Chapter 113 High Myopia and the Vitreoretinal Complications
Introduction
The incidence of high myopia varies among ethnic groups, races, and countries, but there is a higher incidence in Asian countries. Some of the incidence rates worldwide range from 1% in Black Americans,1 2% in Caucasian Americans,1 2.6% in Chinese individuals,2 to 5.5% in Japanese individuals.3 The prevalence of myopia seems to be increasing,4 and it is one of the major causes of visual impairment, especially in Europe and Asia.5,6
Examiners often have difficulties obtaining clear and high-contrast OCT images in highly myopic eyes. The characteristics of the OCT image in these eyes are: (1) a relatively low signal to noise ratio; (2) deep posterior staphyloma in the presence of which the peripheral tissue often drops off from the top edge of the image; (3) poor fixation due to a large central scotoma from chorioretinal atrophy; and (4) critical signs that are mostly outside the fovea. The pearls for the OCT examination are as follows. First, it is much better to use spectral domain (SD-) OCT, which provides much higher sensitivity and scanning speed than time domain (TD-) OCT. TD-OCT is acceptable; however, micropathologies such as small macular holes or columns (glial thin tissue bridging the inner and outer retina in the area of retinoschisis) that are clearly depicted in SD-OCT images might be overlooked. Second, the pathology of interest must be located near the top of the OCT image. SD-OCT has the strongest signal at the top and the weakest at the bottom because of the so-called signal decay. This procedure maximizes the signal and enhances the contrast of the pathology being targeted. Third, large internal fixation or external fixation must be used to avoid unnecessary ocular movement in cases with a large central scotoma. Finally, attention must be paid to pathologies outside the fovea. For instance, a small macular hole is sometimes outside the fovea,7 and other micropathologies such as retinal vascular microfolds, internal limiting membrane detachments, and paravascular microholes are sometimes far outside the macula. The use of the 5-raster scan has a significantly higher rate of detection of these pathologies than the use of a single B-scan alone.8 The use of raster or grid scan is highly recommended to understand all of these micropathologies.
Imaging technologies have identified myopic foveoschisis, which is a relatively new pathology that was recognized about 10 years ago.9 It is now generally agreed that this pathology is not uncommon in highly myopic eyes, and myopic foveoschisis is regarded as a precondition for development of a macular hole and retinal detachment. OCT studies of myopic foveoschisis have revealed many preclinical and pathological conditions underlying the myopic–macular diseases, as discussed below. This information is also helpful for understanding the process and pathophysiology of macular holes and retinal detachments, which are the most problematic complications for vitreoretinal surgeons. In this chapter, we review the recent studies and shed light on the vitreoretinal complications of high myopia.
Retinal detachment from peripheral breaks
Retinal detachments from peripheral retinal breaks are common in high myopia. The prevalence of any type of retinal detachment increases in association with the degree of negative refractive error.10 The distribution of high myopia exceeding −6.0 D is about 16% in overall cases and the lifetime risk is more than 20-fold compared with emmetropia.11 In addition, the onset of retinal detachment is at a younger age, based on the degree of myopia.11 The frequency of retinal peripheral degeneration increases along with the axial length.12 The development of posterior vitreous detachment (PVD) according to the higher liquefaction of the vitreous body occurs at a younger age in eyes with severe high myopia.13 These facts seem to account for the increased prevalence of retinal detachment.
Epidemiology of surgical macular complications
The incidence rates of myopia-specific macular complications such as myopic foveoschisis and macular holes with or without retinal detachments have not been well documented, because these complications are rare. Myopic foveoschisis was identified in 9% of patients with posterior staphyloma.14 In patients with a macular hole and retinal detachment, 8.5% develop the same pathology in the fellow eye within 4 years.15
Rhegmatogenous retinal detachment after refractive surgeries
Rhegmatogenous retinal detachment is a major complication after refractive surgeries. The incidence is not as high after laser in situ keratomileusis and was reported to be 0.25%16; however, it is much higher after refractive lens exchange, reportedly 7.3% within 3 years17 and 8.1% in 7 years.18 Retinal detachment is a rare but general complication after cataract surgery, with incidence rates of 0.93% in the general population19 and 2.2% after phacoemulsification in highly myopic eyes.20 A high likelihood of PVD occurring within 5 years after surgery21 seems to be associated with a higher incidence.
Etiology and pathophysiology
Myopic foveoschisis
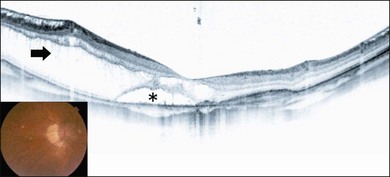
Myopic foveoschisis is characterized by retinoschisis with or without localized retinal detachment and is specific to high myopia. This pathology was identified recently (Fig. 113.1).9 Myopic foveoschisis is also referred to as a posterior retinal detachment without a macular hole in highly myopic eyes, described by Phillips in 1958, who reported a case with a retinal detachment within posterior staphyloma but no apparent macular hole.22 Perhaps some patients might have this pathology; however, it is difficult to rule out small macular holes or paravascular microholes. The detailed pathology and its mechanism awaited the development of OCT for decades. Takano and Kishi examined 32 highly myopic eyes with OCT and found retinoschisis in nine eyes and a foveal detachment in one eye, suggesting that retinoschisis and foveal detachment are not uncommon in highly myopic eyes.9 It has been reported that myopic foveoschisis is characterized by variations in the foveal architecture, including a foveal cyst in 47%, a lamellar hole in 29%, and a foveal detachment in 29%.23
The pathogenesis of myopic foveoschisis has been disclosed recently. Various OCT images from these myopic eyes have led to the hypothesis that the inner retina is less flexible than the outer retina.24 Factors limiting the inner retinal flexibility include the vitreous cortex adhering to the retina, epiretinal membranes (ERMs), internal limiting membrane (ILM), and retinal vessels. Preretinal membranes, which can be hard to recognize clinically and are found only at the microscopic level in highly myopic eyes,25 cause deterioration in the retinal flexibility.
Histologic studies have shown retinoschisis at multiple levels in the outer plexiform layer, inner plexiform layer, ganglion cell layer, and nerve fiber layer.26 There also is a preretinal fibrous membrane. The retinoschisis is bridged and a lamellar hole sometimes can be observed in the foveal region. An electron microscopic study on excised ILM samples during vitrectomy has shown that collagen fibers and cell debris were present on the inner surface of the ILM in 70% of the myopic foveoschisis, substantially more than that found in idiopathic nonmyopic macular holes (0%).25 Moreover, more fibrous glial cells were likely to be found on the inner surface of the ILM.26 Microvascular traction can be seen as arteriolar separation from the retina.27
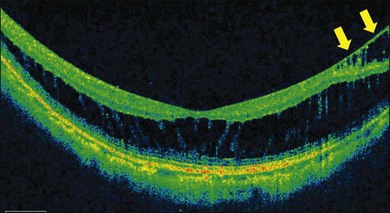
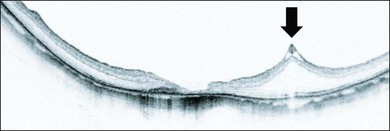
ILM detachments, sometimes recognized as “inner retinoschisis,” are often seen in highly myopic eyes, which explains the underlying traction from the ILM on the other retinal layers (Fig. 113.2).28 Inner retinal elevations along with retinal vessels recognized as tent-like lesions on OCT images, so-called retinal vascular microfolds, are observed especially in vertical sections (Fig. 113.3).29 This finding represents traction from the vessels on the retinal surface. A large OCT study of 200 highly myopic eyes reported a 6% incidence of ILM detachments, a 13.5% incidence of retinoschisis, and a 20% incidence of retinal vascular microfolds.30 These components generate inward tractional force on the inner retina, which potentially splits the retina, causing retinoschisis and finally leads to a retinal detachment at the fovea.
Macular hole with or without retinal detachment
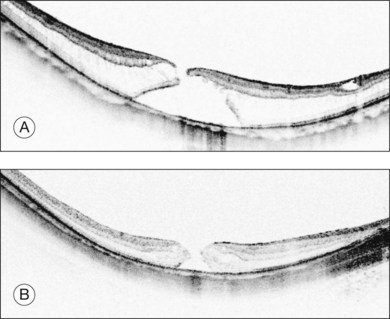
Retinal detachments from a macular hole are a typical complication in highly myopic eyes. The vitreous cortex adhering to the retinal surface around the hole causes tangential traction that generates an inward vector component in deep staphyloma in highly myopic eyes, resulting in a retinal detachment.31 Releasing the retinal traction is critical to successful reattachment; thus, vitrectomy with vitreous cortex and membrane removal is effective.31 Physicians sometimes observe macular holes without a retinal detachment,32 indicating that macular hole formation does not always lead to retinal detachment and that there might be two distinct types of macular holes in high myopia. A recent OCT study reported that persistent traction at the macular hole edge after opening is critical for initiating a retinal detachment.33 A macular hole with retinoschisis has a higher likelihood of progressing to a retinal detachment than those with a retinal cyst, resembling idiopathic non-myopic macular holes (Fig. 113.4).
A macular hole with retinoschisis typically presents with deeper posterior staphyloma, which explains the lower anatomic success rate in this subtype.33 Deep posterior staphyloma generates a larger vector component from the tangential traction exerted by the ERM or the ILM, which acts on the retina as an inward tractional force. This is why the retinoschisis is present in the retinoschisis type. In addition, with deep staphyloma it is more difficult to close the macular hole because of excess stretching in the retina. While shallower posterior staphyloma generates less tractional force and the retina is flat as seen in non-myopic eyes. This flat configuration exerts less stretching in the retina, and, thus, there is a higher likelihood of macular hole closure. The type of macular hole is highly dependent on the depth of the posterior staphyloma and underlying tractional force, which affect the anatomic success rate. OCT observation of the macular hole edge provides one clue to the prognosis.33
In highly myopic eyes, multiple components adhere to the retinal surface in most cases and are often recognized during vitreous surgery. Electron microscopic studies have shown that they are the vitreous cortex, cellular ERMs, and ILMs,34 suggesting that complete removal of these tractional forces is essential in reattachment surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree