’s normal hemostatic mechanisms stop the hemorrhage. Gelfoam powder always should be used with care because its particles (approximately 50 µm) in solution act as a liquid, easily passing through tiny arteries, which may result in skin necrosis or damage to cranial nerves, or through collateral channels communicating with the intracranial circulation.
PVA is more permanent than Gelfoam, but much of the efficacy of the vascular occlusion is a result of a combination of PVA plus intravascular thrombus. The stellate-shaped particles slow the intravascular flow, and thrombus forms.2–4 This thrombus may be metabolized before fibrosis occurs, however, resulting in partial or complete recanalization over weeks to months. PVA is easy to use, being supplied as uniform particles within a narrow range of size (150 to 1250 µm). In most patients with neoplasms, the smallest size (150 µm) is used because the particles can be easily injected through a small microcatheter placed selectively into tiny feeding arteries and penetrate into the tumoral vascular bed.
Because of the stellate shape of PVA particles, they do not form a tightly packed embolic mass, allowing recanalization as the interspersed thrombus undergoes lysis. Various types of beads and spheres have been produced to overcome that limitation, such as Embosphere Clear (Biosphere Medical, Inc., Rockland, MA). Their more uniform size and spherical geometry theoretically produce more complete and more permanent vascular occlusion. Similar spheres might also be filled with a chemotherapeutic or other agent for more prolonged treatment of a nonsurgical neoplasm. Microfibrillary collagen (Avitene; Avicon, Inc., Fort Worth, TX) is a hemostatic agent that may be mixed with contrast material for embolization5 or mixed with other embolic agents such as PVA and ethanol.6
Detachable balloons with a valve mechanism to keep the balloon inflated are currently unavailable in the United States, but should be available again in late 2009. They are used primarily for fistulas with a single artery-to-vein connection. Most experience was with intracranial post-traumatic carotid-cavernous sinus fistulas, but this technique was also used for vertebral artery–vertebral venous fistulas (usually post-traumatic) or for any other type of fistula in the face or neck.7–9 They were also used for occlusion of a parent artery leading to an unclippable aneurysm, a dissected carotid or vertebral artery producing embolization into intracranial vessels, or a carotid artery to be sacrificed at tumor surgery. Electrolytically detachable coils are used now instead of the currently unavailable detachable balloons. Many coils are usually necessary, however, to do what one balloon could accomplish, increasing the complexity and expense of the procedure.
There are numerous liquid embolic agents, the most commonly used being absolute alcohol (100% ethanol) and various tissue adhesives, including the cyanoacrylates and Onyx (MicroTherapeutics, Inc., Irvine, CA). Absolute ethanol is extremely toxic to the endothelium,10 and is highly effective at producing sclerosis of vascular lesions, such as venous and lymphatic malformations.11–13 Although it has also been used to treat arteriovenous malformations and dural arteriovenous fistulas, the problem with these fast-flowing lesions is the need to increase the “dwell time” of the ethanol to interact with the intima, often requiring temporary balloon occlusion more proximally. It has also been used for tumors, via endovascular and percutaneous access, particularly recurrent tumors that are surgically inaccessible.
Cyanoacrylates such as isobutyl-2-cyanoacrylate (IBCA) or N-butyl-2-cyanoacrylate (NBCA) produce polymerization of rapidly flowing blood within seconds. They not only produce immediate thrombosis and have tissue adhesive properties, but they also initiate a giant cell inflammatory reaction of the vessel wall.14 These embolic liquids are excellent for lesions with rapidly flowing blood, such as an arteriovenous malformation or an arteriovenous fistula. Neoplasms have slow flow, so there is no need to use these agents, which are associated with more risk than particulate materials injected intra-arterially or other agents injected percutaneously.
The newest “liquid” agent is Onyx, which is an ethylene vinyl alcohol copolymer containing dimethyl sulfoxide as the agent facilitating absorption through endothelial barriers.15 This tissue adhesive is a needed new addition to the armamentarium of the neurointerventionalist because it slowly permeates into tiny vessels feeding a vascular lesion, “creeping” into these feeders during fluoroscopic visualization and control, without the rapid setup time of the cyanoacrylates.15,16
Any embolization procedure with a liquid agent should be approached with trepidation because occlusion of the end-arteries to the face, tongue, and cranial nerves may lead to necrosis, and intracranial embolization may occur as the liquid passes through tiny collateral channels to vessels feeding normal structures. Liquid embolization should be performed only when superselective catheterization can be done directly into the direct feeders to the lesion, or with percutaneous puncture of the lesion and direct visualization of the flow of the agent,17 to prevent unwanted extension to the blood supply of vital structures.
Provocative Testing to Ensure the Safety of Embolization
Two important techniques help to ensure the safety of vascular occlusion at the skull base. The first involves the injection of lidocaine (Xylocaine) 1% without preservatives into an arterial feeder that is considered a candidate for embolization, to predict the potential of permanent cranial nerve palsy from the embolization procedure.18 This provocative test anesthetizes the cranial nerve if there is blood supply leading to it from the vessel catheterized. Critics of this test suggest that a false-positive test may occur because a liquid anesthetic can be injected into the capillary bed, whereas particles used for embolization stop short of terminal arterioles so that devascularization is rare. It is likely that a negative test result is truly negative and reassuring.
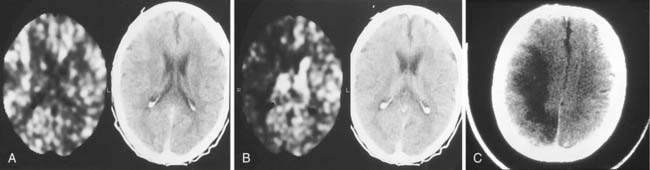
Different methods have been used during temporary occlusion to evaluate the physiologic effects of the BOT on cerebral blood flow to predict the risk of cerebral infarction after definitive occlusion. These methods include electric studies such as evoked potentials or electroencephalography,19 measurements of arterial stump pressures distal to the site of temporary occlusion,20 induced hypotensive challenges, and transcranial Doppler studies. Also, several cerebral blood flow imaging methods, including xenon-enhanced CT (Fig. 136-1),21 single photon emission computed tomography (SPECT), positron emission tomography, and MRI and CT perfusion studies, have been used to evaluate cerebral blood flow during BOT to determine the potential risk of ischemia after permanent occlusion.22,23 We prefer to use SPECT because it adds little to the basic BOT and easily provides the needed information. After the balloon has been inflated for a short time, the radionuclide is injected intravenously, and the patient is scanned a few hours after the completion of the angiographic study (the radiopharmaceutical “sticks” to the brain tissue during its initial circulation in proportion to the blood flow to that tissue).
Endovascular Treatment of Neoplasms
Paragangliomas
Paragangliomas, also known as chemodectomas or glomus tumors, are neoplasms related to chemoreceptor tissue. They usually are benign, but locally invasive and highly vascularized. Most glomus tumors originate within the temporal bone (48%), including lesions along the promontory of the middle ear (glomus tympanicum tumors) and lesions related to chemoreceptor tissue in the jugular bulb (glomus jugulare tumors). Tumors related to the vagus body (11%) in the high cervical region are called glomus vagale tumors, and tumors related to the carotid body (35%) at the common carotid artery bifurcation in the neck are called carotid body tumors. Multiple tumors are found in approximately 10% of patients (Fig. 136-2), and a familial form exists.24
Glomus Tympanicum Tumor
The glomus tympanicum is a tiny tumor that usually manifests with pulsatile tinnitus and otoscopically is seen as a reddish blue mass behind the tympanic membrane. CT scanning allows the differentiation of this small tumor from an extension into the middle ear cavity of a larger glomus jugulare tumor. It also is necessary to exclude an aberrant ICA. In the former, the bony plate between the jugular foramen and the middle ear is destroyed, whereas in the latter, the posterior bony margin of the carotid canal is missing.25 This tumor is usually small enough for surgery to be performed without embolization.
Glomus Jugulare Tumor
A patient with a glomus jugulare tumor usually presents with dysfunction of cranial nerves IX, X, or XI, and XII if the tumor is large. Pulsatile tinnitus also is common. Contrast-enhanced CT or MRI usually is the first diagnostic test performed, with the diagnosis generally made and the extension of the tumor shown. The tumor begins in the region of the jugular foramen and may extend inferiorly into the upper neck, superolaterally into the middle ear by destroying bone, posteromedially and posterolaterally into the posterior fossa, and anteriorly to envelop the petrous ICA. Bone destruction can be extensive, simulating a malignant tumor, as the chemodectoma spreads through the skull base. Destruction around the foramen magnum may occur, with compression of the brainstem.26
The tumor is fed by multiple external carotid artery (ECA) branches, with each of these arteries feeding a specific compartment of tumor. The ascending pharyngeal (bilaterally at times) and middle meningeal (posterior division) arteries are the most commonly involved, with the stylomastoid branch of the occipital and the posterior auricular arteries providing supply less frequently (Fig. 136-3). If the tumor extends posteriorly around the foramen magnum, supply may be from the anterior and posterior meningeal branches of the vertebral artery. Intradural tumor within the posterior fossa may be fed from the anterior and posterior inferior cerebellar arteries. Tumor surrounding the high cervical or petrous portions of an ICA may parasitize tiny branches of these segments (see Fig. 136-3).27–29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree