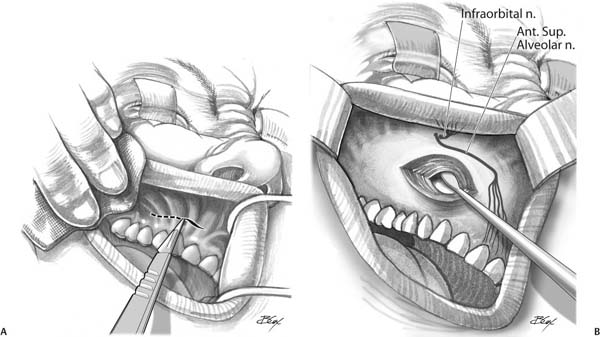
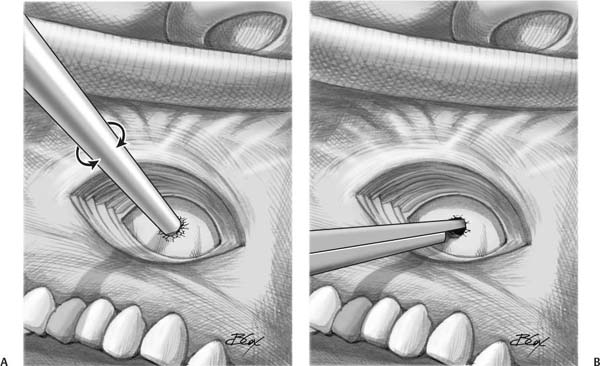
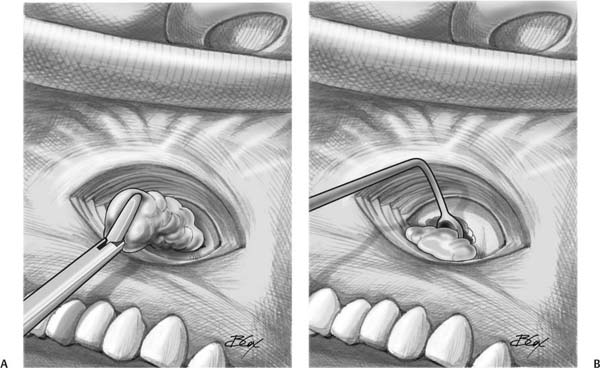
17 Caldwell–Luc Surgery Before the advent of Caldwell–Luc surgery in the 1890s, maxillary sinus disease had been treated by antral washout through the alveolus after removal of a tooth, as described, for example, by William Cowper in 1707. Others described opening the sinus into the nasal passage; however, poor lighting and an incomplete understanding of the sinonasal anatomy led to failures and a decline in popularity of that method. A canine fossa approach to antral washout was used by Desault and Lamorier in the late 18th century. This same approach was advocated by Jansen in the late 19th century; however, he also described packing the sinus to stimulate granulation tissue formation. Still others—notably Lothrop, Claoue, Mikulicz, and Canfield—popularized the inferior meatal antrostomy for surgical management of maxillary sinus infection. In the last decade of the 19th century, three surgeons working independently—George Caldwell of the USA, Scanes Spicer of England, and Henri Luc of France—described creation of an anterior antral window for surgical extirpation of diseased sinus mucosa, to be used in conjunction with an inferior meatal antrostomy. Caldwell–Luc surgery, as it became known, was the primary workhorse for maxillary sinus disease until the 1920s, when intranasal procedures gained in popularity. With the introduction of the nasal endoscope and the advent of functional endoscopic sinus surgery (FESS) in the 1980s, Caldwell–Luc surgery was pushed even further into the background, and today it is utilized only in patients with tumors, masses, or persistent maxillary sinus disease after other medical and surgical therapies have failed. Clarification should be made of some basic terminology. In the canine fossa puncture (described in detail in Chapter 12 of this book) the maxillary sinus is entered through a sublabial, anterior approach placed in a location designed to minimize complication and morbidity. The location of this puncture—traditionally just lateral to the canine fossa—is intended to minimize trauma to the branches of the infraorbital nerve and the anterior superior alveolar nerve that innervate this area. Endoscopes, powered instruments, and other tools may be placed through what is typically a 4 to 5 mm opening. In the Caldwell–Luc approach, this opening is enlarged with cutting instruments (typically Kerrison rongeurs) for improved anterior access to the maxillary sinus. In the Caldwell–Luc procedure (also known as transbuccal radical antrostomy), the maxillary sinus mucosal lining is removed—typically via a Caldwell–Luc approach—and a gravity drainage port is created with an inferior meatal antrostomy. Morbidity from the Caldwell–Luc approach and procedure can be significant and long-lasting. It is for this reason that appropriate indications should be adhered to when considering Caldwell–Luc. Mucosal preserving techniques should always be tried prior to any attempt at mucosal extirpation. Advances in endoscopy and endonasal instrumentation designed specifically to reach into the recesses of the maxillary sinus have led to significantly increased possibilities via endoscopic endonasal approaches, and these less traumatic approaches should be given first consideration. On the other hand, tumors, foreign bodies, and fungal disease, or cases where extended access to the pterygopalatine fossa is required, are some instances where a Caldwell–Luc approach via anterior antral window is appropriate. Others have used this approach in the surgical repair of facial trauma, including orbital floor fractures. The Caldwell–Luc procedure, involving mucosal extirpation, may be considered for cases of persistent maxillary sinusitis in the context of failed aggressive medical and surgical interventions, or in cases of tumor removal. Common anatomic reasons for surgical failure such as missed natural ostium sequence, recirculation, and retained uncinate process must be ruled out prior to performance of a Caldwell–Luc procedure for chronic rhinosinusitis. The Caldwell–Luc approach begins with a gingivolabial incision in the mucosa superior to the canine tooth. This incision is carried laterally to the level of the first molar with care to maintain enough vertical height on the inferior mucosal cuff for adequate tension-free wound closure at the end of the procedure. The incision is made through the periosteum and wide subperiosteal elevation is performed widely over the face of the maxilla. Elevation is carried superiorly to the level of the infraorbital nerve. Attention should be paid to the infraorbital nerve and the anterior superior alveolar nerve. The nerves are protected while the sinus is entered through the anterior wall (Fig. 17.1). Fig. 17.1 (A,B) An incision has been made through the upper lip mucosa and down through the periosteum to expose the face of the antrum. Retractors are placed for increased exposure while a periosteal elevator is used to increase exposure over the face of the maxilla. Elevation is carried superiorly to the level of the infraorbital nerve. Fig. 17.2 (A) A small opening into the antrum is made using a trocar. Placement is performed in a location just superolateral to the canine fossa. (B) After opening into the maxillary sinus, the opening is enlarged using a Kerrison punch. The transantral opening is placed in a location just superolateral to the canine fossa to minimize trauma to branches of the infraorbital and anterior superior alveolar nerves. (Details of precise canine fossa placement are described in Chapter 12.) Various methods have been described to perform the anterior antrostomy. Traditionally, the opening has been created via a small puncture with a trocar aimed medially, followed by a Kerrison punch to enlarge the opening (Fig. 17.2). Others have supported the use of a high-speed drill as a less traumatic and more precise method of entering the sinus. After entrance into the sinus, the contents are removed with grasping instruments. The sinus mucosa is then elevated and removed with curved Coakley curettes and grasping forceps (Fig. 17.3). An inferior meatus antrostomy is frequently performed to allow for nonphysiologic, gravitational drainage. In cases where an intranasal maxillary antrostomy has not previously been performed, one is created with standard endoscopic endonasal techniques. The anterior maxillary wall is left open, and the incision is closed in layers with absorbable suture (see Video 17.1). In some situations where a Caldwell–Luc procedure is appropriate, we have begun to use a modified version, the endoscopic endonasal Caldwell–Luc procedure, which is performed in the following fashion. After endoscopic endonasal resection of the middle turbinate, a large maxillary antrostomy is created using traditional endoscopic techniques. Resection of the medial maxillary sinus wall is continued posteriorly to the junction of the medial and posterior sinus walls with the use of through-biting forceps and the powered instrumentation. Next, using a 70-degree endoscope in combination with angled forceps, meticulous removal of the mucosa from the posterior maxillary sinus wall is performed. Mucosal stripping is continued anteriorly with removal from the lateral, superior, and inferior maxillary sinus walls. Appropriate care is taken to avoid injury to the infraorbital nerve when working along the sinus roof. Frontal sinus instruments are used for optimal access to the mucosa of the lateral maxillary sinus wall. More recently, adjustable angled forceps have been introduced that can be used for this purpose. When the limit of anterior visualization is reached using the 70-degree endoscope, change to the 120-degree endoscope is made, allowing full visualization of the anterior maxillary sinus wall. It should be emphasized that with this approach the entire inner surface of the maxillary sinus can be visualized. Utilizing the 120-degree endoscope in this manner can be a significant technical challenge, and practice in a cadaver laboratory is recommended prior to use on a patient. Complete removal of the diseased mucosa is continued along the anterior wall using angled Coakley curettes until all bony maxillary sinus walls are exposed. An angled-tip burr may then be used to drill down any remaining bony abnormalities (see Video 17.2). Fig. 17.3 (A,B) After entrance into the sinus, the contents are removed with grasping instruments. The sinus mucosa is then elevated and removed with curved Coakley curettes and grasping forceps. Frequent postoperative visits are vital to good results after Caldwell–Luc surgery. Because of the mucosal extirpation, frequent debridements are required in the early weeks to fully remove the blood and scabs, which are the products of surgery. Postoperative discomfort generally limits the amount of debridement that is possible with each visit, and extended visits may be required. In our experience, postoperative care will either lead to remucosalization or to scarring of the sinus. In fact, scarring may be preferable because it functions as a means of sinus auto-obliteration. Compared with FESS, Caldwell–Luc surgery is associated with significantly more patient morbidity. It is for this reason that endoscopic, mucosal preserving approaches should always be preferred—when possible—to Caldwell–Luc surgery. Unlike the typical recovery time of several weeks after FESS, patients should be forewarned that healing from an external Caldwell–Luc procedure may take several months. Complications encountered with Caldwell–Luc include facial edema and pain, bleeding and hematoma, numbness in the infraorbital and anterior superior alveolar nerve distributions, dacryocystitis and persistent epiphora, devitalized teeth, and oroantral fistulae. Facial hypoesthesia is particularly common and its impact on patient quality of life should not be underestimated. Some of these symptoms may be encountered by upwards of 20% of patients. Mucoceles have been noted to occur many years after the initial surgery. More serious, though extremely rare, complications include inadvertent entrance into the orbit and damage to the ocular contents. It is likely that the endoscopic endonasal Caldwell–Luc procedure has significantly less morbidity than the conventional external approach; however, at this point in time there is not enough data to prove this statement. Caldwell–Luc surgery should be a last resort for patients with chronic rhinosinusitis. Only when patients have failed aggressive medical and mucosa-preserving surgical intervention should Caldwell–Luc surgery be considered as a treatment option. When these guidelines are followed, the Caldwell–Luc approach and procedure has been shown to have success rates exceeding 90%. However, some patients have persistent disease after Caldwell–Luc surgery. Treatment of recalcitrant sinus disease in these patients is difficult, but several options are available. First, it must be recognized—and patients must be forewarned—that unlike FESS, recovery after Caldwell–Luc surgery may take months, not weeks. For this reason, early reintervention is discouraged. In some patients, however, symptoms may persist or recur years after surgery. Evaluation should involve careful examination of the sublabial area as well as the sinus with 30- and 70-degree endoscopes. Scars in the sublabial area should be palpated and examined for tenderness and discomfort. All corners of the sinus itself should be visualized endonasally in search of inflamed mucosa, necrotic debris, or pockets of infection. Dedicated sinus computed tomography (CT) is imperative to look for the presence of abscesses, which may have formed within the sinus itself—trapped in the scar tissue filling the sinus. It should be recognized that patients who have had Caldwell–Luc surgery may get sinus infections once or twice per year, like every other patient with chronic rhinosinusitis. Because of the poor mucosal function, these infections may persist longer than usual, and in addition to standard medical treatment, they may require in-office debridements. In patients who fail medical treatment, revision surgery may be indicated. Some have advocated revision endoscopic mucosal-sparing surgery such as creation of a “mega-antrostomy” (removal of posterior-inferior turbinate with endoscopic medial maxillectomy) in these cases. Others support a revision Caldwell–Luc procedure for cases of failed Caldwell–Luc procedures. Either approach may be appropriate. The treatment, however, must be tailored to the disease: a focal abscess or loculated pocket of mucous must be marsupialized and will not respond to a “mucosal-preserving” surgery. The continued use of Caldwell–Luc surgery sparks a great deal of controversy in the otolaryngology–head and neck surgery community. Although most agree that Caldwell–Luc is reserved as a final effort for patients who have failed traditional surgery and whose disease is incompletely accessible to endoscopic approaches, some argue that it simply should never be used at all. Formal evaluation of the efficacy and complications of the Caldwell–Luc approach and procedure are uncommon, but some studies have been done. In one study from 1997, 150 patients were randomized to FESS or Caldwell–Luc surgery. At 7-year follow-up, 20% of the FESS patients had undergone revision surgery compared with 18% of the Caldwell–Luc patients.1 Another study from 1997 found a revision surgery rate of 18% in FESS patients versus 5% in the Caldwell–Luc group.2 More recently, a 5-year retrospective study showed a 92% success rate after an average 2-year follow-up on 37 patients who underwent 50 Caldwell–Luc procedures.3 These studies and others suggest that, when used appropriately, the Caldwell–Luc procedure can lead to positive outcomes. Several authors have suggested an intermediate procedure for use in surgery of the severely diseased maxillary sinus. The canine fossa puncture as a means to remove diseased mucosa (while sparing the mucosal base) has been used with some success. A 2005 study by Wormald evaluated 42 severely diseased maxillary sinuses and found improved symptom control in patients who underwent combined maxillary antrostomy and mucosal clearance via canine fossa puncture versus those who had maxillary antrostomy alone.4 A 2008 study found similarly superior results when comparing mega-antrostomy with mucosal clearance via canine fossa puncture to maxillary antrostomy alone in patients with severely diseased maxillary sinuses.5 These results have been challenged by a 2008 study that found no advantage to canine fossa puncture and mucosal clearance when comparing 13 patients who underwent standard middle meatal antrostomy to 11 patients who underwent antrostomy with mucosal clearance via the canine fossa approach.6 It is, however, well known that Caldwell–Luc surgery has a high rate of complication and patient morbidity, and for this reason should be used only as a last resort. A 1988 review of 670 patients who underwent Caldwell–Luc surgery at a single institution found a 19% complication rate.7 Facial numbness continues to be among the most common of these complications. Cadaver studies by Wormald and others have elucidated the distribution patterns of the infraorbital nerve and anterior-superior alveolar nerve that lead to these sensory deficits when traumatized.8 In fact, the simple canine fossa puncture—theoretically less invasive than a Caldwell–Luc approach or procedure—has been noted to have a long-term incidence of postoperative facial numbness that approaches 10%.9 These studies highlight the lack of strong evidence-based medicine that could determine the decision over when to use a Caldwell–Luc approach or procedure or some modification thereof. Future studies will be needed to bring clarity and certainty to this decision. In the meantime, innovation will likely lead to other hybrid approaches such as the canine fossa puncture and the endoscopic endonasal Caldwell–Luc procedure. • The Caldwell–Luc approach provides access to the maxillary sinus via the anterior face of the maxilla. • The Caldwell–Luc procedure involves exenteration of the maxillary sinus mucosa, traditionally through a Caldwell–Luc approach. • The Caldwell–Luc procedure is a procedure of last resort, appropriate in the treatment of sinusitis for patients who have failed aggressive medical and surgical therapy. • The Caldwell–Luc approach and procedure have significant associated morbidity and should be reserved for patients who have not responded to prior surgical intervention. • When used in this manner, Caldwell–Luc surgery has been found to have good outcomes. • Morbidity to facial sensation may be minimized by paying careful attention to the typical distribution patterns of the infraorbital nerve and anterior superior alveolar nerve. • Hybrid approaches—maxillary antrostomy with canine fossa puncture and the endoscopic endonasal Caldwell–Luc procedure—have recently been described and may decrease morbidity without compromising efficacy.
 The Caldwell–Luc Approach and the Caldwell–Luc Procedure
The Caldwell–Luc Approach and the Caldwell–Luc Procedure
 Indications for Caldwell–Luc Surgery
Indications for Caldwell–Luc Surgery
 Surgical Technique of the Caldwell–Luc Approach and Procedure
Surgical Technique of the Caldwell–Luc Approach and Procedure
 Surgical Technique of the Endoscopic Endonasal Caldwell–Luc Procedure
Surgical Technique of the Endoscopic Endonasal Caldwell–Luc Procedure
 Postoperative Care
Postoperative Care
 Complications of Caldwell–Luc Surgery
Complications of Caldwell–Luc Surgery
 Management Options after Failed Caldwell–Luc Surgery for Chronic Rhinosinusitis
Management Options after Failed Caldwell–Luc Surgery for Chronic Rhinosinusitis
 Evidence-based Review of Caldwell–Luc Surgery
Evidence-based Review of Caldwell–Luc Surgery
Caldwell–Luc Surgery
Pearls
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree