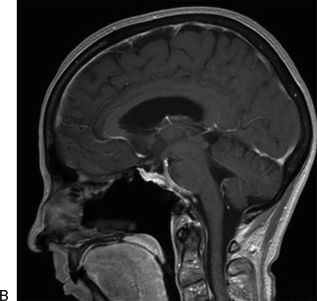
FIGURE 35.1 A. Preoperative CT angiogram sagittal reconstruction showing a petroclival meningioma that requires a pituitary transposition for access to the upper pole of the tumor. The dashed arrow shows the corridor of access achieved following transposition. B. Sagittal MRI following endonasal resection with pituitary transposition.
Tumors that are intimately involved with the posterior cerebral arteries (PCAs) can be difficult to safely dissect without adequate exposure of the capsule of the tumor. Removal of the dorsum sellae or complete gland transposition provides excellent exposure and access to this region. Rare basilar or PCA aneurysms could be accessed as well (Fig. 35.2), though this requires significant experience and very careful patient selection.
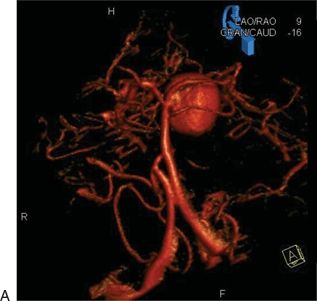
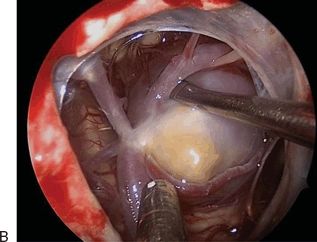
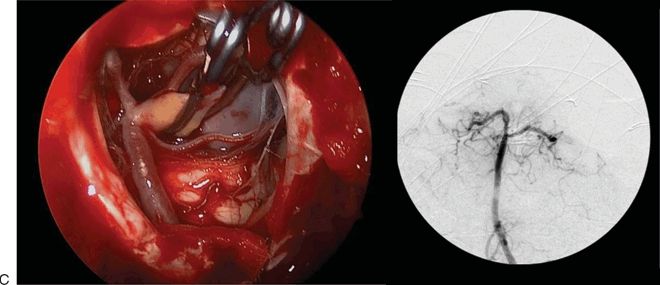
FIGURE 35.2 A. Preoperative CTA showing a three-dimensional reconstruction view of a large PCA aneurysm causing an oculomotor nerve palsy. B. Intraoperative view of the aneurysm before clipping. C. Intraoperative view of the aneurysm after clipping. Intraoperative angiogram showing complete obliteration of the aneurysm and patency of normal basilar apex branches.
CONTRAINDICATIONS
Sinus infection is a contraindication to endonasal intradural (or potentially intradural) tumor resection. However, this can usually be cleared in a short period of time, with antibiotics, surgical drainage, or a combination of therapies. Otherwise, there are no absolute contraindications, though care must be taken to evaluate the relationships of the upper cranial nerves to the mass, especially when it originates laterally such as a petroclival meningioma. If the majority of cranial nerves are displaced medially, a lateral or posterolateral approach is preferable.
Finally, the pituitary transposition approach requires the use of angled endoscopy and a comfort level with management of the cavernous and intercavernous sinuses, basilar venous plexus and the paraclival, and parasellar internal carotid artery (ICA) and its branches. This requires a surgical team with significant prior experience performing endoscopic skull base surgery.
PREOPERATIVE PLANNING
Both magnetic resonance imaging (MRI) and computed tomography angiography (CTA) are important in planning any clival approach. They provide complementary information: MRI shows specific tumor characteristics that may narrow the differential diagnosis and demonstrates the relationships of the nerves to the tumor (especially with FIESTA or fine-cut T2 imaging); CTA reveals bone involvement in the form of erosion or hyperostosis and ICA and basilar artery relationships. It is especially critical to evaluate the size and height of the posterior clinoid processes (PCPs). If there is any sign of calcification of the dural ring or petroclinoidal ligament, dissection behind the ICA can result in potential disaster if this calcified spike is unknowingly manipulated into the artery.
Both MRI and computed tomography (CT) should also be closely examined for signs of sinus infection or other associated sinonasal pathology.
Hormonal evaluation with a full pituitary panel should be performed to document and treat preoperative dysfunction and provide baseline levels for comparison following surgical manipulation of the gland.
Preoperative treatment with corticosteroids is useful for patients with new or progressive neurologic deficits. A full course of antibiotic therapy with careful preoperative reevaluation for clearance of infection is important in patients with identified sinusitis.
SURGICAL TECHNIQUE (SEE VIDEO 35.1)
The superior clivus can be approached endonasally in one of the three ways: extradurally, interdurally, and intradurally. These approaches provide an increasing degree of access to the upper clivus as well as increasing risk of pituitary dysfunction. Both factors should be balanced for optimal tumor management. A purely extradural dissection has almost no risk of permanent pituitary failure but provides limited exposure in cases of extensive clinoid involvement or a “tall” dorsum sellae, whereas an intradural transposition allows complete, unencumbered access to the dorsum, clinoids, and perimesencephalic cistern but may carry a high risk of hypopituitarism from loss of venous drainage and manipulation of the gland.
As with any endoscopic endonasal approach, the surgery is performed by a surgical team consisting of an otolaryngologist and a neurosurgeon. The patient’s head is typically fixed in headpins to prevent inadvertent movement with the head slightly extended and rotated toward the surgeons. The nasal cavity is decongested with oxymetazoline-soaked pledgets immediately following induction. After image guidance is registered, the midface and abdomen (in the rare likelihood of needing an adipose tissue or muscle graft) are prepped and draped. A third- or fourth-generation cephalosporin or equivalent coverage for nasal flora with cerebrospinal fluid (CSF) penetration is given for antibiotic prophylaxis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


