CHAPTER 26 Hair Restoration
Medical and Surgical Techniques
As a result, hair restoration has long been considered an integral part of facial rejuvenation. Scalp hair loss—alopecia—can dramatically affect an individual. In fact, alopecia has been associated with significant changes in self-image, psychological well-being, and even success in a career.1 Hair loss draws attention to the forehead, the scalp, and the shape of the head and distracts the viewer from the central face and eyes. Hair loss can be a source of tremendous patient concern and anxiety. Subsequently, individuals invest considerable time and money in seeking treatment.
Neither gender escapes the difficulties associated with hair loss. In women, greater distress may be associated with even minimal hair loss, because alopecia in women is a less common and accepted problem.1 Although alopecia is the result of several different processes, the most common cause remains androgenetic alopecia (AGA). In men, AGA is characterized by the classic hereditary male-pattern baldness. In women, it manifests as a diffuse thinning with an intact anterior hairline, although occasionally a male-pattern type of hair loss can occur. AGA affects more than half of the male population and up to 40% of women older than 70 years.2,3
Pathophysiology
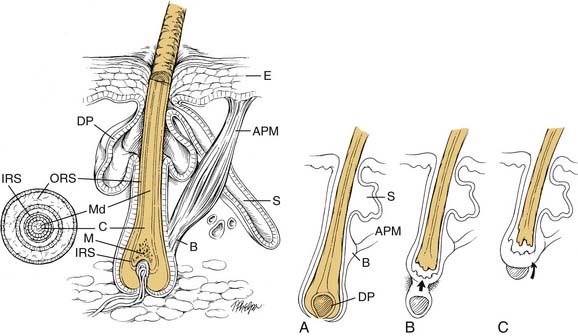
The average scalp has approximately 100,000 to 150,000 hairs.4 Hair density must decrease by 50% before alopecia becomes noticeable. Each hair contains both a matrix that is located below the dermis and a visible hair shaft (Fig. 26-1). The matrix lies beneath the dermis in the subcutaneous fat at the base of the hair follicle and contains rapidly dividing cells that migrate superiorly into the zone of keratinization. In this zone, cells undergo a process of dehydration and chemical change that results in the formation of the hair shaft, which is a dense mass of dead keratinized cells. As more cells are added to the base of the follicle, the shaft is displaced superiorly, and the hair shaft grows to become visible at the surface.
The formation of hair is a cyclical but asynchronous process that has periods of growth, involution, rest, and shedding.5 The majority of hair follicles in the scalp (approximately 90%) are in the growth, or anagen phase. This growth phase lasts approximately 3 to 10 years and is longer in women than in men. In the next stage, the catagen phase, proliferation ceases and involution occurs secondary to apoptosis. Less than 1% of the hair follicles are in the catagen phase, which lasts for less than 2 weeks. The remaining 5% to 13% of hair follicles are in the resting, or telogen phase. This stage last approximately 3 to 4 months during which there is no active hair growth.1 Alternatively, proteolytic enzymes may be induced during the telogen phase, which causes the hair shaft to be shed during a recently described exogen phase.5a Fifty to 100 hairs may enter the exogen phase each day from the normal telogen phase, and up to 400 may shed during a telogen effluvium (described later). The cycle begins again with the anagen phase and results in new hair growth from the area of shedding or displaces the previous hair shaft. Androgens play an essential role in regulating hair growth. At puberty, androgens increase the size of the follicles in the beard, chest, and extremities while decreasing the size of the follicles in the temporal region, thereby reshaping the anterior hairline.6
Androgenetic Alopecia
There are various causes of hair loss. AGA, or male-pattern baldness, is the most common cause in both genders (Table 26-1). AGA eventually affects 60% to 80% of white men and can begin in puberty. Approximately 20% of men note some hair loss at puberty, and the number increases sequentially with each decade. For example, by 30 years of age, 30% of white men have noted baldness, and, by 50 years of age, approximately 50% to 60% demonstrate alopecia.3 In women, the onset is typically later, with 40% of women 70 years old or older demonstrating alopecia.2
Table 26-1 Various Etiologies of Alopecia
| Diffuse Hair Loss | Focal Hair Loss |
|---|---|
The incidence of AGA varies among ethnic groups. In the black population, the incidence is approximately one-fourth that of white men.7 Japanese men have a similar incidence of AGA as black men during the earlier years, but the incidence increases to one-third that of whites as age advances.8 In Chinese men, AGA is rare before age 40 years.3 In all groups of patients, the incidence and severity of AGA increase with age.
The development of AGA depends on several factors. In a study of identical twins, Hamilton showed that the extent and development of AGA depended on the interaction of three factors: androgens, genetic predisposition, and age.3 The interaction of several genes (polygenic) and certain environmental factors influence the expression of hair loss.9,10 It is most important to note that androgens play a critical role in the development of hair loss. No expression of baldness due to AGA occurs in the absence of circulating androgens.
Hair follicles on the scalp are genetically predisposed to be either sensitive or resistant to androgenic factors that inhibit hair growth. Autograft studies have demonstrated this genetic predisposition. For example, hair follicles from the occipital scalp that are immune to androgens were transplanted to the bald frontal scalp and continued to grow. These findings established and continue to advance the concept of donor dominance and are the basis for successful hair graft transplantation.11
Various androgens variably affect different regions of hair growth. Testosterone influences axillary and pubic hair growth, whereas DHT affects beard growth and scalp hair, specifically the development of AGA.12 In addition, a hair’s sensitivity to androgens may change over time, accounting for the effect of age, puberty, and possibly environment.
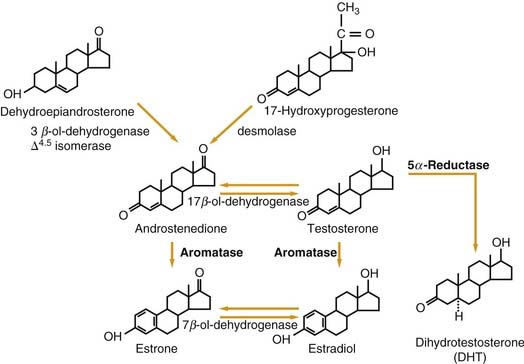
Extensive hair loss in men is not necessarily a reflection of an overall increase in testosterone. Two enzymes play critical roles in AGA (Fig. 26-2). The 5-alpha reductase enzyme is responsible for the metabolism of testosterone into DHT, which is the androgen that is most directly associated with the inhibition of hair growth and AGA. The cytochrome P-450 aromatase enzyme also has an important role in the hormonal pathway. Aromatase metabolizes testosterone into estradiol and androstenedione into estrone.13 A decrease in aromatase consequently increases the amount of testosterone that will be metabolized into DHT via the 5-alpha reductase pathway. Therefore AGA is mediated by increased 5-alpha reductase activity and by the lack of aromatase enzyme in specific regions of the scalp, thereby resulting in higher levels of DHT.
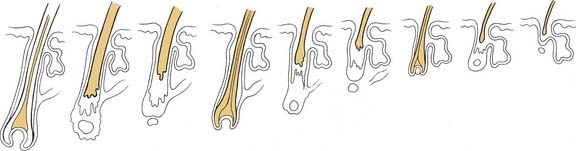
The end result of this androgen-mediated process in the development of AGA is the miniaturization of susceptible hair follicles. The follicles become progressively smaller in size and have shorter periods of growth so that coarse terminal hairs progress through a thinner, more lightly pigmented intermediate phase before they are replaced by fine vellus hairs (Fig. 26-3).14 In women, this process may advance beyond the stage of vellus hairs to produce a bald scalp that is completely free of hair.
Although androgenetic alopecia is the most common cause of hair loss, a variety of other etiologies should be considered in the patient’s evaluation (see Table 26-1). Alopecia manifests as either a focal or diffuse process and can be associated with or without scarring. Scarring can directly injure the hair follicle and lead to focal alopecia. Scarring alopecia is typically seen in patients with traumatic injuries such as lacerations, burns, radiation, and unfavorable sequelae of facelifting and endoscopic browlifting, as well as with selective connective tissue diseases, including discoid lupus erythematosus, lichen planopilaris, dermatomyositis, and sarcoidosis.15 If only the hair shaft is damaged, alopecia is temporary, because the underlying follicular apparatus continues to grow new hair. If the follicle, including the matrix, is completely destroyed, the loss of hair is likely permanent. Traumatic, nonscarring alopecia may also occur as a result of externally applied traction with certain hairstyles (e.g., cornrows, hair weaves).
Infectious etiologies should be considered in cases of focal alopecia. Staphylococcus aureus, Streptococcus, and syphilis are associated with folliculitis and furuncles, which can result in scarring and permanent alopecia. Tinea capitis is a fungal infection that results in focal, nonscarring alopecia and is diagnosed with a Wood light or a potassium hydroxide preparation of a hair sample.15
Diffuse, nonscarring alopecia is often associated with telogen effluvium in which diffuse hair shedding occurs as hairs precipitously shift from the growth phase to the resting and exogen phases. Telogen effluvium is a physiologic response to a variety of stressors including hormonal or systemic conditions and a broad range of medications. Hypothyroidism, hyperthyroidism, postpartum, and postmenopause are frequently seen as manifesting with diffuse alopecia.16 Categories of drugs that may result in temporary hair loss include chemotherapy agents, anticoagulants, anticonvulsants, thyroid replacement, beta-blockers, tricyclic antidepressants, and oral contraceptives.16 Patients with malnutrition, specifically with deficiencies in protein and essential minerals such as zinc and iron, may have poor hair growth and develop alopecia. Finally, patients undergoing severe physiologic (e.g., with acute and chronic systemic illness) or significant psychological stress (i.e., trichotillomania) can suffer from temporary hair loss.16
Focal or diffuse alopecia can also result from alopecia areata. Alopecia areata is an autoimmune disease that affects almost 2% of the population and typically manifests as small round patches of hair loss without evidence of scarring.6,17 The hair loss ranges in severity from small areas of alopecia that spontaneously regrow to persistent, extensive patches. The extent of loss can include the complete loss of all scalp hair (alopecia totalis) or all hair on the body (alopecia universalis).6 Inflammation may play a role by stimulating cytokines and growth factors, which retard hair growth.5
Patient Evaluation
For the majority of women with AGA, extensive hormonal evaluation is not necessary. Testing total testosterone, dehydroepiandrosterone, and prolactin levels is warranted if any of the following conditions associated with androgen excess are present: hirsutism, severe cystic acne, irregular menses, infertility, virilization, or galactorrhea. Measuring thyroid-stimulating hormone levels may be helpful if thyroid abnormalities are suspected. A complete blood count and iron studies should also be considered for a woman who has heavy or long-lasting menses.6
Examination of the scalp skin should include evaluating the pattern of hair loss as well as any skin lesions that are indicative of infection or malignancy. Hamilton3 published the first useful classification of AGA in 1951; Norwood and Shiell’s18 modification has become the standard system of classification used by hair restoration surgeons. This complete classification system includes seven categories (Fig. 26-4). The anterior hairline is altered with bitemporal recession occurring first, followed by balding of the vertex. As a more uniform frontal recession progresses posteriorly, the entire frontoparietal region eventually bears only inconspicuous vellus hair. The inferior occipital and temporal scalp are spared, resulting in the classic hair fringe.
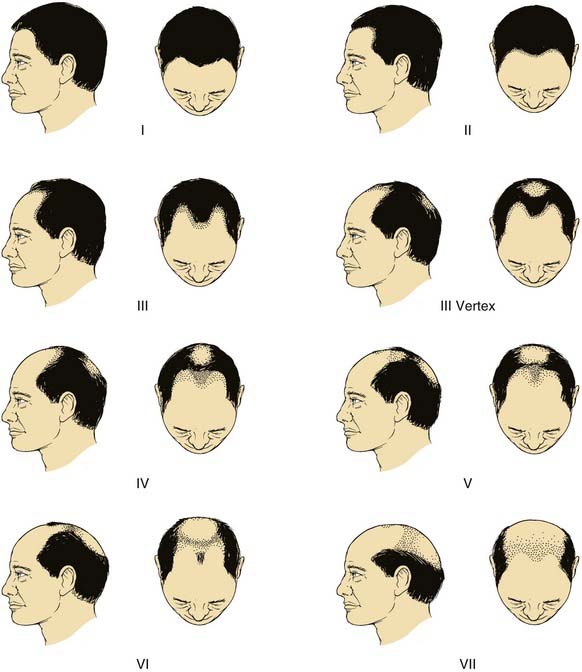
Figure 26-4. Norwood classification of the most common types of male-pattern baldness.
(Adapted from Norwood OT. Male pattern baldness: classification and incidence. South Med J. 1975;68:1359. Courtesy of Charles C Thomas, Publisher, Ltd., Springfield, Illinois.)
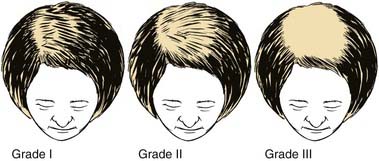
Female baldness patterns can be similar to those seen in men, but the genetic transmission is less clear. The Norwood classification system can be used, but female alopecia more often consists of a diffuse thinning in an oval area on top of the scalp. In 1977, Ludwig classified AGA in females into three stages (Fig. 26-5).19 In grade I, only perceptible thinning of the hair occurs at the vertex, while a thin band of more dense hair from 1 to 3 cm in width is retained at the hairline. More advanced stages correlate with an increase in hair loss on the vertex and a progressive thinning of the anterior hairline.
Patient Counseling
The initial consultation of a patient with hair loss must foster open communication and trust. Often these patients suffer from an altered body image and insecurity about their physical appearance. The patient must understand that the goal is not necessarily to restore his or her previous head of hair but rather to remove the appearance of baldness by recreating hairlines and improving hair density (Fig. 26-6).
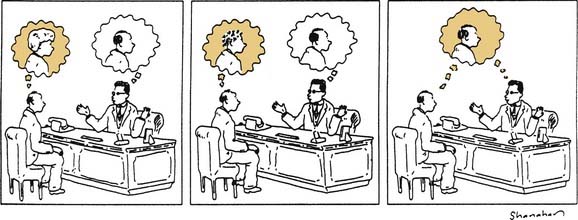
Figure 26-6. The initial consultation must foster the open discussion of realistic and obtainable goals.
(From Quinlan P. The consultation. In: Stough DB, Haber RS, eds. Hair Replacement: Surgical and Medical. St. Louis: Mosby; 1996:29, Fig. 1-17.
Medical Management
Minoxidil
Topical minoxidil is a piperidinopyrimidine derivative vasodilator that possesses trichogenic properties. Topical minoxidil is available in two strengths (2% and 5%) and is applied topically to the scalp twice daily. Minoxidil is safe for both men and women for the treatment of androgenetic hair loss. Originally used as an oral antihypertensive medication, minoxidil acts as a potassium-channel agonist, thereby resulting in a reduction in cytoplasmic-free calcium. The relevance of this unique cellular mechanism to hair growth is unclear. Various theories have postulated that hair growth is due to several mechanisms at the cellular level: (1) decreased activity of epidermal growth factor; (2) increased angiogenesis as a result of the up-regulated expression of vascular endothelial growth factor; and (3) increased activation of prostaglandin endoperoxide synthase-1.18,20,21
In several clinical trials, applying topical minoxidil (2%) twice daily resulted in dense hair regrowth on the vertex scalp in less than 5% of patients, while 25% to 30% of patients demonstrated moderate hair regrowth over one year.22–24 In patients for whom significant hair regrowth did not occur, minoxidil did appear to stop or significantly slow the progression of AGA.25 The results in women with AGA have been similar to those seen in men. Unfortunately, maintenance of the regrowth is dependent on continued use of minoxidil. When the treatment is discontinued, the hair gained is lost, and the hair that should have been shed during the treatment period will follow within 3 to 4 months. For those who continue its use, a peak effect is reached at approximately 1 year, with a subsequent slow decline in regrowth.26,27
Adverse reactions associated with topical minoxidil are primarily limited to irritant dermatitis or folliculitis (3% to 5%), which is now probably less with newer formulations such as the foam vehicle. Allergic contact dermatitis occurs in less than 1% of patients.23 Modifying treatment to include a lower concentration and less frequent application may alleviate these reactions. Increased hair growth (hypertrichosis) outside of the area of application (e.g., eyebrows, face, ears, arms, beard) has been reported, and is more common in women. The reason is unclear, but its occurrence is possibly the result of the inadvertent transfer of the topical solution.14,28 Patient compliance had also been an issue with the original topical minoxidil given twice-daily application, but some practitioners now suggest once-daily therapy.