Granulomatous Inflammation
Martha Farber
Chronic granulomatous inflammation is an inflammation characterized by epithelioid cells usually surrounded by lymphocytes and on occasion by plasma cells, polymorphonuclear leukocytes, and eosinophils. Epithelioid cells are modified macrophages that are involved in phagocytizing foreign material. Multinucleated giant cells are formed by fusion of macrophages and have different names (Langhan, foreign body giant cell, Touton giant cell), depending on the configuration of the nuclei within the giant cell.
The agents causing this type of inflammation are low-grade irritants, including traumatically introduced foreign material or endogenous material such as keratin, lipid, blood, cholesterol, and lens protein and infectious agents of low virulence such as viruses, fungi, protozoa, helminths, and bacteria that are obligate intracellular parasites. These agents either resist phagocytosis or are poorly broken down after phagocytosis, which can lead to extensive spread of the infection. Infectious agents within the granuloma can often be identified histopathologically with the use of special stains such as acid-fast stains, silver stains, and periodic acid–Schiff (PAS) stain. Granuloma formation develops under the influence of specific cytokines that differ from the cytokines of acute inflammation or the cytokines associated with wound repair. There are also some granulomatous systemic inflammations for which the cause is still unknown, such as sarcoidosis and rheumatoid arthritis.
Posttraumatic Granulomatous Inflammation
Injury to the globe with or without retention of foreign material may cause granulomatous inflammation.
Sympathetic Uveitis (Sympathetic Ophthalmia)
Sympathetic uveitis is a T-cell–mediated, bilateral, diffuse granulomatous uveitis that occurs after penetrating ocular trauma or surgery.1,2,3,4,5 The injury often involves uveal incarceration or prolapse. Although the inflammation may start as early as 5 days or as late as 50 years after injury, more than 90% of cases occur 3 weeks to 3 months after injury.6,7 A review of cases submitted to the Armed Forces of Pathology before 1950 revealed phacoanaphylactic endophthalmitis, another presumed autosensitivity disease, in 25% of patients with sympathetic uveitis. Only 5% of the sympathetic uveitis cases submitted after 1950 had associated phacoanaphylactic endophthalmitis. The marked reduction in cases manifesting both diseases probably is attributable to advances in the management of penetrating wounds.
Usually, removal of the injured eye before sympathetic uveitis occurs completely protects the noninjured eye against inflammation. Rarely, sympathetic uveitis has been reported to develop in the sympathizing (noninjured) eye after the injured eye has been enucleated.8 However, once the inflammation starts, removal of the exciting eye probably has little effect on the course of disease.9,10 Some evidence suggests that the prognosis for vision may be favorably affected by early enucleation of the exciting eye. Sympathetic uveitis in nontraumatized eyes has been reported in a few isolated cases. A diagnosis of sympathetic uveitis in the absence of an ocular injury, however, should be viewed with skepticism.11 Unless the whole eye is sectioned serially and examined carefully for evidence of perforation, the presence of some long- forgotten penetrating ocular wound cannot be ruled out.
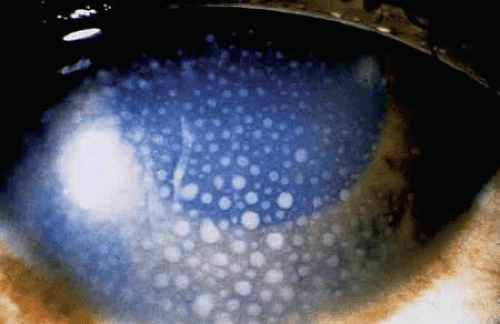
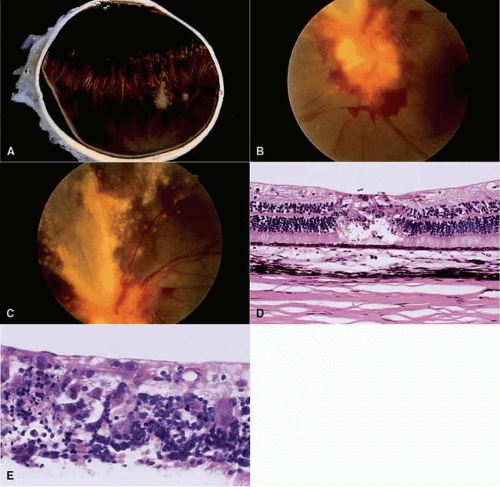
The acute onset of sympathetic uveitis generally is heralded by symptoms of blurred vision and photophobia in the sympathizing eye. Vision and photophobia worsen concurrently in the exciting eye, and a granulomatous uveitis develops. Biomicroscopy often reveals mutton-fat keratic precipitates in both eyes (Fig. 1). These precipitates consist of collections of epithelioid cells plus lymphocytes, macrophages, multinucleated giant cells, and pigment on the posterior surface of the cornea. Ocular hypertension may develop due to blockage of the angle by cellular debris or peripheral anterior synechiae. Occasionally, hypotonia occurs from decreased aqueous output by the inflamed ciliary body.
The cause appears to a delayed type of hypersensitivity reaction of the uvea to antigens localized on the retinal pigment epithelium (RPE), uveal melanocytes, and photoreceptors.12 The lymphocytic infiltrate consists almost exclusively of T lymphocytes, mainly suppressor-cytotoxic T cells.13,14,15 Sympathetic uveitis also shares many histologic features with Vogt-Koyanagi-Harada disease. The relation between the two diseases remains uncertain.16,17,18,19
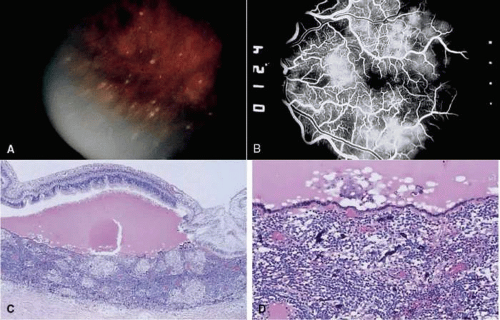
Sympathetic uveitis is a clinicopathologic diagnosis alone20 (Fig. 2). There are four characteristic histologic findings of both the sympathizing and the exciting eye:
Diffuse uveal thickening is caused by a granulomatous inflammation composed predominately of epithelioid cells and lymphocytes. Sometimes eosinophils are plentiful, but plasma cells typically are few or moderate in number, and neutrophils are rare or absent. The anterior segment is often distorted by the trauma, and in these cases, the posterior choroid is the best place to look for evidence of granulomatous inflammation.
The choriocapillaris and the posterior retina are spared from the inflammatory process.17,21 Granulomatous inflammation may involve the ora serrata.
Collections of epithelioid cells lying between Bruch’s membrane and the RPE are called Dalen-Fuchs nodules. These cells are derived primarily from circulating monocytes and macrophages.14 Some of the cells may be derived from RPE cells.24 Localized retinal detachments may be present, particularly overlying coalescing Dalen-Fuchs nodules.6
Granulomatous inflammation may extend into the uveal tissue that normally is present in the scleral canals and in the vicinity of the optic disc. Therefore, an evisceration that leaves behind the sclera and optic nerve may not protect a patient against sympathetic uveitis. Controversy remains over whether there is a greater risk of sympathetic ophthalmia after evisceration versus enucleation.25,26,27,28
Phacoanaphylactic (Phacoantigenic) Endophthalmitis
Phacoanaphylactic endophthalmitis is a unilateral (sometimes bilateral if the lens capsule is ruptured in each eye),17 zonal granulomatous inflammation centered around lens material. It depends on a ruptured lens capsule for its development.29,30,31 The disease is thought to be a result of a breakdown in tolerance to lens protein liberated through a rupture in the lens capsule.
Antibodies are formed against these lens proteins. The antibodies reach the lens remnants in the eye, and an antibody-antigen reaction called phacoanaphylactic endophthalmitis occurs. Lens protein is normally recognized by the immune system as self. The condition may be considered an autoimmune disease process that results from the breakdown or reversal of central tolerance to lens protein at the T-cell level.32 Small amounts of circulating lens protein normally maintain T-cell tolerance, but tolerance may be altered pathologically as a result of trauma, possibly through the adjuvant effects of wound contamination.16,33
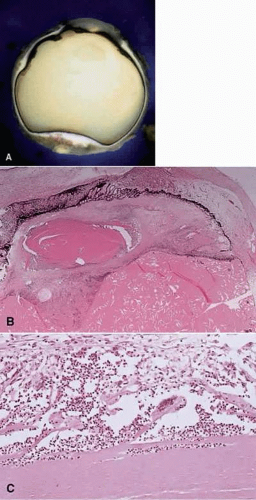
Histologically, in addition to the findings of trauma sufficient to rupture the lens capsule, a zonal granulomatous inflammation is found surrounding the injured lens. Neutrophils envelop and seem to dissolve the lens protein (Fig. 3). They are surrounded by epithelioid cells and occasional (sometimes abundant) multinucleated giant cells. Lymphocytes, plasma cells, fibroblasts, and blood vessels (granulation tissue) surround the epithelioid cells. Usually, if the lens is not dislocated posteriorly by the trauma, the iris also is encased in this inflammation and inseparable from it. The uveal tract generally shows a reactive, chronic nongranulomatous inflammatory reaction. On occasion, however, the same trauma that ruptures the lens capsule and produces the phacoanaphylactic endophthalmitis also sets off a sympathetic uveitis. As surgical techniques for repairing traumatized globes have improved, these two conditions do not accompany each other as frequently as they once did.
Unlike the lens protein that escapes through a ruptured lens capsule, the lens material that leaks through an intact lens capsule in mature or hypermature cataracts presumably is denatured. This denatured protein incites a macrophagic response but apparently is incapable of acting as an antigen and eliciting an antibody response. The macrophages, swollen with their engulfed denatured lens material, may block the anterior drainage angle and cause an acute secondary open-angle glaucoma called phacolytic glaucoma.34
Foreign Body Granulomas
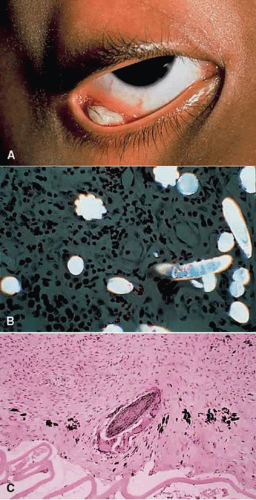
Foreign body granulomas may develop around exogenous foreign bodies that generally are introduced into the eye at the time of a penetrating wound35,36,37 (Fig. 4). They also may develop around endogenous products such as blood, cholesterol, keratin, or lipid. Blood in the vitreous, on rare occasions, incites a foreign body inflammatory response.38 When this occurs, the intravitreal hemorrhage almost invariably is traumatic in origin rather than spontaneous. Intraocular migration of caterpillar or tarantula hairs can also lead to choroidal granulomas. Histologically, a zonal type of granulomatous inflammatory reaction surrounds the foreign body.36,39,40
Nontraumatic Infectious Granulomatous Inflammation
Many different organisms (fungi, bacteria, viruses, parasites) can produce a granulomatous inflammation within the eye and ocular adnexa. These infectious agents are sometimes difficult to distinguish clinically, and in immunodeficient patients, concurrent infections with more than one organism may occur.41 Histologic examination with the use of special stains is helpful in determining the causative agents. Immunoperoxidase studies, in situ hybridization, and the polymerase chain reaction (PCR) are sometimes needed to identify the organisms.42,43,44
Viral
Cytomegalic Inclusion Disease (Salivary Gland Virus)
Cytomegalic inclusion disease is caused by the cytomegalovirus (CMV), a herpes virus with a double-stranded DNA core. Congenital and acquired forms of the disease exist. Cytomegalic inclusion disease is the most common viral infection of the neonate, with an incidence of 5 to 20 per 100 live births. The congenital infection is characterized by low birth weight, jaundice, retinochoroiditis, hepatosplenomegaly, and neurologic involvement. Clinically, the central retinochoroiditis is similar to congenital toxoplasmosis except for the lack of hemorrhage in toxoplasmosis. Laboratory testing reveals thrombocytopenia, anemia, and intracranial calcifications. Most infected infants are asymptomatic at birth.
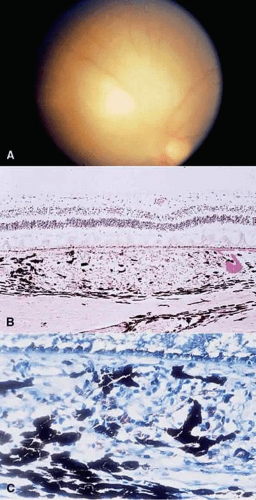
The adult form is found mainly in patients who are immunosuppressed due to chemotherapy, cancer,45 or organ transplants46 or who are immunodeficient due to HIV infection.47,48,49,50,51 CMV retinitis is the most common ocular infection in patients with AIDS. The adult acquired CMV form starts with scattered, white retinal dots or granular patches that may become confluent.46,47 These may begin in the peripheral or central retina and are associated with sheathing of retinal vessels and retinal hemorrhages.52,53
Histologically, a primary, coagulative, necrotizing retinitis and a secondary, diffuse, granulomatous choroiditis are seen. This choroidal infiltrate is minimal in AIDS patients with CMV retinitis. The infected retinal cells show large eosinophilic intranuclear inclusions and small, multiple, basophilic intracytoplasmic inclusions, both of which are highly characteristic of CMV.54,55 The intracytoplasmic inclusions consist of numerous virions closely associated with dense masses of matter (PAS positive on light microscopy). The intranuclear inclusions are formed by the presence of virions within a mass of viral subunit material that forms a lacy, centrally located pattern in the nucleus.55 The nucleolus is marginated and free of virions. Clumping of peripheral chromatin is lacking (Fig. 5).
Herpes Zoster Ophthalmicus
Ocular complications occur in more than 50% of cases of herpes zoster ophthalmicus.56 Corneal complications include dendritic ulcer (rare), ulceration, perforation, peripheral erosions, bullous keratopathy, pannus formation, stromal vascularization, hypertrophy of the corneal nerves, ring abscess, granulomatous reaction to Descemet’s membrane, and endothelial degeneration. Peripheral anterior synechiae, exudate, and hyphema may be present in the anterior chamber. A chronic nongranulomatous anterior uveitis usually develops. A fibrovascular membrane of the anterior surface of the iris, posterior synechiae, and cataract formation can complicate the inflammation. A mild mononuclear infiltrate may be found in the vitreous. A perivasculitis and vasculitis may be present in the retina, optic nerve, and long posterior ciliary vessels. The varicella virus has also been detected in progressive outer retinal necrosis, an extremely rapid retinal infection found in AIDS patients.57 Chronic nongranulomatous inflammation is also seen in the choroid, long posterior nerves, and optic nerve meninges.58 Less commonly, a granulomatous inflammation may involve the choroid. Acute and chronic inflammation of the sclera and episclera also is a complication in herpes zoster ophthalmicus.
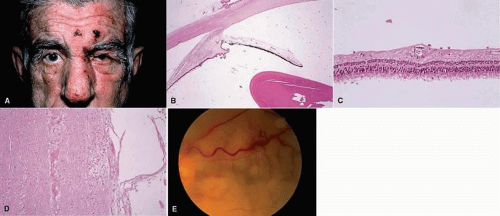
Histologically, the most characteristic findings are the lymphocytic (chronic nongranulomatous) infiltration involving the posterior ciliary nerves and vessels, frequently in a segmental distribution. This may result in a diffuse or patchy necrosis and atrophy of the iris and pars plicata (Fig. 6). Granulomatous inflammatory lesions surrounding areas of necrosis also may be seen, most commonly in the choroid or surrounding Descemet’s membrane.59 Inclusion bodies have not been demonstrated in the chronic inflammatory lesions.60,61
Bacterial
Mycobacteria
Tuberculosis (Mycobacterium tuberculosis)
The hematogenous spread of the tubercle bacilli from the lungs is the major route for intraocular infection. HIV-infected patients are at high risk for infection. The most common form of ocular involvement with tuberculosis is a uveitis (choroidal tubercles are most common) that may spread to involve the retina.62,63,64 The involvement may become massive to form a large tuberculoma involving all coats of the eye (panophthalmitis).65,66 Clinically, mutton-fat keratic precipitates are seen on the posterior surface of the cornea. PCR on vitreous specimens to detect mycobacterial-specific DNA sequence is helpful in making the diagnosis. Histologically, the classic pattern of caseation necrosis consists of a zonal type of granulomatous reaction around the areas of coagulative necrosis. Acid-fast bacilli can be demonstrated by special stains.67,68
Leprosy (Mycobacterium leprae)
There are two forms of leprosy: lepromatous leprosy and tuberculoid leprosy.
In lepromatous leprosy, the lepromin test (analogous to the tuberculin test) is negative, suggesting little or no immunity. The prognosis is poor. Lepromas of the skin result in leonine facies and neurologic changes. Most often, the anterior portion of the eye is involved with inflammation.69,70,71 Impaired corneal sensation is the major complication of the disease. Histologically, a diffuse type of granulomatous inflammation containing lepra cells, histiocytes with amorphous cytoplasm, and Virchow cells, histiocytes with vacuolated cytoplasm, is present, mostly in the anterior portion of the eye. This is thought to be due to the fact that the bacteria grow better in the cooler anterior portion than the warmer posterior portion of the eye, similar to the skin being more involved than deeper structures of the body.
In tuberculoid leprosy, the leproma test is positive, suggesting immunity. The prognosis is good. A neural involvement predominates, with hypopigmented (vitiliginous), hypoesthetic lesions and thickened nerves. The ulnar nerve is particularly vulnerable, leading to the characteristic claw hand. The ocular adnexa and orbital structures are involved, especially the ciliary nerves, but not the eyeballs. Histologically, a discrete (sarcoid, tuberculoid) type of granulomatous inflammatory reaction is seen, centered mainly around nerves. The individual nodules tend to be of much more varied sizes than those in sarcoidosis or miliary tuberculosis. Because there is good immunity, organisms are much harder to find and are generally located in an area of nerve degeneration.
Nontuberculous Mycobacteria (Mycobacterium chelonae, Mycobacterium fortuitum, Mycobacterium avium-intracellulare)
These opportunistic organisms can cause periocular infection,72 keratitis,73 granulomatous uveitis (which may be asymptomatic if in the choroids), or a panophthalmitis. The infection is seen most often in immunocompromised patients. Histologically, discrete granulomatous inflammation within the uvea or inflammatory, necrotic masses may be present. Acid-fast bacilli are detected within the cytoplasm of macrophages as well as free within the necrotic tissue74 (Fig. 7).
Spirochetes
Lyme Disease
There are three overlapping chronologic stages of Lyme disease, caused by the spirochete Borrelia burgdorferi.75 The bacteria are transmitted by the Ixodes dammini tick. Within 4 to 20 days of a tick bite, the first stage is heralded by a red rash, erythema migrans, at the site of the bite. Flulike symptoms, including fever, swollen lymph nodes, and malaise, are often present at this stage. Ocular findings at this stage may include a follicular conjunctivitis. The second stage of the disease occurs weeks to months later and has systemic findings, including skin lesions, cardiac and central nervous system symptoms, and arthritis. At this stage, ocular signs may include blepharoconjunctivitis, bilateral granulomatous uveitis, neuroretinitis, retinal vasculitis, cranial nerve palsies, and pupil abnormalities.76 Stage three can occur months to years after a diseasefree period and is characterized by Lyme arthritis, which occurs in more than 50% of untreated patients. Central nervous system disease and keratitis, scleritis, and extraocular muscle inflammation may occur.77 Enzyme-linked immunosorbent assays, Western blot analysis, or PCR can detect antibody against the Borrelia antigens.78
Syphilis (Treponema pallidum)
Both the congenital and acquired forms of syphilis may produce a nongranulomatous interstitial keratitis or anterior uveitis.79,80 The common form of posterior uveitis is a smoldering, indolent, chronic, nongranulomatous inflammation. It is characterized by disseminated, large, atrophic scars surrounded by hyperplastic RPE. A more virulent type of uveitis may occur with a granulomatous inflammation.81 Both the nongranulomatous and the granulomatous forms of uveitis often involve the overlying retina82 and can also involve the anterior uvea.83 When anterior chamber involvement occurs, spirochetes may be obtained by aspiration of aqueous from the anterior chamber. The uveitis often occurs during the secondary and tertiary phases of the infection, when skin lesions and central nervous system findings are present (Fig. 8). Histologic findings in the nongranulomatous disseminated form of posterior choroiditis include atrophy and scarring of outer retinal layers, RPE, and inner choroidal layers. Scattered lymphocytes and plasma cells may be present. Dehiscences in Bruch’s membrane may occur, through which retinal elements may invade the choroid. Bruch’s membrane may be folded into the atrophic, sclerosed choroid. The treponema spirochetes can be demonstrated in the ocular tissue with special stains, often in areas devoid of inflammatory cells. In the granulomatous form of posterior chorioretinitis, the inflammatory process generally involves the choroid and overlying retina and is quite vascular. Epithelioid cells, lymphocytes, and plasma cells are seen. Treponemas can be demonstrated in the inflammatory tissue with the Warthin-Starry stain.84
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree