Chapter 38 Drug Delivery
A brief history of the field of drug delivery
The most common form of administration of a medication is the pill. There is evidence of the use of pills at least as early as ancient Egypt in the Ebers Papyrus (1500 bc). They consist, generally, of a medication mixed with a number of excipients or additives such as sugars and starches to protect and stabilize the formulation.1 The basic concept is that one swallows the pill, it dissolves in the stomach, and the medication is absorbed in the intestines to the circulation. This approach works well for many drugs, but not for those which can break down in the stomach. Insulin is usually presented as a case in point which must be injected because it cannot survive the environment of the stomach. Insulin is injected into the fatty tissue2 and is then absorbed into the systemic circulation.
Systemic administration of medications by either route can be problematic for certain tissues, particularly those with strong barrier characteristics or those which are poorly vascularized. Early versions of local delivery systems to the eye involve ointments which were described in ancient Mesopotamia.3 Pilocarpine drops have been used for at least 100 years to lower intraocular pressure (IOP) and treat glaucoma.4
Drug delivery systems are a broad area that includes targeted systems as well as systems that provide controlled release of the drug. One of the earliest targeted systems was the liposome, which has been shown to build up in tumors due to the enhanced permeation effect.5 Liposomes were discovered in the 1960s and the first US Food and Drug Administration (FDA) approval came with Doxil, the liposomal-encapsulated formulation of doxorubicin, an anticancer agent in the 1990s.6 More recent variants on targeted systems have focused on adding molecules on the outside of liposomes or other nanoparticles that can allow them to target the tissue of interest.7 Targeted systems may allow the systemic delivery of a molecule that is released in the ocular tissues.8 However, in and of themselves, targeted systems do not provide sustained delivery of drugs. They can be engineered to do so, but if one looks at the half-life of doxorubicin, it is still on the order of hours as opposed to days or weeks. This does not mean that targeting cannot be combined with sustained delivery, but they are two components to consider.
Sustained delivery is better termed controlled delivery. The fundamental difference is that controlled delivery is dictated by the device and not the environment around the device.9 This is fundamental to the drug delivery. One does not want to administer a device to a patient and have different patients get the drug over different time courses, particularly in an unexpected way. One of the first controlled delivery systems was actually in the eye, the Ocusert system to deliver pilocarpine for glaucoma. The Ocusert system is a reservoir system that relies on the transport of the drug through a membrane. Membranes are effective for small molecules (less than 600 Da),10 but are not suitable for delivering larger molecules such as antibodies, growth factors, and proteins more broadly.
The watershed in the drug delivery world occurred in 1976. Robert Langer and Judah Folkman showed that large molecules could be delivered over days and weeks from polymer matrices, and they showed that the release profile could be tailored based on the matrix.11 The concept was not warmly received and there were huge questions about the mechanism and plausibility of the approach,12 but the drug delivery field has grown from being nonexistent in the USA in the 1980s to 11.5 billion dollars in 1996,13 to an estimated 85 billion dollars in 2010.14 The economic impact is a reflection of a number of factors, including the ability to provide new patent protection for off-patent medications, but it also reflects the impact on human health.
Drug delivery
Formulating sustained-delivery systems
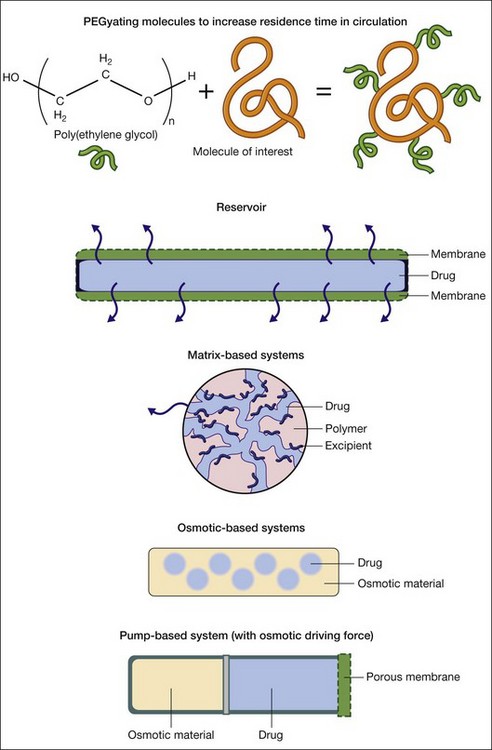
There are five broad approaches for the sustained delivery of drugs (Fig. 38.1). The first approach involves attaching molecules to the drug to increase its residence time. Poly(ethylene gycol) or PEG is the workhorse of this approach. PEGylating or attaching PEG molecules can increase the circulation time of a drug in the bloodstream by creating a highly hydrated volume around the drug.15 The second broad approach is to encapsulate the drug of interest in a reservoir system that includes a membrane that allows the drug to diffuse through the device and into the surrounding tissue. This approach lies at the basis of drug delivery systems, including the Ocusert implant delivering pilocarpine.16 Diffusion-based systems work for limited, typically small, molecules with molecular weights less than 600 Da.10 There are great benefits to the membrane-based systems, such as the ability to deliver many drugs over very long timescales, but there are risks, including the rupture of the membrane, leading to spontaneous delivery of the entire reservoir.9
The third approach involves mixing the drug with polymers which entrap the drug in a matrix. The drug typically phase separates on the micro- or nanoscale from the polymer, leading to veins of the drug in the polymer matrix. The tortuosity of the veins plays a tremendous role in the release of the drug. With nondegradable polymers, the drug delivery profile is dictated by diffusion.17 With degradable polymers, the drug delivery profile is dictated by a combination of diffusion and degradation events that occur over time.17 The challenges in the matrix-based approaches involve achieving good mixing of the drug in the matrix to form tortuous pathways as well as promoting interactions between the drug and matrix. The closer the two associate with each other, the more likely one will achieve very long (weeks to months to years) release. Thinking about this interaction becomes part of the process of formulating drug delivery systems.
The fourth approach involves osmotic systems. In these systems the diffusion of water into the matrix leads to swelling and drives the release of the drug via diffusion. Typically, osmotic systems lead to relatively fast release of drugs with a significant burst effect. Investigators are developing asymmetric membranes to control the delivery in a more uniform manner over time,18 but osmotic systems have not been used extensively other than as components to drive pump technologies which do have robust, long-term delivery.
In thinking about which approach makes the most sense in formulating a drug delivery system, one needs to consider the following: the size, nature, and stability of the drug, the length of time one wants to deliver the drug, and the amount of the drug one wants to deliver over time. Regarding size, small molecules (<600 Da) can diffuse through polymers such as silicone.10 Larger molecules, macromolecules such as proteins, are not able to diffuse through polymers on a useful timescale for most applications.11 If one is hoping to deliver larger molecules, one will need to consider the methods outside of the membrane approach.
The nature of the drug refers to its charge and solubility. Most of the popular biodegradable polymers are extremely hydrophobic. If the drug of interest is very hydrophilic, it can be challenging to encapsulate the hydrophilic drug in the hydrophobic polymer matrix. One of the classic methods to overcome this challenge is to use excipients that interact with both the drug and the polymer. Fu et al. showed how excipients could greatly improve loading and delivery of glial cell line-derived neurotrophic factor (GDNF) through the use of excipients.19 Likewise, charged molecules can interact poorly in uncharged or similarly charged polymer systems. Poly(lactic-co-glycolic acid) (PLGA) can be synthesized with a carboxyl group on the end that carries a negative charge depending on the pH. This can improve the encapsulation of positively charged molecules.
Beyond the drug, one needs to consider the amount of the drug one needs to deliver and the time course. Matrix-based formulations have been shown to deliver medications for years, but they rely on relatively high polymer-to-drug ratios, which makes them more suitable for applications where one can either deliver a large volume of material (which is unlikely in the eye) or where one has a relatively potent medication. As we will see in the examples below, many of the commonly used drugs are effective at low concentrations, but it is an important consideration. Membrane and pump systems can both deliver larger amounts of drugs over time, but the volume they deliver determines the necessary reservoir size and overall device dimensions. The time course is the second critical component. Membrane and pump approaches can both lead to very constant delivery depending on the geometry of the devices.10 Careful formulation can lead to very constant delivery over time from matrix-based formulations, but they are prone to burst release due to drug adsorbed on or near the surface of the materials.10
Delivering drugs in a targeted manner
For some compounds, though, one may want either to deliver them systemically or to deliver them to a particular cell type in the eye and not to all cell types. A good example of this would be the delivery of a specific agent for a specific cell type, such as the retinal pigment epithelium (RPE).20 The most common forms of targeting have involved creating particles, typically nanoparticles, from either liposomes or other polymers that are covered in PEG arms to reduce their aggregation and promote transport, and attaching molecules to the particles that bind to receptors or molecules on the cells of interest. Antibodies,21 peptides,22 and aptamers23,24 have all been used to facilitate targeting.
The key issues to consider in designing a targeting molecule are the specificity and affinity of the targeting moiety to the molecule of interest on the cell. Poor affinity or specificity will lead to poor targeting. Once one has identified targeting molecules with appropriate affinity and specificity, one needs to insure the stability of targeting molecule in vivo. Larger molecules, such as antibodies, have the potential to be denatured or enzymatically cleaved in vivo, which has motivated the identification of smaller molecules with similar specificity and affinity such as aptamers.23,24
Targeting is primarily used to concentrate systemically administered particles in the tissue of interest. In the retina, much of the work has focused on targeting the choroidal vessels.25,26 There is evidence that, when particles are small enough, they can cross through to the retina when administered systemically,27 which opens up the possibility of delivering targeted nanoparticles to the retina via systemic administration.
Gene delivery
Gene therapy has the potential to replace or restore function in the retina as well as produce growth factors which protect the eye. It is very challenging, though, to get the genetic material both to the cells and into the genome without breakdown of the material. There have been many studies looking at the transfection efficiency of deoxyribonucleic acid (DNA) through routes of administration, including drops, subconjunctival, intravitreal, and subretinal injections, and in all cases the transfection efficiency has been low to the retina and the subsequent protein expression is typically small and over a short duration.29
To facilitate more effective delivery of DNA and subsequent protein expression, a number of vectors have been pursued. The two basic approaches involve viral and nonviral delivery of constructs to the retina. Viruses have adapted over millions of years to deliver genes to cells efficiently, and viral delivery is generally efficient. Viral delivery does raise safety concerns and there were substantial complications and deaths in early viral-based gene therapy trials.30,31 Nonviral gene delivery has sought to provide safer alternatives, but the challenge lies in getting efficient delivery and incorporation of the genetic material.
Viral systems
There are three major classes of virus that have been used for transduction: retroviruses, lentiviruses, and adenoviruses. Retroviral vectors only infect dividing cells, making them relatively unattractive for ocular applications.32 Lentiviral vectors are designed to infect nondividing cells in the G0 or G1 phase of the cell cycle.32 There are significant safety concerns with both retroviral and lentiviral vectors because they have the potential to insert into the genome. Of the three major classes, adenoviruses have drawn tremendous interest for gene therapy because they do not incorporate into the genome, which is thought to reduce their oncogenic potential, and they are extremely effective at transducing cells.32 However, adenoviruses have been found to be very immunogenic, and one of the early clinical trials using an adenovirus had to be halted when an 18-year-old died due to a systemic inflammatory response syndrome.31
Adenovirus-based vectors have continued to be pursued in the eye because of the local delivery and immune-privileged nature. GenVec has used an adenovirus to deliver the gene for pigment epithelium-derived factor (PEDF) for the treatment of neovascular AMD in a phase I trial.33 The adenovirus-based delivery system was well tolerated by patients with only transient, mild inflammation in some patients which was managed with topical medications. There was no control group in this phase I trial, but the size of the choroidal neovascular lesions was smaller in the high-dose group. Much of the follow-on research has focused on repeated administrations, longer-term expression of PEDF, and using inducible promoters to direct expression of the protein of interest.34–36
A variant on the adenovirus, first found as a contaminant of adenoviruses, the adeno-associated virus (AAV), has proven to be an effective alternative. Like adenoviruses, AAV vectors do not integrate into the genome. Furthermore, they do not elicit a strong immune response.32 One of the first major successes for gene therapy with AAV vectors has been the treatment of Leber congenital amaurosis, a severe form of retinal degeneration that leads to vision loss in early childhood.37 A replication-deficient AAV vector was used to deliver a gene for isomerohydrolase activity (AAV-hRPE65v2). The vector was injected subretinally, and vision gains were found in younger patients.
Nonviral systems
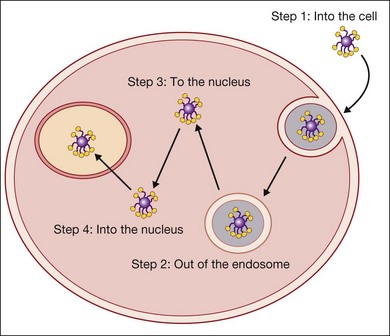
There are five basic steps that have to be achieved to transfect a cell (Fig. 38.2). The genetic material must get to the cell, into the cell, out of the endosome, to the nucleus, and into the nucleus. Viruses have evolved a complex set of tools to achieve this. For example, the adenovirus has a targeting moiety for the cell of interest and leverages the pH drop in the endosome by having the capsid undergo a conformational change which opens the endosome. It is thought to bind to dynein, a molecular motor that moves along the microtubules to travel to the nucleus.38
Nonviral systems have been designed to address one or more of these issues, and the more recent systems have been designed to address several or all of these critical steps for transfection. Liposomes were among the earliest transfection agents. Liposomes are capable of shielding DNA from enzymatic breakdown until the material gets to the cell, but their fusion with the cell membranes is not efficient.39 However, in 1987, the use of cationic liposomes was first identified as a means to facilitate high rates of transfection.40 The cationic component of the system facilitates interactions with the negatively charged cell membranes and the subsequent cell fusion which delivers the DNA into the cell. While this is a tremendous improvement over previous nonviral approaches, the efficiency is still far lower than viral systems.
Positively charged polymers like polylysine and polyethylenimine (PEI) were very early in the nonviral vector development timeline. PEI, one of the major cationic polymers, was first shown to be an effective polymer for gene delivery in 1995.41 It does two critical things. First, it is a positively charged polymer that complexes with negatively charged DNA to create positively charged nanoparticles which stick to the anionic membranes of cells. Second, it is a proton sponge, meaning that as the pH is lowered in the endosome, the amines on the polymer take up the hydrogen ions and the polymer protonates. It does this to the point that it swells and bursts the endosome. The polymer, however, has no specific method for getting the DNA to or into the nucleus. PEI tends to be most effective in dividing cells where the organization of the mitotic spindles facilitates movement of the particles to the nucleus.41,42 PEI has been used in animal models for transfection of retinal cells.43 The particles were taken up primarily by what appear to be Müller glial cells but no quantification is discussed so it is not possible to assess what sort of efficiency was achieved.
In light of the complexities of getting DNA to the nucleus, more recent research has focused on developing multicomponent systems that incorporate protection of DNA with endosomal escape mechanisms and nuclear targeting moieties.44–46 The challenges of specific transfection of retinal cells in the eye with nonviral vectors are significant, and it is likely that careful engineering of the vector will be needed for successful, long-term transfection, but the field is moving forward rapidly. It is likely to be a very different landscape in the next decade.
Cellular delivery for sustained drug delivery
Engineering cells for delivery
The attraction of using cells for the delivery of therapeutic agents is that cells can deliver a molecule for very long periods of time, potentially years. Furthermore, cells have the potential to integrate into the retina and deliver molecules in layers that may not be easily reached by standard drug delivery of gene therapy approaches. For example, it can be challenging to deliver genes to the retina and to get robust expression of the molecule of interest via intravitreal injections.47 However, there are studies showing that certain cells may be able to migrate and integrate with the retina following intravitreal administration and produce molecules such as GDNF and brain-derived neurotrophic factor (BDNF) to preserve retinal cells in a number of models of retinal degeneration.48,49 Mesenchymal stem cells,49 embryonic stem cells,48 Schwann cells,50 and fibroblasts51 have all been engineered as a means to promote neuroprotection and have all successfully been used for several months in animal models.
Engineering materials for immunological protection
While the eye is immune-privileged,52,53 the presence of disease can alter this privilege, and long-term survival of transplanted cells is not guaranteed. Since the primary purpose of the engineered cells is to deliver their molecular payload, encapsulating them to protect them from the host while allowing their molecules to reach the retina makes a great deal of sense. It also facilitates their removal should complications arise.
As noted in the section on sustained delivery systems, solid polymer membranes do not allow large molecules (> 600 Da) to diffuse through.10 Most of the growth factors noted above are significantly greater than 600 Da. The solution, then, is to engineer the materials with higher-molecular-weight cutoffs that allow the growth factors through but still block the transport of antibodies and other larger molecules.
Alginate gels and variants on alginate gels have been one of the most used materials to encapsulate cells for this purpose since the early 1980s. Alginate is an attractive material in that it does not adsorb proteins, facilitating their transport, but the molecular weight of the transported molecules can be controlled by the crosslinking density.54–56 Because alginate gels are crosslinked water-swollen gels, the encapsulated cells are able to remain hydrated and transport of nutrients and waste is maintained. Other materials, primarily synthetic hydrogels, have become popular because the permeability can be tightly controlled through crosslinking agents and density, membrane thickness, and the use of multiple layers.57,58 Kristi Anseth’s group has shown that functionalizing hydrogels with moieties that interact with cells can still maintain the long-term delivery of the protein of interest while leading to higher and longer-term cell viability, the ultimate goal of these encapsulation systems.59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree