Chapter 129 Cavernous Hemangioma
Clinical findings
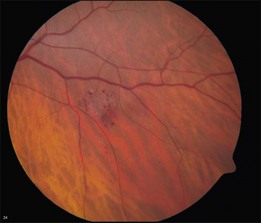
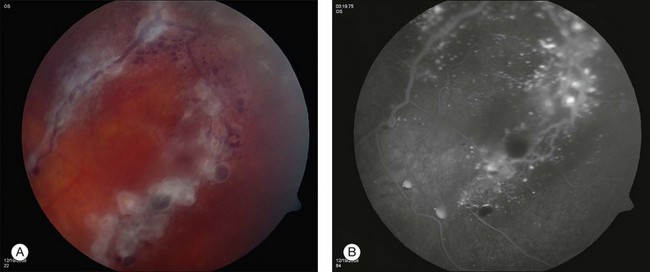
Retinal cavernous hemangiomas are composed of clusters of saccular aneurysms filled with dark blood. There is no intervening retinal tissue between the aneurysms. The aneurysms range in size from microaneurysms to a half-disc diameter.1 The typical tumor is isolated, one to two disc diameters in size, and resembles an intraretinal cluster of grapes (Fig. 129.1, see also Fig. 129.3).2,3 However, the clinical appearance can be quite variable; ranging from a single aneurysm to a wide distribution over the entire fundus or following the course of a major vein (see Fig. 129.5). Commonly, layering of the red blood cells within the aneurysms causes a plasma–erythrocytic separation that has been called a “pseudohypopyon.” Often a white or gray fibroglial membrane covers the surface of the tumor (see Fig. 129.5A). The adjacent retinal blood vessels appear unaffected by the tumor, with no evidence of feeder vessels. Although a mild lipid exudate has been reported adjacent to the hemangioma in one case,4 exudation from the tumor is extremely rare either at presentation or with long-term follow-up. The slow circulation through the aneurysms is responsible for the lack of exudation of lipid or fluid.
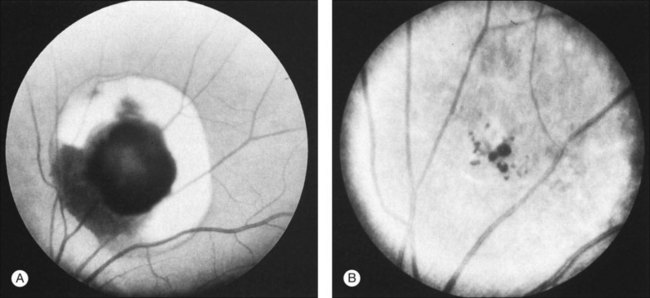
Retinal cavernous hemangiomas are symptomatic when they are located in or adjacent to the macula which has been reported in approximately 10% of the cases in the literature.1,5,6 In these cases, visual acuity can be decreased on the basis of both tumor location and amblyopia. Visual disturbance can also result from vitreous hemorrhage. Cavernous hemangioma can cause simultaneous subretinal, intraretinal, and preretinal hemorrhage (Fig. 129.2). Although vitreous hemorrhage has been reported in 10% of retinal cavernous hemangiomas, it is usually old, minimal, and unassociated with long-term loss of visual acuity.1 However, vitreous hemorrhage, if it occurs in a child, may cause amblyopia.7
Cavernous hemangiomas have also been reported to be located on the optic nerve head.8–10 These tumors have a clinical appearance similar to the retinal lesions (Fig. 129.3). An enlarged blind spot may be demonstrated on the visual field, but visual acuity is normal. Gündüz et al.11 described a patient with a cavernous hemangioma in the superonasal quadrant of the fundus and unilateral decreased visual acuity, with associated red–green color defect. Cone response and 30 Hz flicker responses were nearly absent.
Differential diagnosis
The characteristic appearance of a retinal cavernous hemangioma is rarely confused with other conditions. Retinal telangiectasis can have a similar appearance, and several authors have suggested that older cases of cavernous hemangioma were mistakenly called Coats disease or Leber miliary aneurysms.3,8,12 The lack of intraretinal exudate distinguishes this tumor from Coats disease, but the differentiation from Leber can be more difficult. Gass points out that the retinal telangiectasis of Leber is a progressive condition affecting the integrity and structure of the “intrinsic” vasculature, whereas the cavernous hemangioma is a sessile tumor projecting from and partly isolated from the retinal blood vessels.8 On the other hand, Giuffre13 reported a case with a cavernous hemangioma and retinal telangiectasis closely located in the same eye, suggesting a relation between these two developmental conditions. Telangiectatic or microaneurysmal vascular dilation can also be seen as late sequelae in branch vein occlusions and diabetic retinopathy but should be easily differentiated from retinal cavernous hemangioma by the associated features.
Ancillary studies
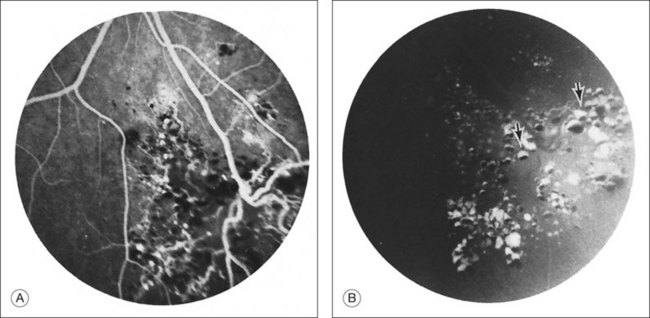
Fluorescein angiography may show autofluorescence of the gray-white epiretinal membrane overlying the tumor. The aneurysms will fill slowly and often incompletely up to 30 minutes after dye injection. Dye will rarely extravasate from the tumor in the late phase of the angiogram. In addition, the plasma–erythrocytic separation often seen on clinical examination is dramatically demonstrated in the later phases of the angiogram. The fluorescein collects in the superior portion of the aneurysm, with the gravitated blood cells blocking its accumulation in the inferior area (Figs 129.4 and 129.5B).
Although performing echography is rarely necessary, the ultrasonographic features have been described by Shields3 in cases in which diagnosis was rendered difficult by vitreous hemorrhage. A-scan shows a high initial spike and high internal reflectivity. B-scan shows an irregular surface, large internal acoustic density, and absence of choroidal excavation. Many cavernous hemangiomas are too small to exhibit a characteristic echographic pattern.
Natural history
Growth of a retinal cavernous hemangioma is exceedingly rare. Klein et al.4 reported the only case of enlargement, and this developed after photocoagulation. Messmer et al.1 noted enlargement of the fibroglial component, which may represent progressive thrombosis of some of the aneurysms. In a later report, Kushner et al.14 monitored two patients over 5–10 years and reported definitive growth.
Visual loss can occur from growth of an associated epiretinal membrane. In addition, macular pucker has been reported separate from the membrane overlying the hemangioma; the membrane and the tumor in this case were probably unrelated.1 Vitreoretinal or vitreopapillary traction may occur occasionally.15
Vitreous hemorrhage is the most common cause of progressive visual disturbance in patients with cavernous hemangioma. Although usually mild due to slow blood flow through the hemangioma, isolated cases of severe hemorrhage have been reported.16–18 Impairment of visual acuity from vitreous hemorrhage is a very uncommon event.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree