Fig. 8.1
Orbital cellulitis . Contrast CT (a) axial (b) coronal. Black arrow demonstrating fat stranding and edema involving the medial and inferior recti muscle on the right with no abscess collection
Specimen Collection
Nasal swabs are unreliable for identifying a pathogen associated with sinusitis, as bacteria that colonize the respiratory tract may not be the causative agent of a suppurative infection [1, 11].
Studies that have utilized proper methods for recovery of anaerobes have identified these pathogens in an overwhelming majority of abscesses [12]. In one study, 90 % of intracranial abscess cultures revealed anaerobes [12]. Lack of proper technique in collecting and/or processing anaerobic cultures is felt to be responsible for the poor yield observed in many operative cultures [13]. In order to maximize recovery, it is imperative that if collected in a syringe the sample is immediately sealed or is transported in anaerobic media and that samples are promptly delivered to the microbiology laboratory [14].
Medical Management of Extracranial Complications
Empiric therapy for orbital infections must include drugs with activity against the expected pathogens including Streptococci, Staphylococcus aureus, oral-gram negatives, and oral anaerobes. Local patterns with regard to the frequency of methicillin-resistant Staphylococcus aureus infections should be considered. Commonly used antibiotics with activity against Streptococcal species and oral-gram negatives include ampicillin-sulbactam and third-generation cephalosporins. Clindamycin and vancomycin have activity against methicillin-resistant Staphylococcus. Ampicillin-sulbactam and clindamycin provide good coverage of oral anaerobes whereas vancomycin is only active against gram-positive anaerobes. If MRSA is not suspected, monotherapy with ampicillin-sulbactam can be considered [14].
A retrospective review of cases of sinogenic orbital infections from a large tertiary pediatric hospital noted that the mean parenteral and total duration of antibiotics was 12 and 24 days, respectively [15]. Abscesses that have not required surgical intervention may warrant longer parenteral therapy. In patients with normal visual acuity, some providers may elect to initiate treatment with IV antibiotics for 24–48 h prior to obtaining imaging. Imaging is then obtained if there is no improvement of signs and symptoms [16].
Surgical Management of Extracranial Complications
Preseptal cellulitis is caused by sinusitis in 15 % of cases [10]. Other causes of preseptal cellulitis are localized skin infection, local trauma, insect bites, animal bites, foreign bodies, or acute dacryocystitis. Classic physical exam findings demonstrate eyelid swelling and erythema with normal eye movement and no evidence of chemosis. Imaging is not initially necessary for patients demonstrating classic physical exam findings, but may be necessary for patient failing to improve after 24–48 h of treatment. Children older than 1 year with mild preseptal cellulitis and no signs of toxicity may be treated as outpatient with close follow-up. Other patients should be treated as inpatient with IV antibiotics. If there is concern that sinusitis is the causative mechanism, treatment also may include nasal decongestant, i.e., oxymetazoline, nasal steroids, and nasal saline.
Patients with postseptal infection typically present with fever. In one study, 94 % of patients with postseptal infections vs. 47 % of patients with preseptal infections demonstrated a fever [9]. Postseptal infections are preceded by sinus disease in 90 % of cases. Patients with a suspected postseptal infection should have an ophthalmology and otolaryngology consultation.
Patients with orbital cellulitis may have ophthalmoplegia, pain with eye movement or diplopia (Fig. 8.1). They will have periorbital erythema, edema and chemosis. An ophthalmology consult is warranted to assess for changes in visual acuity and intraocular pressure. Imaging in these cases is a debated topic as the goal of imaging is to identify a drainable abscess [17]. Provided that there is no compromise in visual acuity, some clinicians elect to initiate treatment with IV antibiotics for 24–48 h prior to obtaining imaging. The imaging modality commonly obtained is contrasted CT scan of the sinuses, although MRI may be considered particularly if there is concern for intracranial involvement. Imaging followed by surgery should be performed urgently if decreased vision is a concern. Treatment for uncomplicated orbital cellulitis consists of IV antibiotics, nasal decongestant, nasal steroid, and nasal saline.
Signs and symptoms of subperiosteal abscess are similar to orbital cellulitis except patients with a subperiosteal abscess may have proptosis and inhibition of extraocular movement (Fig. 8.2). Patients may complain of diplopia, but visual acuity is typically normal. If visual acuity is normal, treatment may be initiated prior to imaging and imaging obtained if improvement is not observed in 24–48 h or if symptoms worsen. Subperiosteal abscesses along the medial wall, <1 cm in width, and in patients younger than 9 years of age have a higher likelihood of responding to medical management alone [18–21]. Surgical approaches can be external, endoscopic, or combined. Most medial or inferior wall abscesses are amendable to drainage via a transnasal endoscopic approach. Lateral or superior abscess require an external approach [22].
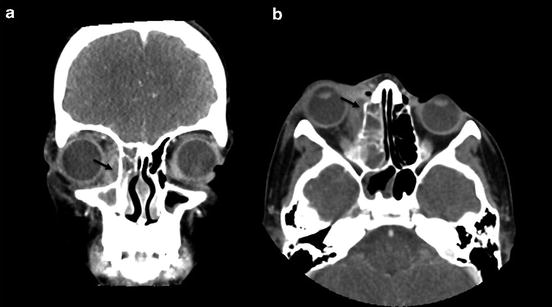
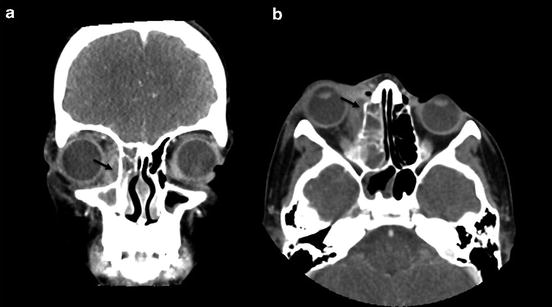
Fig. 8.2
Subperiosteal abscess . Contrast CT scan (a) coronal (b) axial. Black arrow shows evidence of peripherally enhancing small subperiosteal abscess collection in the extra-conal space of the right orbit with moderate surrounding edema and mass effect on the adjacent medial rectus muscle. There is fluid opacification in the right ethmoid and maxillary sinuses
Patients with an orbital abscess typically exhibit the same signs as orbital cellulitis plus proptosis and visual acuity changes. Imaging should be obtained in patients with a suspected orbital abscess. Treatment consists of IV antibiotics and in most institutions an oculoplastic surgery consult for drainage of the abscess through an external approach.
Cavernous sinus thrombosis is a life threatening condition (Fig. 8.3). It should be suspected if the contralateral eye is also affected. Signs and symptoms which may be observed are ptosis (CNIII), extraocular eye movement impairment (CNIII, IV, VI), numbness of forehead or midface (CNV1 and V2), headache, and loss of vision (CNII). Magnetic resonance venography should be obtained. Treatment consists of IV antibiotics. Anticoagulation may be used with the aim to inhibit propagation of the thrombus and promote recanalization of the sinus.
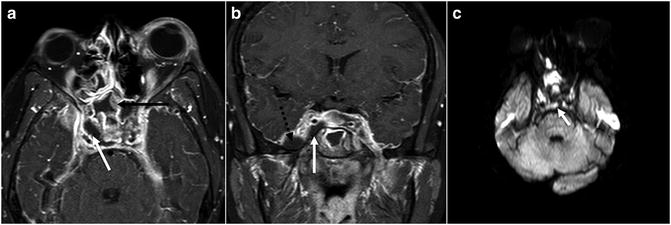
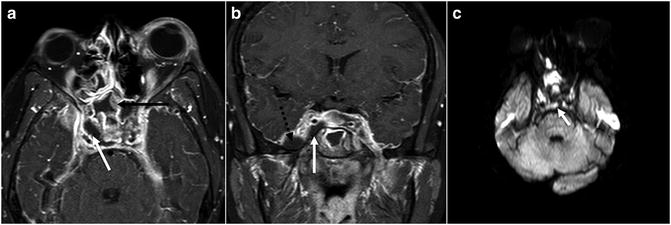
Fig. 8.3
Cavernous sinus thrombosis . (a) MRI contrast axial T1 (b) MRI contrast coronal T1 (c) MR axial DWI. There is evidence of complicated sphenoiditis with right subtemporal epidural abscess and associated right cavernous sinus thrombosis. Note of decreased enhancement in the right cavernous sinus when compared to the contralateral side. Evidence of restricted diffusion is noted in the involved sphenoid sinus and cavernous sinus. Black arrow shows marked sphenoiditis; white arrow shows right cavernous sinus thrombosis with decreased enhancement; dashed black arrow shows peripherally enhancing epidural abscess in the right sub-temporal region with accompanying dural enhancement
Pott’s Puffy Tumor
Pott’s puffy tumor is osteomyelitis/subperiosteal abscess of the frontal bone from frontal sinusitis (Fig. 8.4). Patients present with forehead or scalp swelling and tenderness over the forehead. Treatment involves aspiration and/or drainage of forehead abscess and treatment of the sinusitis. Management of the underlying frontal sinusitis should be with IV antibiotics +/− surgical drainage of the frontal sinus. Surgical drainage may be achieved by an external approach (trephination), combined external and endoscopic approach, or endoscopic approach [23].
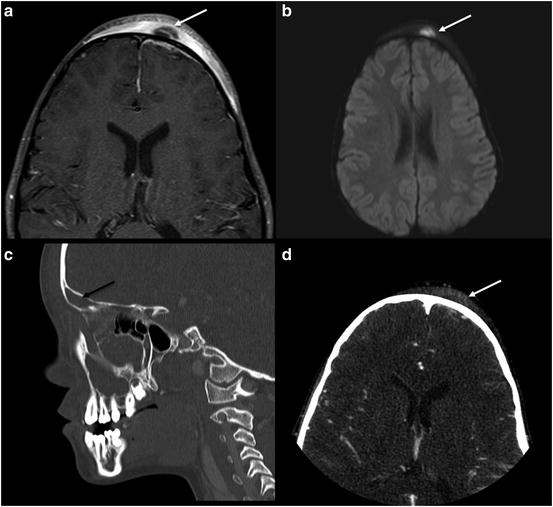
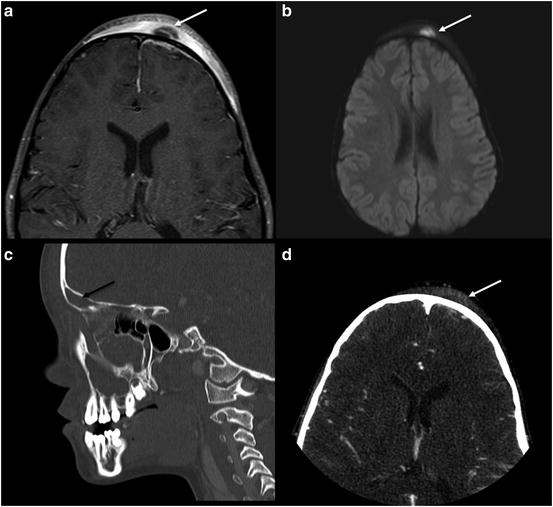
Fig. 8.4
Pott’s Puffy Tumor . (a) MRI post axial T1 (b) MRI axial DWI (c) contrast CT sagittal (d) contrast CT axial. There is peripherally enhancing subperiosteal abscess in the left anterior frontal area with marked adjacent scalp edema. There is associated dural thickening and enhancement in the left frontal convexity and interhemispheric fissure. White arrow shows restricted diffusion in the abscess. Black arrow shows acute frontal sinusitis with complete fluid opacification
Intracranial Complications
Pathophysiology of Intracranial Complications
The frontal sinuses are most commonly associated with intracranial complications, followed by the ethmoid, sphenoid and maxillary sinuses. Intracranial spread of infections is believed to occur mainly by progression of septic thrombi through the valveless diploic veins of the skull base that penetrate dura [24]. Less commonly, it can occur via direct extension of osteomyelitis of the bony sinus walls or via penetration through existing bony defects (e.g., congenital or posttraumatic) [5]. The frontal skull is particularly vulnerable to spread of infection, likely because of its rich network of diploic veins. It has been postulated that the rapid growth of the frontal sinuses and their blood supply account for the high association of intracranial complications in adolescent males [25]. Intraparenchymal brain abscesses are seeded by the hematogenous route, and therefore, can be found in all regions of the brain.
Classification of Intracranial Complications
Intracranial complications of sinusitis are less common than orbital infections, but may lead to significant morbidity and mortality. The incidence of intracranial complications has been reported to be 3–17 % [26–28]. They include meningitis, epidural or subdural empyema and abscess, venous sinus thrombosis and intraparenchymal abscesses. Subdural empyema is the most common intracranial complication, comprising 33–85 % of all intracranial complications of sinusitis [29]. Sinus infection may progress to intracranial infection despite adequate IV antibiotic therapy. Maintaining a high index of suspicion is key in the prevention of potential lifelong disability. Intracranial complications should be suspected in a patient who presents with fevers, severe headache, photophobia, seizures, or other focal neurologic findings. Rhinorrhea and nasal congestion are not always observed. Diagnostic evaluations often include imaging studies such as CT and MRI. CT has the superior ability to demonstrate bony detail and anatomy, which are critical in guiding Endoscopic Sinus Surgery. MRI is obtained when intracranial extension is suspected, due to its ability to discriminate brain and meningeal inflammation as well as fluid collections [30]. Examples of an epidural abscess and subdural abscess are shown in Figs. 8.5 and 8.6, respectively.
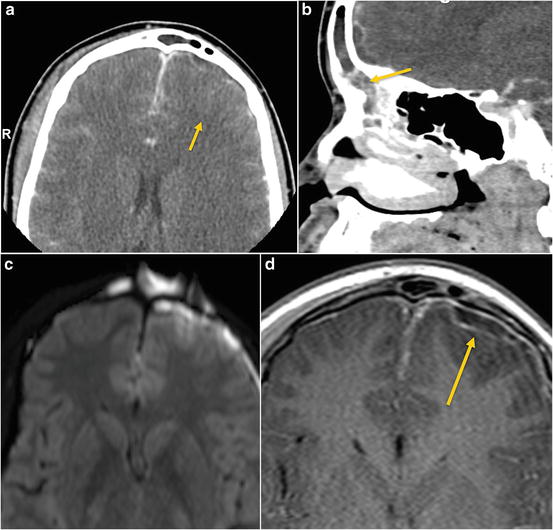
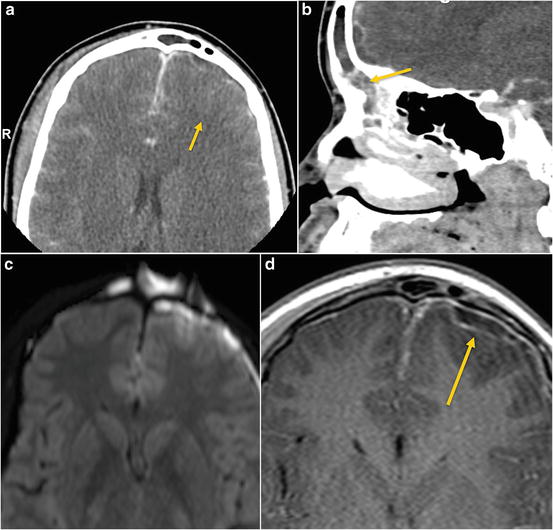
Fig. 8.5




Subdural empyema . (a) Axial and (b) sagittal post contrast CT images show a peripherally enhancing subdural empyema in the left anterior frontal convexity secondary to complicated acute sinusitis from the frontal sinus. (c) Axial MRI diffusion (DWI) sequence and (d) post-axial T1 showing left frontal subdural empyema and anterior frontal lobe cerebritis secondary to frontal sinus abscess with restricted diffusion. Restricted diffusion is also noted in the abscess. There is associated dural thickening and enhancement in the contralateral frontal convexity and interhemispheric fissure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


