CHAPTER 110 Conservation Laryngeal Surgery
A variety of open surgical approaches are available. When applied for the appropriate indications, they have an excellent ability to control laryngeal cancer while conserving laryngeal function. Conservation laryngeal procedures are historically the original “organ-preservation” techniques; the first hemilaryngectomy for malignancy was performed by Billroth in 1874.1 Long before nonsurgical approaches were available to attempt to preserve the entire structure of the larynx, innovative surgical techniques were being used to remove enough of the larynx to allow for local control of the malignancy while preserving adequate structure to allow the larynx to function.2 There exists a spectrum of laryngeal malignancies for which there is a complementary spectrum of conservation laryngeal procedures available. This chapter reviews the open conservation laryngeal procedures in the organ-preservation surgical paradigm available for managing the spectrum of selected glottic, transglottic, and supraglottic carcinomas. These techniques allow for the maintenance of physiologic speech and swallowing without the need for a permanent tracheostoma. The modern head and neck surgeon must have a comprehensive understanding of both surgical and nonsurgical organ-preservation strategies to allow for the most comprehensive care in the treatment of the patient with laryngeal cancer.
The common thread in the history of conservation laryngeal surgery is that these procedures were first developed outside the United States and then imported to its shores. Improvements in antibiotics and anesthetic techniques fostered the development of conservation laryngeal surgery.3 Vertical hemilaryngectomy, which was first described by Billroth1 in Germany and popularized in Europe by Leroux-Robert and Portmann,4 was refined in the United States by Som,5 Norris,6 and Conley.7 A French surgeon named Huet described a procedure in which a portion of the supraglottis was excised without the upper portion of the thyroid cartilage in 1938.8 Later, a Uruguayan surgeon named Alonso extended this procedure to resect the upper portion of the thyroid cartilage together with the supraglottic structures, thereby defining the supraglottic laryngectomy.9,10 The supraglottic laryngectomy was popularized in Europe by Bocca11 and in the United States by Ogura,12 Som,5 and Kirchner.13 The supracricoid laryngectomies originally were described in 1959 by the Austrian surgeons Majer and Reider14 approximately one decade after Alonso had described the supraglottic laryngectomy.9 The supracricoid laryngectomies were later promoted in Europe by Labayle15 and Piquet and associates16 and were imported to numerous institutions in the United States during the 1990s.17
The first of two major classes of techniques that developed was the vertical partial laryngectomy, in which entry into the endolarynx is through a vertical thyrotomy, the most notable example of which is the vertical hemilaryngectomy. The second major class of techniques is the horizontal partial laryngectomy, in which endolaryngeal entry is made through a transverse or horizontal thyrotomy (i.e., supraglottic partial laryngectomy). During the 1960s through the 1980s, innovative surgeons18–23 reported numerous small series of patients in which the indications and extent of resection of these basic techniques were extended in an attempt to manage larger lesions. The commonalities among these series were (1) the relatively small numbers of patients; (2) variable local control rates compared with the strict previous indications for the procedure that was being extended; and (3) complex reconstructions requiring cartilage and mucosa rotation flaps with variable functional results.18–25 These variable results made it difficult for other surgeons to use these extended procedures in the treatment of larynx cancer. Despite these innovations of the pioneers of conservation laryngeal surgery, the techniques that most surgeons became facile with, as reflected by the large numbers of series in the literature, were the standard vertical hemilaryngectomy and standard supraglottic laryngectomy. A common surgical solution in the United States for lesions considered too large for these standard conservation laryngeal procedures was total laryngectomy, with the innovations being in the area of alaryngeal speech and speech shunt development.26,27
In many European countries, laryngectomy, with its concomitant permanent stoma, was considered an anathema to be avoided when possible, and a different approach evolved. In 1959 in Austria, Majer and Reider14 reported on a new horizontal partial laryngectomy technique in which the entire thyroid cartilage, true cords, false cords, and all or a portion of the epiglottis and preepiglottic space were resected. The reconstruction was with a pexy either between the cricoid and hyoid (cricohyoidopexy) or between the cricoid and the remaining epiglottis and hyoid (cricohyoidoepiglottopexy). This procedure, known as the supracricoid partial laryngectomy, allowed for a complete resection of the preepiglottic and paraglottic spaces and of the surrounding cartilage and soft tissue, resulting in higher local control in glottic, supraglottic, and transglottic cancers that equaled total laryngectomy, resulting in speech and swallowing without a permanent tracheostomy. Unlike the plethora of extensions of the vertical partial laryngectomy and the supraglottic laryngectomy, the supracricoid laryngectomies were repeated in many patients by numerous European centers during the 1970s through the 1990s with consistently excellent local control and functional results.16,28–37
Conservation Laryngeal Surgery Today
The focus of this chapter is to provide the general otolaryngologist–head and neck surgeon with an introduction to these techniques. This information is important because it is the responsibility of the general otolaryngologist–head and neck surgeon to understand the indications for the full spectrum of open and endoscopic organ-preservation surgical approaches and either gain the expertise to perform these procedures or refer the patient to surgeons who have this special expertise.38
During the 1970s and 1980s, the functional and oncologic results after supraglottic laryngectomy were reported in numerous series in the United States, defining the role of this technique among the plethora of surgical and nonsurgical options available for supraglottic carcinoma.39–41 During the same period and into the 1990s, the role of vertical partial laryngectomy for glottic carcinoma has been re-examined because of advances in nonsurgical and laser endoscopic approaches to similarly staged disease.3,42 In the 1990s the supracricoid laryngectomies were imported to numerous institutions in the United States, and the European functional results have been reproduced.17,43,44 The supracricoid laryngectomies have broadened the spectrum of reliable techniques available to the conservation laryngeal surgeon.3
At present, a renaissance is occurring in the United States in the area of conservation laryngeal surgery. Many factors have fostered the rekindled interest in conservation laryngeal surgery, including (1) a clearer understanding of the three-dimensional extent of laryngeal carcinoma, which has stemmed from numerous clinicopathologic studies and from advances in radiologic techniques; (2) numerous long-term studies of outcome after the application of a broad spectrum of techniques; and (3) the introduction of new techniques during the past 2 decades. Today, there are a variety of techniques available for selected laryngeal malignancies, with predictable functional and oncologic outcome based on analyses in the literature of many patients. The full spectrum of surgical techniques allows the surgeon to consistently offer patients, with selected lesions, excellent local control that will result in speech and swallowing without the need for a permanent tracheostoma. This may provide the patient with an alternative to nonsurgical organ-preservation modalities. There are organ-preservation principles to which the surgeon must adhere to maximize both oncologic and functional outcome. Conservation laryngeal surgery is precision surgery,45 and to achieve successful oncologic and functional results, the conservation laryngeal surgeon should have a firm grasp on the clinical assessment of laryngeal cancer and a complete understanding of the surgical techniques. The art of correctly staging the lesion as one appropriate for a conservation laryngeal procedure requires an in-depth knowledge of both the static and dynamic anatomy of the larynx and how the tumor relates to it.
Anatomy, Physiology, and Tumor Spread
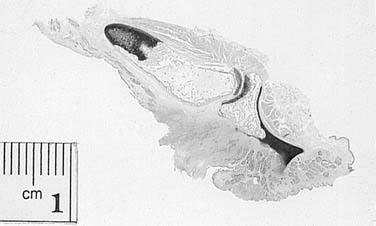
In 1966 Bocca elegantly stated that, “often cancer seems to have limits, while the surgeon seems to have none. We should make efforts to force upon our knife the same limits as those which surrounding tissues or structures force upon cancer and its spread.”11 Bocca’s eloquent statement underscores that successful outcome in conservation laryngeal surgery is predicated on a thorough knowledge of the pertinent surgical anatomy and on an understanding of the behavior of the malignancy in a particular anatomic site. Much of what is known concerning the three-dimensional spread of malignancy through the larynx has been derived from clinicopathologic studies in which the entire larynx was sectioned. These whole organ section studies are the basic science foundation for clinicians performing conservation laryngeal surgery.
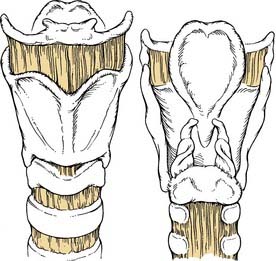
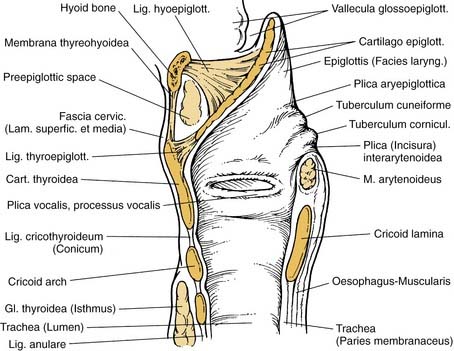
The surgical anatomy of the larynx can be understood in terms of the skeleton and connective tissue barriers, the spaces delineated by these structures, and the soft tissue structures, which include the fat, musculature, vessels, nerves, and adnexa that fill these spaces. The skeleton of the larynx (Fig. 110-1) is dominated by the thyroid cartilage, which articulates posteriorly and inferiorly through the inferior cornua with synovial joints on the posterolateral aspects of the cricoid cartilage. A thick tendon originates from the superior cornua and attaches to the lateralmost aspect of the “crown” of the larynx, the hyoid bone. Anteriorly there is a notch, and the lateral aspect of the laminae is traversed by the oblique line, which is the point of attachment of the strap musculature. The extension of cancer into the thyroid cartilage tends to occur in areas of ossification of the cartilage.46 The mode of invasion into the ossified bone has been attributed to osteoclast formation,47 extension along collagen bundles,48 or through areas of high vascularity.49 The most common site of invasion of the thyroid cartilage was at the angle,50 although other sites of predilection for carcinoma invasion are the points of attachment of the cricothyroid membrane and the anterior origin of the thyroarytenoid musculature.48 The perichondrium provides an excellent barrier to invasion, and once the carcinoma is within the cartilage, the cancer can extend throughout the cartilage behind an intact perichondrium, precluding surgical cuts through the cartilage, as is done in some partial laryngectomies.51 Nakayama and colleagues52 noted that a large proportion of patients staged clinically as T3 actually had thyroid cartilage invasion when the specimens were analyzed by whole organ sectioning, and they noted that in these patients with T3 glottic cancers, any combination of two factors including significant degree of calcification of the cartilage, tumor length greater than 2 cm, and anterior commissure involvement resulted in a higher incidence of cartilage invasion (71% to 92%).
The cricoid cartilage is the only circumferential ring in the airway, and preservation or reconstruction of its ring-shaped structure allows for decannulation after conservation laryngeal surgery. The arytenoid cartilages sit atop the cricoid, to which they are attached by a synovial joint. The two muscular processes of the arytenoid cartilages are oriented posteriorly and laterally, and the vocal cord tendon originates from the tip of the vocal process and spans anteriorly to the thyroid cartilage. The most common site of cricoid cartilage invasion by carcinoma is at its posterior superior border, and the most common site of arytenoid invasion is at the points of attachment of the joint capsule.53
The epiglottis, with its numerous fenestrations, originates from the tendinous attachment on the thyroid cartilage, fanning out from its most inferior point known as the petiole to a widened superior aspect above the hyoid. The carcinoma on the infrahyoid surface of the epiglottis readily extends through the fenestrations of the epiglottic cartilage through blood vessels49 and the ducts of the seromucinous glands.54 The hyoid bone is almost never involved by supraglottic carcinoma. Kirchner55 noted no cases of hyoid bone invasion in 55 supraglottic carcinomas evaluated by whole organ section, although in Kirchner’s series,55 two patients had cancer up to the periosteum, one of which could be palpated at the level of the thyrohyoid membrane and one which had vallecula mucosa involvement. Among 172 patients with supraglottic carcinoma reported by Timon and colleagues,56 only four patients had hyoid bone invasion, and a common feature of all of these patients was vallecula mucosal involvement. Preservation of the hyoid bone helps with swallowing postoperatively. Understanding this concept is essential and makes it possible to perform supracricoid laryngectomy with cricohyoidopexy in selected transglottic tumors. These authors concluded that it is sound to preserve the hyoid bone in cases without palpable submucosal vallecula carcinoma or vallecula mucosal involvement.55,56
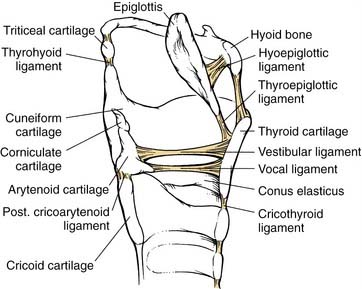
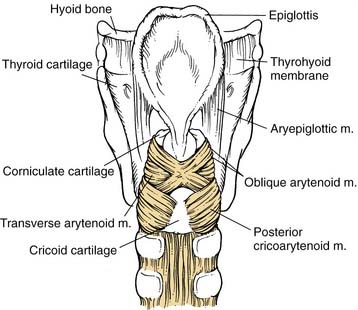
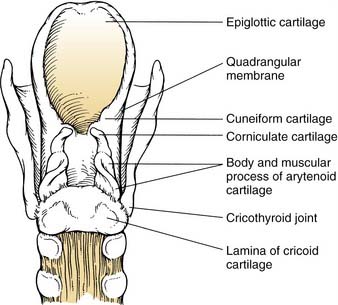
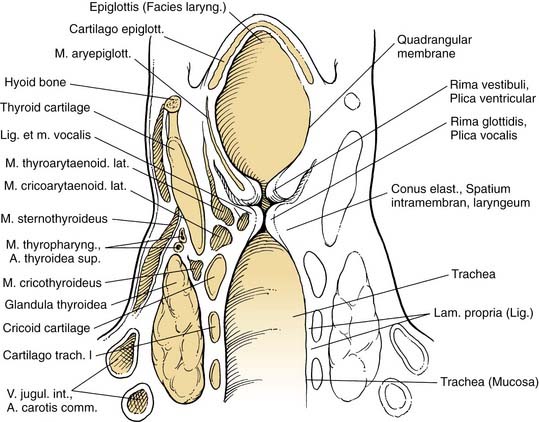
There are numerous condensations of fibrous tissue that traverse the three-dimensional anatomy of the larynx. Some of the modern knowledge of these structures comes from the pioneering work of Tucker and Kirchner, both of whom studied whole organ sections of larynges and analyzed this anatomy.57–59 The conus elasticus (Fig. 110-2) spans from each vocal cord down laterally to the cricoid cartilage. The conus elasticus provides a temporary barrier for the spread of early glottic carcinoma, but ultimately, for larger cancers, it serves as the gateway to the subglottic and extralaryngeal spread of carcinoma.60 Posteriorly, it is also attached to the arytenoid, providing stability to the arytenoid and the vocal tendon. The vocal tendon, which essentially is a medial condensation of the conus elasticus, attaches anteriorly to the thyroid cartilage at the Broyles ligament or the anterior commissure tendon.61 Although the anterior commissure tendon is devoid of perichondrium, the ligament constitutes a dense fibrous attachment to the cartilage and sends slips of fibrous tissue superiorly to the thyroepiglottic ligament. Kirchner and Carter60 have noted that the anterior commissure tendon is a point of dense adhesion of fibrous tissue, and it is rare for an early glottic cancer with anterior commissure involvement to erode into the thyroid cartilage here. However, the anterior commissure tendon provides access to cartilage invasion for larger cancers, which spread superiorly or inferiorly.60 Anteriorly, there is a superior inferior condensation of the conus elasticus called the cricothyroid ligament, which is a central structure and does not spread out laterally to provide a connective tissue barrier along the circumference of the cricoid.50 This is different than its superior counterpart, the thyrohyoid membrane. The thyrohyoid membrane drapes along the entire circumference of the thyroid cartilage superiorly and spreads upward to the hyoid bone (Fig. 110-3). Extension out of the larynx through the thyrohyoid membrane alone is rare and is typically seen when cancer exits the larynx through the upper portion of the thyroid cartilage.50 The quadrangular membrane (Fig. 110-4) originates from the top of the arytenoid posteriorly and from the lateral aspect of the epiglottis anteriorly and then extends inferiorly like a curtain to an inferior condensation of fibrous tissue, which spans between the inferior aspect of the arytenoid posteriorly and the petiole of the epiglottis anteriorly. The hyoepiglottic ligament was recently elegantly described by Zeitels and Kirchner,62 who showed this structure to be a resilient barrier to malignant spread from the supraglottis to the tongue base when the cancer is confined to the laryngeal membranes and does not clinically invade the suprahyoid epiglottis.
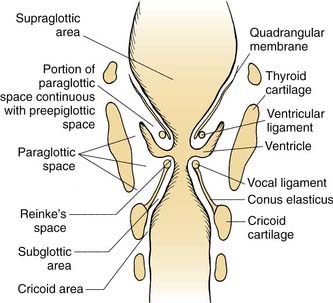
The skeleton and fibrous tissue barriers demarcate a number of spaces within the larynx. The superiormost space is the preepiglottic space (Fig. 110-5), which is filled with fat and traversed by blood and lymphatic vessels.63 Kirchner and Carter60 noted that carcinoma tends to invade within the preepiglottic space with a “pushing edge,” which is almost “encapsulated” after it reaches the elastic tissue membranes in the preepiglottic space, contributing to the oncologic safety in saving the hyoid bone during supraglottic surgery. The boundaries of this space are the vallecula mucosa and the hyoid superiorly, the thyrohyoid membrane and the thyroid cartilage anteriorly, and the epiglottis posteriorly. Posterolaterally, on either side, the preepiglottic space is bounded by the superior portions of the paraglottic space.64
There is a paraglottic space on either side of the larynx (Fig. 110-6). Superiorly, the medial boundary is the quadrangular membrane, whereas inferiorly, the medial margin is the conus elasticus. It originates superiorly within the aryepiglottic fold, where it fades to a peak. The paraglottic space makes up the substance of the true and false cords and within it are the thyroarytenoid musculature and the mucosa-lined, air-filled space known as the ventricle and its superior extension, the saccule. Inferiorly, it follows the conus elasticus down to the top of the cricoid cartilage. Anteriorly, it abuts the preepiglottic space and the anterior third of the thyroid cartilage, and the posterolateral boundary is the mucosa of the medial aspect of the pyriform sinus. The paraglottic space traverses the supraglottis, glottis, and subglottis laterally within the larynx. Rather than having a distinct barrier to superior-inferior spread, cancer seems to be impeded in its course through the paraglottic space to varying degrees by the hourglass shape of the space, which is made by the indentation of the ventricle and saccule.65 One additional space is Reinke’s space, which actually is a potential space under the true vocal cord mucosa and provides no barrier to invasion.
The behavior of carcinoma in the supraglottis is modified by the soft tissue, connective tissue barriers, and the skeleton of the larynx (Fig. 110-7). Kirchner57 showed, in an analysis of whole organ sections, that supraglottic carcinomas that overlie the epiglottic cartilage have a tendency (9 of 10 cases) to extend into the preepiglottic space, at least microscopically, through the fenestrations in the epiglottic cartilage. In addition, Bridger,54 working with the whole organ section collection at Johns Hopkins, showed that seromucinous tubuloalveolar glands extend through the fenestrations and provide a route of spread of cancer into the preepiglottic space. Although it had been suggested in the past that embryologic fusion planes somehow provide protection against inferior spread of carcinoma from the supraglottis to the glottis, a recent study that evaluated all of the series of whole organ sections in the literature revealed that the incidence of spread of supraglottic carcinoma to the glottic level is between 20% and 54%.65 This study indicated that there was a statistically significant relationship between the presence of abnormal cord mobility or involvement of carcinoma below the false cord and glottic level extension, most commonly through the paraglottic space.65
Carcinomas at the glottic level tend to begin at the junction of the anterior one third and posterior two thirds of the vocal cord. They readily pass through Reinke’s space to the tissues below. Early studies by Pressman,66 with submucosally injected dyes and radioisotopes, indicated that barriers existed between the two sides of the glottis and the supraglottis. Welsh and colleagues53 demonstrated that as dye concentration increases, these barriers become less effective. For early lesions, the conus elasticus provides a barrier to extension; as the lesion enlarges, this barrier becomes less pertinent.67
The sensation to the supraglottis is supplied by the superior laryngeal nerves, whereas the glottis and subglottis are innervated by the recurrent laryngeal nerve. The neural structures play an important role in timely postoperative functional rehabilitation.68 Whenever possible, the main trunks of the superior and recurrent laryngeal nerves and the hypoglossal nerves, bilaterally, should be preserved during conservation laryngeal surgery.
Certain aspects of physiology of the larynx are pertinent to successful application of conservation laryngeal surgery. Hirano and colleagues,69 in a whole organ analysis of the normal larynx, noted that 50% to 65% of the entire adult airway is located posterior to the tips of the vocal processes and concluded that the posterior larynx is the respiratory airway and the anterior portion is the phonatory airway. This is because all of the musculature that opens and closes the glottic chink, the lateral cricoarytenoid musculature, changes the position of the vocal processes during speech and swallowing. The arytenoids are responsible for opening the airway for breathing and for closing during swallowing and speaking. The vocal cords provide vocal quality during phonation; therefore loss of one or both vocal cords results in hoarseness, but preservation of at least one arytenoid and an intact circumferential ring at the level of the cricoid is sufficient for speech and swallowing without a tracheostomy.70–75
Principles of Organ-Preservation Surgery
The otolaryngologist–head and neck surgeon must adhere to certain key principles to determine a patient’s eligibility for a conservation laryngeal surgery. The advent of the supracricoid laryngectomy makes us direct our focus away from the vocal fold and concentrate on the cricoarytenoid unit as the essential functional unit of the larynx. The organ-preservation principles are formulated to help provide consistent oncologic and functional outcomes.76 These can then be compared with current nonsurgical organ-preservation options to allow the patient and physician to make educated decisions regarding treatment. Adopting these principles will enable the surgeon to maximize oncologic and functional outcomes for a number of glottic, supraglottic, and transglottic malignancies.
First Principle: Local Control
Local control is the most important principle. Survival from the index cancer is compromised if there is a local failure after radiation therapy or surgery to the supraglottis and glottis.77 Early detection of the primary site recurrence may be difficult for a number of reasons. Medical and surgical organ-preservation modalities alter the topography of the larynx and make definitive evaluation of recurrent cancer difficult. Symptoms may be attributed to the treatment intervention or recurrent tumor, although increasing pain, persistent ear pain, and dysphagia are ominous signs. Repeat endoscopy and biopsy of the original primary site is warranted. Computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) may also be helpful in explaining recurrent or persistent cancer. Organ-preservation laryngeal procedures should be used only when resection of the tumor can be accomplished comfortably with local control rates approximating those of total laryngectomy.
Preoperative Evaluation
Clinical Evaluation of the Primary Site
Before examining the larynx, the physician should listen to the patient speak and breathe. The degree of airway impairment and the voice quality should be assessed. Glottic carcinomas that affect the phonatory structures tend to cause hoarseness; supraglottic cancers frequently are above the cords and cause a muffled “hot potato” voice as they enlarge. Hoarseness from a supraglottic carcinoma may indicate impairment of cord mobility as a result of arytenoid involvement or glottic level involvement. Next, both sides of the neck should be palpated for nodal disease. The thyroid cartilage itself should be palpated for irregularities, as should the areas directly above and below the thyroid cartilage. A bulge or mass at the level of the thyrohyoid membrane may indicate massive preepiglottic space invasion. A mass at the level of the cricothyroid ligament may indicate a Delphian lymph node, which indicates subglottic extension of the malignancy.78 Indirect mirror or fiberoptic laryngoscopy is used to assess the larynx and surrounding structures. The important gross pathologic characteristics that need to be evaluated are airway impairment, endophytic versus exophytic, superficial spread versus deep invasion, mucosal structures involved, arytenoid and vocal cord mobility, and extensions out of the endolarynx.
The clinical assessment of laryngeal mobilities provides excellent insight into the three-dimensional extension of carcinoma within the larynx. Mobility of the vocal cord itself, without attention to arytenoid mobility, is adequate when planning for management that is directed to the entire organ such as total laryngectomy or radiotherapy. Biller and Lawson79 and Ogura’s team80 have noted that assessment of arytenoid mobility and cord mobility is important in the preoperative planning for conservation laryngeal surgery, particularly when the vocal cord itself is fixed. Assessment of vocal cord mobility is best clinically assessed during indirect laryngoscopy by having the patient speak or breathe deeply, whereas arytenoid mobility is best assessed by having the patient cough gently.
Cancers involving the glottis and supraglottis have different effects on vocal cord mobility and arytenoid mobility. Impaired mobility from glottic carcinoma may be a result of superficial thyroarytenoid invasion or bulk on the surface of the cord in an exophytic lesion.67 Hirano and others81 assessed the degree of thyroarytenoid muscle invasion in glottic carcinoma and found fixed cords had deeper invasion into the musculature than impaired cords. Numerous studies have demonstrated that glottic carcinoma associated with a fixed vocal cord most commonly results from extensive invasion of the thyroarytenoid muscle.81–83 In some patients, subglottic extension with fixation to the cricoid cartilage and lateral extension with adherence to the thyroid cartilage resulted in fixation of the cord82 and invasion of the lateral cricoarytenoid musculature and the cricoarytenoid joint.83 At the supraglottic level, cancer invasion into the thyroarytenoid musculature at the glottic level is less likely, and the most common cause of cord fixation, noted by Hirano and others,81 was deep arytenoid cartilage invasion superiorly. Montgomery84 and Ogura85 assessed vocal cord and arytenoid mobility, independently, in preparation for conservation laryngeal surgery of the supraglottis. Brasnu and colleagues,86 in a whole organ section series, noted two types of impairment in arytenoid mobility—namely the “weight impact” of the tumor—in which the arytenoid motion seems impaired superiorly causing “pseudofixation” versus actual fixation from the malignant involvement of the intrinsic laryngeal musculature, the cricoarytenoid joint, or both (Fig. 110-8). They are distinguished by careful evaluation of the vocal fold; if any motion of the cord is noted in the presence of what seems to be arytenoid fixation from a supraglottic cancer, this is “pseudofixation.”86 This information is valuable to the conservation laryngeal surgeon because it is unlikely that a larynx with a “pseudofixed” arytenoid has cricoarytenoid joint and musculature involved, whereas these areas are involved in more than two thirds of patients when “true fixation” of the arytenoid is present. We have found that the fiberoptic scope has use in the assessment of vocal cord mobility in the presence of exophytic supraglottic carcinomas because the tip of the scope can be manipulated past the lesion to look at the structures below. The clinical implication is that careful assessment of the vocal cord and arytenoid mobilities is essential when planning for conservation laryngeal surgery to attempt to understand which deep structures are invaded and which in turn may improve the likelihood of applying the appropriate surgical technique.
Radiologic Evaluation of the Primary Site
Although imaging studies are frequently available before the clinical evaluation of the primary site, the best role of these studies is to corroborate the clinical findings noted on indirect and direct laryngoscopy and to corroborate clinical evidence of deep growth of lesions. This is because although there are specific findings that are particularly useful to assess with imaging studies, there are limitations to the value of these studies, and they may either overpredict or underpredict tumor in certain situations. One caveat is that when evaluating particularly small lesions or the superficial extension of a large lesion, CT87 or MRI may demonstrate little abnormality. This is because these modalities are insensitive to superficial mucosal masses. Another pitfall is seen in those with large exophytic lesions. When lesions have large extensions into the airway, they may sit up against adjacent mucosal sites such as the pyriform sinus, tongue base, floor of mouth, lateral pharyngeal wall, or ventricle or saccule. Although the point of the attachment of the cancer may be small and discrete, the scan may deceptively indicate that all mucosal surfaces are involved. In these patients the endoscopist has a better view of the lesion, and the clinical examination takes precedence over the radiologic evaluation. Valsalva maneuver performed during the CT scan may be useful if these issues cannot be resolved at endoscopy.88 Occasionally, tumors may be isodense (CT) or isointense (MRI) with the surrounding tissues, which at times may overestimate or underestimate the size of the lesion noted on the clinical examination.89 In these patients the radiologist and surgeon should work together to find the true extent of tumor.
Laryngeal imaging studies have been useful in a number of areas. Occasionally, the bulk of the lesion extends submucosally into the subglottis. In these patients, MRI more so than CT can be useful to demonstrate the direct invasion or secondary thickening or asymmetry caused by the lesion in this area. Coronal T1-weighted MRI scans are particularly elegant in demonstrating submucosal transglottic spread. The cricoarytenoid area is best evaluated with axial scans, and sclerotic changes on CT are indications of perichondrial or direct arytenoid cartilage involvement.88,90 Sagittal MRI has been shown to be a sensitive and specific test for varying degrees of preepiglottic space invasion.91 Because the cartilages of the larynx calcify starting in the second decade in an inhomogeneous fashion, loss of calcification of the cartilage on CT is an unreliable indicator of tumor extension.92 MRI has been shown to be highly sensitive to cartilage invasion, particularly if fat-suppressed and postgadolinium scans are performed. Enhancement into cartilage on postgadolinium fat-suppressed scans is highly sensitive to invasion, but it suffers from reduced specificity because inflammation and chondronecrosis will show similar findings. Kirchner93 noted that the most common site of thyroid ala invasion from glottic carcinoma is the lower edge, and questionable isolated involvement of the superior aspect of the thyroid cartilage may represent random calcification patterns within the cartilage. We agree with Kikinis and colleagues94 that MRI has been more useful for evaluating tumor extension into or through laryngeal cartilages. Fluorodeoxyglucose (FDG) PET has gained popularity among physicians in the staging and surveillance of head and neck cancer.95 Its most promising role in larynx cancer appears to be in the delineation of posttreatment effect (medical organ-preservation strategies) from recurrent tumor. The role of FDG PET in organ preservation for the larynx paradigm is currently being assessed in a prospective study.
T Stage
The larynx by convention is divided into three discrete parts for the purpose of T staging. The supraglottis begins inferiorly at the lateral angle of the ventricle. Although the supraglottis extends superiorly up to the tip of the epiglottis, the vallecula mucosa is part of the oropharynx. The glottis begins at the lateral angle of the ventricle, and it extends 1 cm inferiorly at the midcord level. The subglottis begins at the inferior aspect of the glottic level and extends to the inferior aspect of the cricoid cartilage. Although this partitioning of the larynx is somewhat artificial, it allows for a staging system that, despite its shortcomings, allows for comparison of treatment modalities and prognostication.96 Although the T-staging system is useful when comparing modalities that encompass the entire larynx such as radiotherapy or total laryngectomy, it lacks the precision necessary to determine whether conservation laryngeal surgery may be performed at all and, if so, which particular procedure is indicated. Within each of the four T stages, at each site there is a spectrum of lesions for which a variety of conservation laryngeal procedures may be used with successful outcome. When planning for conservation laryngeal surgery, numerous factors that go beyond the level of detail required in the T-staging system should be evaluated. The factors that are clinically important include the precise extent of mucosal involvement, the depth of invasion of the malignancy, and the vocal cord and arytenoid mobilities. Although it has frequently been stated that millimeter margins are adequate for conservation laryngeal surgery, the caveat to this axiom is that for any given conservation laryngeal technique, millimeters of tumor extension within the larynx may preclude performing that technique and may result in intraoperative conversion to total laryngectomy. The conservation laryngeal surgeon should describe the lesion in more detail than the T-staging system to allow for application of the appropriate conservative laryngeal technique.
Overall Clinical Assessment
The degree to which the severity of pulmonary disease is used in the decision to proceed with conservation laryngeal surgery remains controversial in the literature. The real question is how well the patient will tolerate some degree of aspiration during the early postoperative period.97 The amount of postoperative aspiration varies with the type of surgery contemplated. Vertical hemilaryngectomy sparing arytenoid typically causes little impact on swallowing function, whereas extensions of standard or extended supraglottic laryngectomy may result in increased dysphagia and aspiration risk.98 Some authors advocate pulmonary function tests routinely for all patients,99 whereas others use clinical evaluation such as walking up two flights of stairs without getting short of breath.1,97 The percutaneous gastrostomy tube has been useful for patients who require long periods of no nutrition by mouth.100 The literature actually leaves a fair amount of leeway for the clinician in terms of the pulmonary workup and in terms of how to use this information in clinical decision making. We rarely use pulmonary function testing preoperatively, unless requested by a medical consultant or anesthesiologist in preparation for a general anesthetic. If the patient has chronic obstructive lung disease but can walk up two flights of stairs without being winded and is active in his or her daily life, then the risks, benefits, and alternatives of conservation laryngeal surgery are discussed with the patient. If the pulmonary status indicates severe impairment of activity and a likelihood of morbidity or mortality after the procedure, we do not recommend conservation laryngeal surgery for that particular patient. In actual practice, each surgeon should know, over time, the limitations of a particular surgical technique in “their hands.” Using this approach, there rarely will be patients who need functional laryngectomy for intractable aspiration, although there will also be many patients who have had their larynges spared with conservation laryngeal surgery.
An important factor in patient selection is the patient’s insight into the problem and the ability of the patient to play an active role in his or her rehabilitation. The issue of age has been discussed often in the literature. Some authors have strict age criteria for performing partial laryngeal surgery.101 Others have stated that it is the biologic age and the patient’s overall constitution that is more important than the chronologic age.1,100,102 In addition, conservation laryngeal surgery is a “team endeavor,” and if the patient and family prefer to “sit on the sidelines” rather than be actively involved in the rehabilitation process, it is our experience that the patient will likely have a protracted course with increased morbidity. In our institutions, the assessment of the patient’s willingness and ability to be rehabilitated is a joint decision among the speech pathologist, otolaryngologist, patient, and family. Although we do not obtain preoperative modified barium swallow, all patients are assessed by a speech pathologist, and the rehabilitation is discussed with the patient. The sine qua non for a cooperative and functional patient postoperatively is extensive preoperative counseling by the surgeon and speech pathologist. The patient and family should understand that much work is required on their part for rehabilitation. Some patients may choose alternative nonsurgical approaches to their problem or even total laryngectomy to avoid the swallowing rehabilitation required for some conservation laryngeal procedures.
Surgical Techniques
Indications and Contraindications
The indications for particular surgical techniques, presented in the literature, have varied over time. Indications frequently vary, depending on the stage of development of the technique. When a technique is first introduced, most surgeons advocate conservatism in its application.2,9 Later, pioneering surgeons attempt to cautiously extend the use of techniques, frequently on the basis of applications of their surgical skills combined with their knowledge of surgical anatomy and by necessity without the benefit of long-term oncologic follow-up evaluation.103,104 The final stage in the development of a technique, according to Daly,105 is reevaluation followed by acceptance of the technique on the basis of reported results. Before the last stage of development, the indications for a particular technique are usually parochial and based on the anecdotal experiences at a particular institution or the pronouncement of a pundit in the field. Reliance on the literature for indications and contraindications is, therefore, frequently not helpful because surgeons usually attempt to use techniques for a large spectrum of tumor stages. To address this problem, we have provided, for each technique, a thorough literature review in terms of oncologic results, functional outcome, and complications. The surgeon can use this information when advising patients concerning the risks, benefits, and alternatives for a particular surgical procedure.
Conservation Laryngeal Surgery for the Lesions Originating in the Glottic Level
Vertical Partial Laryngectomies
All vertical partial laryngectomies share a common approach, which includes a vertical transection through the thyroid cartilage and paraglottic space. The extent of resection is decided on the basis of the preoperative and intraoperative assessment of the tumor extent. Although this vertical approach provides useful and expeditious access to the endolarynx, they all share a common characteristic, which is “blind” entry into the larynx through a narrow exposure.106 Depending on the extent of the primary lesion, the initial vertical cut may be close to or distant from the cancer. This point should be considered when these procedures are used.
Vertical Hemilaryngectomy
ONCOLOGIC RESULTS
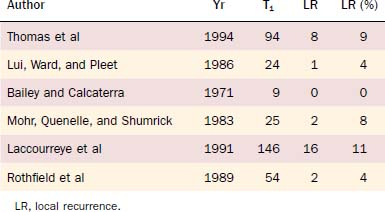
Among the series in the English language literature in which local control has been reported in terms of the T stage, the local recurrence rates for T1 lesions ranged from 0% to 11%, with five of six series having a local control of greater than 90% (Table 110-1). In one large series of 248 patients, the local control was 93% (104 of 112) for patients with malignancy confined to the true cords without anterior commissure involvement.106 In that same series, patients with anterior commissure involvement without impaired mobility or extension beyond the glottis had local failure rate of 25% (8 of 32). When the anterior commissure is involved, the most common site of recurrence is the subglottis, as demonstrated in a series in which 14% (8 of 58) of patients with anterior commissure involvement had vertical hemilaryngectomy failure; in 7 of 8 of these patients, the recurrence was in the subglottis.107 When the anterior commissure is involved by cancer, a wide surgical margin is indicated in the subglottis. Another factor that portends poor local control is extension beyond the confines of the glottis or impaired mobility.
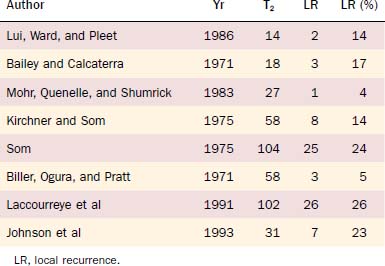
Mohr and others108 reported the highest local control in the literature for T2 glottic carcinoma after extended vertical hemilaryngectomy, but they included only T2 lesions with impaired mobility and excluded lesions that extended beyond the midventricle (only five patients) or beyond 5 mm into the subglottis because of the known high local failure rate for these lesions.108 Subglottic extension has been associated with cricoid cartilage invasion, which is not resected in the standard vertical hemilaryngectomy.109 Extension into the supraglottis through the ventricle should alert one to the possibility of thyroid cartilage invasion, which may account for the higher local recurrence in this patient group.108 The difficulty in managing T2 glottic carcinoma with vertical hemilaryngectomy was noted in a number of series that had local failure greater than 20%,41,106,110 and six of the eight series in the English language literature that correlated local recurrence with T stage reported a local recurrence rate of greater than 14% (Table 110-2). One cause for impaired cord mobility is varying degrees of thyroarytenoid muscle invasion within the paraglottic space, which, in our opinion, may account for the higher local failure rates in vertical hemilaryngectomy in which the paraglottic space is routinely transected.67
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree