Gram-Positive Aerobic Rods
Regina Sun
Vicente Vitiello
Andrew J.W. Huang
Aerobic gram-positive rods are infrequent ocular isolates. Bacillus, Corynebacterium, and Nocardia are the most common genera associated with ocular infections (Table 1).
TABLE 1 Gram-Positive Bacteria of Ocular Importance | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Bacillus Species
The genus Bacillus is an extensive family of large, gram-positive, spore-forming, aerobic, and facultatively anaerobic rods comprising over 100 species, such as the better known B. anthracis, B. cereus, and B subtilis. These bacteria are found commonly in air, soil, dust, hay, milk, water, and wood. Bacillus species are important sources of antibiotics (e.g., bacitracin and polymyxins). With the exception of B. anthracis as an obligate pathogen of animals and humans, they are opportunistic pathogens, causing disease in the presence of a foreign body (e.g., prosthesis, catheter, or shunt), after surgery or trauma, or in intravenous drug abusers. B. cereus can either cause infection or be isolated as a contaminant.
Identification and Virulence Factors
B. anthracis is a large organism that is arranged as single or paired bacilli in clinical specimens and as long serpentine chains and clumps in cultures. In addition to its capsular antigen, B. anthracis has a polysaccharide cell-wall somatic antigen and a toxin associated with it. This toxin consists of three distinct antigenic and heat-labile components: protective antigen, lethal factor, and edema factor. Although none of the components are active alone, the combination of protective antigen with either of the other components has toxic properties. The two major factors responsible for B. anthracis virulence are the presence of the capsule and toxin production.1,2
Following the outbreaks of anthrax in livestock during the World War I, B. anthracis has been under intensive research and development for military purposes. Even though the natural infection is usually controllable, the outbreaks of anthrax-related bioterrorism in the United States in 2001 heighten public anxieties about this organism. It remains one of the top microbial agents, which potentially could be deployed for biological warfare or bioterrorism.
B. anthracis can be readily detected by the microscopic examination and culture of corneal ulcers. Large gram-positive bacilli are seen in tissue. It will grow on nonselective laboratory media with the appearance of nonhemolytic, readily growing, adherent colonies. Definitive identification requires the use of selected chemical tests and demonstration that B. anthracis is nonmotile. B. cereus also grows rapidly and is readily detected in specimens collected from infected eyes. It can resemble B. anthracis but generally is motile and produces markedly hemolytic colonies.
Ocular Infection
Bacillus organisms are a rare but serious cause of endophthalmitis and suppurative keratitis.3,4 Several species have been recovered from eye infections. In addition to trauma, failure of contact lens disinfection is an important predisposing factor to corneal infection by these organisms.5,6,7 In one study, 3% of contact lens-associated corneal ulcers were caused by Bacillus organisms.8 Bacillus organisms have been found in the contact lens care systems of 3% to 7% of asymptomatic patients.9,10 These organisms form spores that are resistant to heat sterilization and many types of chemical disinfectants used for contact lens care. Once a care system is contaminated, it may be difficult to eradicate the organism.11 Trauma, injury with vegetable matter, and exposure to biologic insecticide12 are other risk factors for keratitis. Bacillus has been reported as the causative agent in about 2% of all bacterial keratitis.8,13
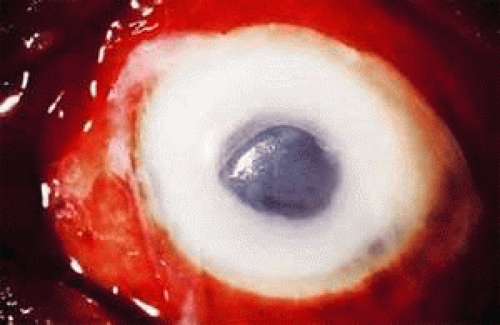
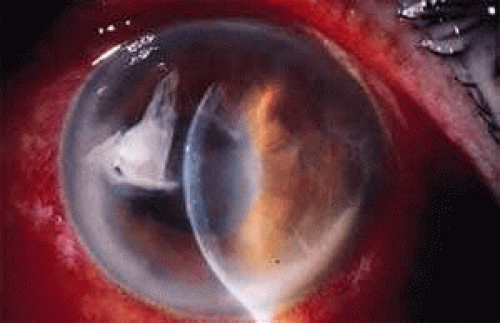
The clinical onset of B. anthracis keratitis can begin with multifocal epithelial opacities that lead to a focal stromal infiltrate. B. cereus keratitis can be extremely severe and can rapidly progress to perforation. It may be characterized by a ring infiltrate in the stroma that is remote from the site of the injury (Fig. 1).14 A history of a corneal foreign body or other corneal trauma preceding the infection generally can be obtained (Fig. 2). B. cereus is one of the most destructive organisms affecting the inner eye that often follows penetrating injuries. The source of the organisms can be either soil contamination of the object penetrating the eye or direct inoculation of organisms colonizing the eye surface. B. cereus panophthalmitis almost always ends in complete loss of vision within 48 hours of the injury with massive vitreoretinal destruction.15 The pathogenesis of B. cereus panophthalmitis is incompletely defined. At least three toxins have been implicated: necrotic toxin (a heat-labile enterotoxin), cereolysin (a potent hemolysin named after the species), and phospholipase C (a potent lecithinase). It is likely that the rapid destruction of the eye, the most devastating characteristic of intraocular B. cereus infection, is the result of interactions of these toxins and unidentified factors.
Susceptibility
Most strains of B. anthracis are susceptible to penicillin but may have variable susceptibility to cephalosporins. In vitro results may not always correlate with clincal efficacy. In general, B. anthracis is sensitive to penicillin, tetracycline, and chloramphenicol, whereas B. cereus is sensitive to clindamycin, vancomycin, erythromycin, chloramphenicol, fluoroquinolones, and aminoglycosides.
According to the 2004 guideline of Centers for Disease Control and Prevention (CDC), postexposure prophylaxis is needed to prevent inhalation anthrax. The recommended regimen is 60 days of antibiotic therapy with ciprofloxacin, doxycycline, or levofloxacin and 3 doses of anthrax vaccine.16 Oral ciprofloxacin has been successfully used for treating wound infection, bacteremia and pulmonary infection of B. cereus. For ophthalmic infections caused by B. cereus, early treatment with topical or intraocular clindamycin and gentamicin appears to be most effective.
Corynebacterium Species
Corynebacteria are a heterogenous group of organisms sometimes called “coryneforms” (“coryne” meaning “club” in ancient Greek) or “diphtheroids” (named after the most pathogenic member, C. diphtheriae). In contrast to other regularly shaped aerobic, gram-positive rods such as Bacillus and Listeria, the coryneform bacteria are small, usually pleomorphic, irregularly shaped gram-positive rods that appear in short chains (U or Y configurations) or in clumps resembling Chinese letters.
The genus Corynebacterium is restricted to bacteria with cell walls containing meso-diaminopimelic acid (m-DAP), arabino-galactose polymers, and short-chain mycolic acids. They are aerobic, non-spore-forming, non-acid-fast, nonmotile, and catalase-positive and can ferment carbohydrates to produce lactic acid. A spectrum of corynebacterial isolates from clinical specimens has been examined systemically.17
Identification and Virulence Factors
The clinical significance of clinical isolates of coryneform bacteria is often confusing. This is in part due to the natural habitat of corynebacatreia, as many of them are part of the normal flora of skin and mucous membranes in humans. C. diphtheriae, the major pathogen in this group, produces a necrotizing toxin that enables it to penetrate an intact corneal epithelium. This protein is a 63-kd protein that consists of two fragments. One of them binds the cell surface, and the other enters the cell and catalyzes the irreversible inactivation of elongation factor-2 (EF-2), which is required for movement of nascent peptidic chains on ribosomes. It has been estimated that one exotoxin molecule can inactivate the entire content of EF-2 in a cell. The concentration of iron also is critical. Iron is an essential element for bacteria growth; however, high concentrations of iron suppress toxin production. EF-2 toxin also has been found in strains of C. ulcerans and C. pseudotuberculosis, both being the closest relative of C. diphtheriae phylogenetically. A PCR (polymerase chain reaction)-based detection system for diphtheria toxin has been described and validated by the CDC.18 However, using such a test as the primary test for clinical specimens has not been recommended, and microbiological culture is essential for confirming diphtheria.
Basic microbiology laboratory tests are valuable for identifying corynebacteria. Corynebacterial species often stain irregularly because of the presence of metachromatic granules. Most of the species are slow growing. Colonies may not become visible on culture plates for up to 1 week or more.19,20,21,22 Although most species of corynebacteria grow well on ordinary media such as sheep blood agar, some species (C. ovis and C. ulcerans) require Loeffler’s or tellurite media for optimal growth.
Differentiation among corynebacterial species usually is difficult. Characteristics such as colony size, pigmentation, odor, and presence of hemolysis are helpful for identification. Key reactions include catalase production, fermentative or oxidative metabolism, motility, nitrate reduction, urea production, esculin hydrolysis, acid production, and the cyclic AMP reaction.23
Ocular Infection
Corynebacterial species are commonly encountered as part of the normal flora of the skin and mucous membranes in humans. They were formerly regarded as nonpathogenic contaminants of the human external eye, but there have been many eye infections reported to be caused by corynebacteria.24 Some species have been reported only as ocular pathogens (e.g., coryneform group A-4 and A-5 bacteria).25
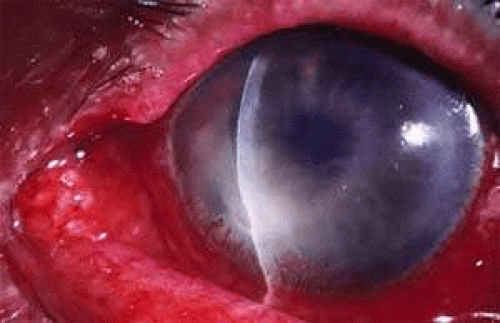
Membranous or pseudomembranous conjunctivitis caused by C. diphtheriae is a classically described entity usually seen in children between 2 and 8 years of age.26 C. macginleyi is primarily isolated from conjunctivitis.27 Late-onset postoperative endophthalmitis caused by C. macginleyi has also been described.15,28 Corneal ulcers caused by corynebacteria usually have an indolent onset and a clinical course with an epithelial defect, an underlying stromal infiltrate, minimal or absent purulent discharge, and a variable amount of anterior chamber reaction and pain (Fig. 3). Old age, ocular surface disease, exposed corneal sutures, eyelid abnormalities, extended-wear contact lenses, diabetes mellitus, and viral keratitis29 are frequent risk factors. C. xerosis is often isolated from Bitot’s spots, a focal conjunctival keratinization seen in xerophthalmia associated with systemic vitamin A deficiency.
Susceptibility
Antibiotic sensitivities among corynebacteria vary greatly. Antimicorbial susceptibility should always be evaluated for clinically significant isolates. Erythromycin, vancomycin, penicillins, tetracycline, and aminoglycosides often are effective. Due to the emergence of vancomycin-resistant gram-positive bacteria, it is inappropriate to use vancomycin as the first-line drug for corynebacterial keratitis.
Listeria Species
The genus Listeria consists of six species. Human disease is mainly caused by L. monocytogenes and rarely by other animal pathogens such as L. ivanovii. L. monocytogenes is a gram-positive, motile, non-spore-forming, non-acid-fast, facultatively anaerobic organism. Its name is derived from its ability to elicit a monocytic reaction in infected animal hosts.30
L. monocytogenes was first reported in 1926.31 and most early reports recognized its role as an animal pathogen. Ocular infection in humans was first noted in 1934, when purulent conjunctivitis developed in a laboratory assistant after accidental inoculation of the organism.32
Listeria species are widely distributed in the environment and asymptomatic human and animal carriers; however, human infection by L. monocytogenes is uncommon and restricted to several well-defined populations: neonates, the elderly, pregnant women, and immunocompromised patients, particularly those with defective cell-mediated immunity. Any organ can be infected by the pathogen, but there is a marked tropism for the central nervous system. Meningitis is the most common disease associated with L. monocytogenes.33,34 Bacteremia, endocarditis, pneumonia, serositis, osteomyelitis, gastroenteritis,35 septic arthritis, and dermatitis have also been described. Although epidemic food-borne transmission in industrialized countries and vertical transmission from mother to offspring are established routes of infection, most cases are sporadic with the source of the organism and the mode of transmission remaining unknown.
Identification and Virulence Factors
L. monocytogenes is an intracellular pathogen, capable of growth in macrophages, epithelial cells, and cultured fibroblasts. All virulent strains produce a beta-hemolysin, listeriolysin O. This hemolysin is required for release of the bacterium after phagocytosis and intracellular growth. Intracellular survival and spread of the organisms are critically important factors because no other virulence factors have been identified.
Listeria can grow on most conventional media. Small, round colonies appear on agar media after incubation for 1 to 2 days. Because of its morphology and hemolysis pattern, L. monocytogenes occasionally is mistaken for Corynebacterium or streptococci. Laboratory identification is based on the presence of a narrow band of beta-hemolysis on blood agar and on its unique tumbling motility when grown at 20°C to 25°C.36 Polymerase chain reaction can identify L. monocytogenes within hours.37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree