 he medial ends of both the superior and the inferior lids contain a punctum. The puncta are situated on a slightly elevated platform, called the “lacrimal papillae,” and face posteriorly, so it is necessary to evert the medial lids to inspect them. The lower punctum is more effective for draining tears.
he medial ends of both the superior and the inferior lids contain a punctum. The puncta are situated on a slightly elevated platform, called the “lacrimal papillae,” and face posteriorly, so it is necessary to evert the medial lids to inspect them. The lower punctum is more effective for draining tears.
Punctual stenosis may be congenital or acquired. Congenital punctal closure may be caused by a membrane on the punctum, or it may be a part of more extensive atresia. The use of local antiviral or antiglaucoma medication or local cicatrizing diseases of the conunctiva may result in obstructions. An infrequent cause of functional closure of the punctum is enlargement of the caruncle that lies between the punctum and the lacus lacrimalis.
A dilator may be used to open a functionally closed punctum with soft elastic walls, but it may close shortly afterward because of the peculiar elasticity of the tissues. Patients with this condition are often frustrated because although syringing is always successful, they continue to suffer from epiphora.
Forcible dilation of the punctum usually fails. Unless some tissue in the mouth and the adjoining wall of the punctum is removed, the condition does not resolve. The treatments available for punctual closure are simple dilation, redilation, and posterior wall punctectomy, in which the vertical limb of the canaliculus is amputated. Because the failure rate is high, many ophthalmologists are reluctant to manage cases of punctal closure.
Treatment of Punctal Atresia
Acquired Punctal Atresia
In cases of functional blockage with no lid abnormality, the management is as outlined below.
TECHNIQUE
Anesthesia
Infiltrate lidocaine 2% near the lid margin and use surface anesthesia.
Surgical Technique
- Insert the dilator into the punctum to confirm its position (Fig. 8.1). When you remove the dilator, the opening closes again, as expected. Syringe the area to confirm that the rest of the passage is clear.
- Insert a medium-sized lacrimal probe into the punctum to reach the ampulla and hold it there.
- Activate a 300-µm Fugo blade tip at the highest energy level and repeatedly touch it to the lacrimal probe at some distance away from the flesh. The tip of the lacrimal probe actually performs the function of the Fugo blade tip every time it is touched, thereby trimming the tissue around the probe.
- When you remove the lacrimal probe, a beautiful round punctum remains.
Figure 8.1. The punctum is hardly visible, but it easily accommodates a medium-size probe. The dilator is passed into the punctum. The probe is inserted into the ampulla. The activated Fugo blade tip touches the probe close to its entry point. A nice punctum is produced at the end of the procedure.
If the condition recurs, it is easy to repeat the treatment.
Postoperative Management
Infiltrate lidocaine 2% near the lid margin and use surface anesthesia.
Congenital Punctal Atresia
In congenital punctal atresia, the punctum may not be visible, or it may be seen vaguely or may appear as a shallow avascular spot or depression. Its presumed location is medial to the meibomian gland orifices. The inferior punctum is temporally displaced relative to the superior punctum, rather than lying directly across from it. The management of congenital atresia is some-what different from that for acquired punctal atresia.
TECHNIQUE
Anesthesia
Infiltrate lidocaine 2% near the lid margin and use surface anesthesia.
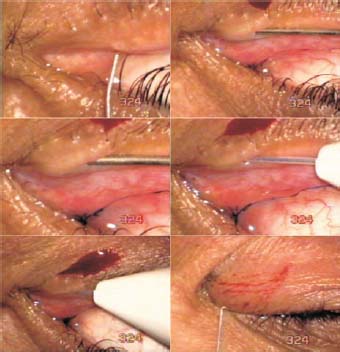
Figure 8.2. The canaliculus is visible as a grey line medial to the punctum. A thin probe encounters the obstruction. A thicker probe is inserted to dilate the canaliculus, through which a 300-µm soft Fugo blade tip is gently pushed up to the obstruction. Activation and movement of the tip in line with the canaliculus instantly clears away the obstruction. A probe is passed through the nasolacrimal duct to complete the operation.
Surgical Technique
- Touch an activated 300-µm Fugo blade tip, set at medium energy and high power, to the supposed or known site of the punctum (Fig. 8.2).
- Touch the tip vertically toward the first vertical section of the canaliculus to a penetration depth of only 0.5 mm.
- Insert a lacrimal probe to determine whether it will negotiate through all of the canaliculus and the nasolacrimal duct. If it does, then pass thicker probes through the canaliculus and the nasolacrimal duct.
- If the newly formed punctum looks reasonably good, nothing remains to be done. The size of the punctum can be increased with the Fugo blade.
Postoperative Management
Prescribe local steroid–antibiotic drops for five to six times a day and steroid–antibiotic ointment at bedtime. Advise the patient to carry out this regimen for 2 weeks.
Treatment of Canaliculus Closure
Opening the Vertical Portion of the Canaliculus
The vertical portion of the canaliculus is about 2 mm long and joins the horizontal canaliculus at a right angle called the “ampulla.” When this part of the canaliculus in involved in scar formation, it is opened in the same way that the punctum is opened.
TECHNIQUE
Anesthesia
Infiltrate lidocaine 2% near the lid margin and use surface anesthesia.
Surgical Technique
- Only the activated tip has to go deeper than a depth of 2 mm. Be very careful not to go through the wall of the canaliculus at the ampulla.
Introduce the unactivated tip into the canaliculus, until it can go no further. Activate it without pressing it. This removes about 0.2 mm of the obstruction. Remove the tip and introduce a probe to see whether the desired depth has been achieved. If it has not, repeat the process until the ampulla is reached. The proof that you have achieved the goal is that the probe can be turned at a right angle and passed into the horizontal segment.
Opening the Horizontal Portion of the Canaliculus
The horizontal canaliculus is about 8 mm long. It usually joins the vertical canaliculus to form the common canaliculus, which immediately enters the nasolacrimal sac through the valve of Rosenmüller (a flap of mucosa to prevent reflux).
A canaliculus can close up as a result of any pathologic condition that produces raw areas on the canalicular wall, which may cause narrowing or obliteration of the lumen. The obliterated length and position varies. Canalicular obstruction can be caused by chlamydial infections (trachoma); viruses such as chickenpox and herpes simplex; bacterial diseases of the lids; or cicatrizing diseases such as ocular pemphigoid. Local medications and radiation can also cause canalicular obstruction, but most canalicular obstructions are idiopathic.
Patients with this condition suffer from intractable epiphora—a condition that is fairly common but often resistant to treatment. A forceful attempt to open the canaliculus with a lacrimal probe at best fails or at worst further damages the canaliculus. What is required is a clean removal of the obstructing epithelial or scar tissue without tearing or puncturing the canaliculus. This can be successfully achieved using the Fugo blade.
TECHNIQUE
Anesthesia
Infiltrate lidocaine 2% near the medial canaliculus.
Surgical Technique
- Verify the obstruction site with a thin lacrimal probe. Then insert increasing sizes of lacrimal probes up to the locus of the obstruction. The idea is to make it easy for the fairly flexible Fugo blade tip to traverse the distance up to the obstruction with the least resistance and without bending.
- Insert a 300-µm straight Fugo blade tip. It has a 200- µm sleeve of nonstick material, which gives the tip a total width of 0.7 mm. About 0.25 mm of the tip is bare. The sleeve ends abruptly and is flat at the end. The 300-µm filament is also flat at the end.
- To reach the site of the obstruction, first pass the 300-µm tip vertically through the first part of the canaliculus and then turn nearly vertically to go through the canaliculus proper. (For right-handed surgeons, tackling the right canaliculus is easier than entering the left one. The opposite is true for the left-handed surgeons.) Stretch the lid straight to make the tip entry easier. The thick cable attached to the Fugo blade handle is rather heavy for the delicate work to be performed; drape the cable over your shoulder to get it out of the way and reduce the drag on the cable.
- Push the Fugo blade tip up to the obstruction site. It is important at this stage that the stretching and straightening of the canaliculus and the ablating tip and the handle of the instrument are correctly aligned because the tip will be activated and pushed simultaneously. Set the tip at medium power at high energy. The tip goes through the obstruction in a fraction of a second; push it all the way in until it strikes the bone.
- Insert lacrimal probes of increasing sizes to ensure that the canaliculus is open and well dilated. Then pass a probe through the nasolacrimal duct, pressing through any obstruction that may be present. This procedure works if the canalicular wall is intact. As the tip ablates the obstructing tissue, the nonstick sleeve keeps the canalicular wall away, thus preventing perforation of the duct. Sometimes, as a result of pathology, previous failed attempts, or both, the canalicular walls may become an inseparable part of the scar tissue. In such cases, making or opening the canaliculus can be a guessing game, but usually in this cases a track will form through which a lacrimal probe can be passed, making the operation likely to be a success.
A successfully opened canaliculus may close again. It may happen days, weeks, or months after surgery, but it can be reopened with little or no problem.
Summary
Canalicular blockage is a common condition. A closed canaliculus is a great concern for the patient because of the continued tearing, and it is a difficult condition for the surgeon. A forceful mechanical attempt to open a recalcitrant canaliculus can only aggravate the condition. But we have successfully treated over 100 cases of canalicular blockage with Fugo blade.
Suggested Reading
Nasolacrimal duct, obstruction. Accessed January 3, 2010, at http://emedicine.medscape.com/article/1210141-overview.
Nasolacrimal duct, congenital anomalies. Accessed January 3, 2010, at http://emedicine.medscape.com/article/1210252- overview.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



