Anesthesia for Eye Surgery
Scott Greenbaum
HISTORICAL PERSPECTIVES
The history of anesthesia for eye surgery dates back 2,500 years. The earliest authentic writings on the subject were those of Sus’ruta, the ancient Indian surgeon who first described couching—the depression of the cataract into the vitreous—around 600 BC.1 He outlined the use of inhalational anesthesia for this method, and also described aseptic technique. Later, Egyptian and Assyrian surgeons used carotid compression to produce transient cerebral ischemia, under which couching was performed. A Spanish alchemist in the thirteenth century described a mixture of sulfuric acid and alcohol, which he called “sweet vitriol”2; in 1730, this substance was renamed either. Faraday reported on its accidentally discovered anesthetic effect in 1818. The use of other general anesthetic agents, such as carbonic acid gas, chloroform, and nitrous oxide was described in the late eighteenth and the nineteenth centuries.1
The eighteenth century was also a time of discovery for more modern techniques of cataract surgery. In 1748, Daviel published a report describing a corneal incision that started at the inferior limbus and continued nasally and temporally for approximately 240 degrees. He next performed an anterior capsulotomy and delivered the lens with a curette or spatula, depending on its density; therefore this, the first planned cataract extraction, was done in an extracapsular fashion.3 In 1753, Samuel Sharp described a planned intracapsular extraction, using a single knife to make the corneal section. It took more than a century for these techniques to become standard practice, during which time couching procedures continued to be performed using soporific drugs and psychological control of the patient.2
In 1865, Albrecht von Graefe described a scleral incision made with a single passage of a knife, followed by the creation of an iridectomy. For this procedure he preferred the use of general anesthetics, especially chloroform.4 He noted that there were potential dangers if the patient strained while awakening from anesthesia, and this may have been one of his main incentives for reducing the size of Daviel’s corneal flap incision.
The next great advance in the evolution of anesthesia had its origins in 1855, when Gaedicke isolated the alkaloid of the coca plant. In 1860, Nieman noted its anesthetic effect on his tongue, and named it cocaine. Carl Koller further described its use as a local anesthetic, and in 1884 Knapp5 and Turnbull6 both reported on the use of cocaine in eye surgery. Knapp described a technique for cataract removal under topical anesthesia using frequent administration of cocaine drops. He also mentioned retrobulbar injection of cocaine for enucleation (the hypodermic needle had been developed in 1853 by Alexander Wood).7 Turnbull introduced another anesthetic technique for enucleation, using topical and sub-Tenon’s cocaine.
An appreciation of the systemic and local toxicity of cocaine soon followed; episodes of syncope, excessive stimulation, hallucinations, and even death made it a far from perfect anesthetic. In addition, its corneal epithelial toxicity and drying effect, as well as its prolonged hypesthesia, led to cases of exposure keratopathy and ulceration.
In 1904, the next advancement in ophthalmic anesthesia began with Einhorn’s discovery of procaine hydrochloride, which could be used for infiltration, instillation, and nerve block anesthesia without the toxic effects of cocaine.2 Procaine had no inherent vasoconstrictive effects, was rapidly absorbed, and had a short duration of action. Therefore, epinephrine was added to slow absorption and thus hasten, intensify, and lengthen the anesthetic effect. This addition, however, introduced the cardiovascular side effects of sympathetic stimulation in susceptible individuals.
A decade later, Van Lint was the first to describe a method for blocking the orbicularis muscle of the eye to prevent blepharospasm during cataract surgery.8 He injected a combination of procaine and epinephrine near the lateral orbital rim, blocking the terminal branches of the facial nerve and innervating the orbicularis. He advocated waiting 30 to 60 minutes before surgery, thus allowing the block to have its full effect. This block was easy to perform and had a good rate of success. Its localized effect was an advantage; however, eyelid edema, bruising, and bleeding were its main drawbacks.
O’Brien originated a method for a more proximal facial nerve block in 1929.9 He injected procaine anterior to the tragus of the ear, over the condyloid process of the mandible. He used 2 mL of anesthetic and advised waiting 5 minutes before operating. Although the block was found to be safe, with a reduced risk of bleeding and intravascular injection, the anatomical variability of the zygomatic, mandibular, and buccal branches of the facial nerve reduced the certainty of a complete block.
In 1943, Lofgren and Lundquist synthesized lidocaine, and 3 years later Lofgren reported on its anesthetic properties.10 It was found to have a faster onset, better diffusion, and longer duration than procaine. In addition, its early proponents believed that lidocaine was less toxic.11 However, more toxicity was observed in higher concentrations. Circulatory depression was also associated with lidocaine, and respiratory depression was noted with procaine.12
In 1949, Atkinson13 reported on the use of hyaluronidase to increase the diffusion of procaine. His method originated in the observation that aqueous testicular extract increased the spread of vaccinia virus.14 This extract was later identified as hyaluronidase.15 Atkinson found that the addition of 6 turbidity-reducing units per milliliter to a solution of 2% procaine with epinephrine provided more profound anesthesia, without reducing the duration of action.
In 1953, Atkinson proposed another approach to blocking the facial nerve. He introduced his needle through an intradermal wheal at the inferior edge of the zygomatic bone, “A little posterior to the lateral margin of the orbit.”16 He infiltrated anesthetic along the zygomatic arch, which he thought was the ideal site to block the upper branches of the facial nerve, sparing those innervating the lips and lower facial muscles. The benefits of this method included the avoidance of lid edema and injection into major vessels and nerves. As with O’Brien’s technique, however, its main drawback was its unpredictability because of anatomic variability.
A decade later, Nadbath and Rehman17 introduced the most proximal variation on the facial nerve block. They injected anesthetic behind the mandibular ramus to block the main trunk of the facial nerve, where it exited the stylomastoid foramen. Although this approach was the least subject to anatomic variation, its site was a veritable minefield of major blood vessels and cranial nerves. In addition, access to the dura surrounding the spinal cord was reported when this method was used in certain frail patients, with resultant respiratory depression and paralysis.18 More commonly, hoarseness, pooling of secretions, and dysphagia were noted when the glossopharyngeal, vagus, and spinal accessory nerves were blocked along with the facial nerve.19
The literature of the next two decades is filled with case reports of complications of retrobulbar anesthesia, the most serious being blindness and death.20,21,22,23,24,25,26,27,28,29,30,31,32 Alternatives to standard intraconal retrobulbar anesthesia were employed as well. In 1985 and again the following year, Davis reported on the use of peribulbar anesthesia.33,34 He credited Kelman for its introduction in the mid-1970s, Davis’s technique involved three injections: two given anteriorly, into and just beneath the upper and lower orbicularis muscle, and one posteriorly, along the floor of the orbit near the equator of the globe. Although Davis cited 1,600 cases without complication,34 it took only a year from the date of his publication for the first reports of globe penetration to be published.35,36
Transconjunctival retrobulbar anesthesia was also introduced in the mid-1980s.37 Gills37 advocated this method to reduce the potential for globe perforation. It was also intended to avoid the need for a separate facial nerve block.
In 1990, Hanson and colleagues38 described a modification of Turnbull’s sub-Tenon’s technique. Although sub-Tenon’s anesthesia had not been forgotten in the intervening 106 years, it had been relegated to a mostly ancillary position. Atkinson16 advocated the technique as a supplement to retrobulbar anesthesia in patients with preoperative inflammation. The author observed Dr. Arnold Turtz, at the Manhattan Eye, Ear and Throat Hospital, perform sub-Tenon’s with a blunt, metal cannula to improve the anesthetic effect of a retrobulbar block and to provide postoperative anesthesia to patients who had received general anesthesia.
In 1950, Kirby2 reported his preference for sub-Tenon’s over retrobulbar anesthesia, because of the frequent complications of retrobulbar hemorrhage and proptosis with the latter technique. He routinely used a needle to inject a combination of procaine, pontocaine, and potassium sulfate before surgery. Forty years later, Yanoff39 described an ocular perforation with the anterior sub-Tenon’s injection. In 1992, the author reported on the elimination of the needle in sub-Tenon’s anesthesia through the use of a flexible, blunt, polyethylene cannula.40 In the same year, Stevens41 described the use of a blunt, metal cannula in delivering sub-Tenon’s anesthesia without a needle, a method similar to that of Turtz.
The 1990s also heralded the resurgence of topical anesthesia. Although Koller had introduced topical cocaine in 1884, its toxicity limited its popularity. In 1956, Atkinson42 had reported using tetracaine (pontocaine) for topical ocular anesthesia. In 1965, Thorson and co-workers43 had described a topical proparacaine anesthetic in strabismus surgery. In 1986, Shimizu44 had demonstrated the use of topical cocaine (3%) in performing clear corneal cataract surgery. In 1992, Fichman45 presented a method for performing topical anesthesia with tetracaine, and began popularizing its use in the United States. This was also the year that the author and Stevens separately described their use of blunt cannula subtenons anesthesia for cataract surgery through an anterior or parabulbar, and posterior approach, respectively.40,41
In an effort to address the inadequacies of topical anesthesia Gills and others proposed the addition of intracameral unpreserved lidocaine in the late 1990s.128,129 These reports were followed by randomized controlled studies refuting their claims of additional anesthetic effect.130,131
Many surgeons who lecture and write on topical anesthetic techniques use the term “vocal local” to emphasize the importance of constant communication with the patient during the procedure. In his discussion of papers presented at the 16th annual session of the American Academy of Ophthalmology and Otolaryngology in Chicago in 1955, Sadove remarked, “I want to emphasize that a few carefully chosen words are as potent as any sedation … vocal is about as good as local.”46
It is easy to see that the rediscovery and modification of previously described techniques has been the driving force in the evolution of ocular anesthesia since 1884.
ANATOMIC PERSPECTIVES
Understanding how to provide the most effective ocular anesthesia in the safest manner requires an anatomic knowledge of the nerves, blood vessels, muscles, and bony landmarks of the orbit, face, and globe. Although this anatomy is unique to any given patient, some basic rules apply that can be of great help.
The first consideration in providing anesthesia for cataract surgery or any other purpose is understanding the goals of the block. Which parts of the eye does one intend to leave without sensation? Which muscles does one wish to paralyze? Once these questions are addressed, the next task is to understand the cranial neuroanatomy.
The details of trigeminal, oculomotor, and orbital anatomy are beyond the scope of this chapter. The reader is referred to Ocular Anesthesia (WB Saunders, 1997) and Atlas of Clinical and Surgical Orbital Anatomy (WB Saunders, 1994). A brief summary follows.
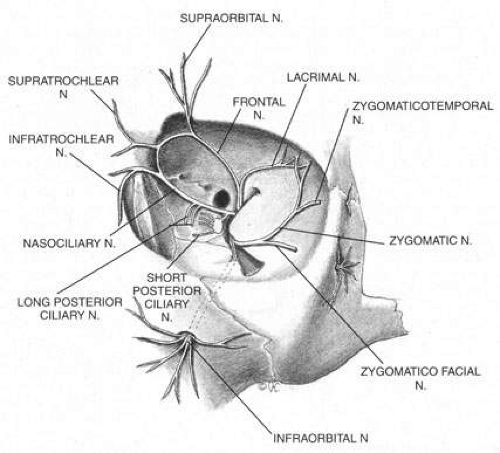
The trigeminal nerve carries the sensory innervation of the eye and adnexa in three divisions: ophthalmic, maxillary, and mandibular. Except for a portion of the sensory input from the lower lid that is carried by the maxillary division, the sensory fibers of the eye and adnexa are found in the ophthalmic division. This division in turn has three components: frontal, lacrimal, and nasociliary, as shown in Figure 1. The frontal nerve usually branches into two more divisions: the supraorbital, which carries sensation from the conjunctiva and skin of the central two-thirds of the upperlid; and the supratrochlear, which carries sensory fibers from the medial third of the upper lid. The lacrimal nerve carries sensory input from the skin and conjunctiva of the lateral aspect of the upper lid.47 The nasociliary nerve carries sensory fibers from the cornea, iris, ciliary body, perilimbal bulbar conjunctiva, and optic nerve sheath; these fibers proceed through its long ciliary branches and sensory root to the ciliary ganglion. The infratrochlear branch of the nasociliary nerve carries sensory input from the medial canthus, medial portion of lower lid skin and conjunctiva, caruncle, lacrimal sac, and canaliculi.
Once it is known which branches are responsible for carrying sensory input from which structures, an approach can be planned that has a reasonable chance of blocking the targeted area. Because, for example, the nasociliary nerve carries fibers that pass through the intraconal space, a standard intraconal retrobulbar block may provide excellent intraocular and partial surface anesthesia. It could not be expected, however, to effectively block the conjunctiva of the upper or lower lids or the lateral aspect of the globe. Because the frontal and lacrimal branches enter the orbit through the superior fissure, above the annulus of Zinn, and the maxillary division enters the orbit through the infraorbital foramen, below the annulus, an intraconal approach probably would not effectively block the structures these branches innervate. If an intraconal retrobulbar block is the only one administered before surgery, patients can be expected to feel irrigating solutions being dropped on the conjunctiva, away from the limbus; they also will be aware of the lid speculum and any manipulation of the lateral surface of the globe. They will probably attempt to close the eye in response to these stimuli. This is the basis for the traditional facial–retrobulbar block combination.
As has been mentioned, numerous facial blocks have been devised to prevent patients from squeezing the eye shut during surgery. None of these blocks keeps patients from wanting to close the eye—only from succeeding. Because the facial block also involves added discomfort, many anesthesiologists and surgeons provide intravenous sedation along with it. Thus, limiting the initial block to the intraconal retrobulbar space also limits its potential benefits, requiring two supplemental procedures. Anatomy determines effect.
The anterior blocks—peribulbar, parabulbar/sub-Tenon’s, and topical—reduce or eliminate the need for a separate facial block by providing better surface anesthesia than the retrobulbar block. Although the first two also provide intraocular anesthesia through their effect on the nasociliary branch, topical blocks provide only surface anesthesia, so that intraocular sensations, such as stretching of the zonules during filling of the anterior chamber, may be felt throughout surgery. Some authors advocate the addition of a subconjunctival injection to add more anesthetic effect to a topical block.48 Recently, intraocular injections of local anesthetics have been popularized as an adjunct to topical anesthesia. This technique is discussed later in this chapter.
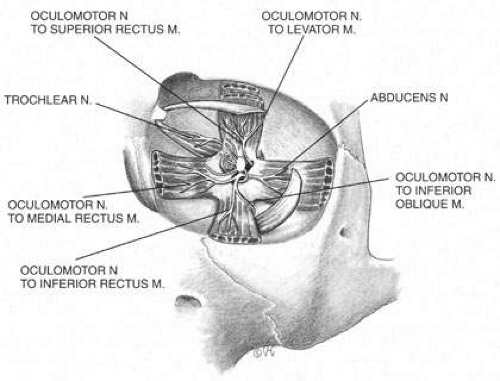
The motor supply of the superior, medial, and inferior rectus, the inferior oblique, and the levator palpebrae superioris is carried by the oculomotor nerve (Fig. 2). It also carries proprioceptive input from these muscles and parasympathetic fibers to the ciliary ganglion. As the oculomotor nerve enters the orbit through the superior orbital fissure, it splits into two divisions, superior and inferior. The superior division is smaller; it courses forward in the superolateral portion of the intraconal space, and turns medially toward the lateral aspect of the superior rectus muscle, where it divides into a network of small branches.49 The innervation of all extraocular muscles is multifocal, with nerve fibers extending distally and proximally between the muscle fibers, before ending at myoneural junctions.47 Some branches innervate the superior rectus, and others pass through it to enter the levator muscle through its inferior surface.
The inferior division of the oculomotor nerve splits into at least three trunks within the intraconal space, and these in turn divide into eight to ten branches as they course forward, lateral to the optic nerve. The medial rectus is innervated by branches that run from beneath the optic nerve into the muscle, beginning at its posterior third. The inferior rectus muscle is similarly penetrated at its posterior conal surface by branches of the inferior division of the oculomotor nerve. The inferior oblique muscle is innervated by a branch that initially contains parasympathetic fibers; these fibers originate in the Edinger-Westphal nucleus and enter the ciliary ganglion inferolateral to the optic nerve. The remainder of this branch then breaks up into smaller fascicles, which penetrate the inferior oblique at its posterolateral aspect.47
The trochlear nerve supplies motor fibers to the superior oblique muscle. It enters the orbit through the superior oblique fissure above the annulus of Zinn, along with the frontal and lacrimal branches of the ophthalmic division of the trigeminal nerve. It crosses the superior rectus origin above the levator and enters the superolateral surface of the superior oblique muscle.47
The abducens nerve enters the orbit through the superior orbital fissure, along with the oculomotor nerve. They are sometimes divided by a dense septum connecting the superior rectus origin to the superior rectus sheath.47 The abducens nerve enters the lateral rectus sheath just anterior to the annulus of Zinn, and first enters the lateral rectus muscle at the medial aspect of the junction of its posterior and medial thirds.47,50
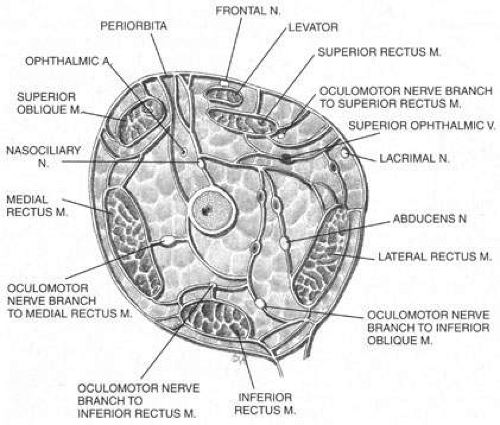
The ciliary ganglion is an irregular structure, measuring 1 mm by 2 mm, that lies just temporal to the optic nerve (Figs. 3 and 4), 7 to 10 mm from the orbital apex.47,51 In it the presynaptic parasympathetic fibers from the Edinger-Westphal nucleus synapse with the postsynaptic fibers that form the short ciliary nerves. Most of these fibers innervate the ciliary muscle, and the remaining 3% to 5% supply the iris sphincter. The ganglion also contains sensory branches of the nasociliary nerve and sympathetic fibers en route to the choroidal vasculature.
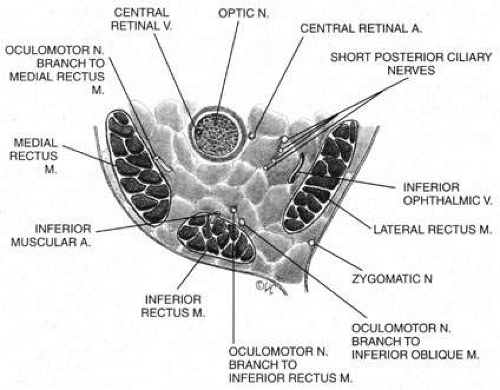 Fig. 3. Posterior orbit. Note the proximity of the optic nerve to the oculomotor branches in this region. |
When attempting to provide akinesia, it should be kept in mind that the motor nerves enter the rectus muscles at the junction of their posterior and medial thirds, or more anteriorly.52 It is also important to remember that these fibers run both distally and proximally between the muscle fibers before they end at the myoneural junctions. A motor block may therefore be achieved at many points along their path. The oculomotor divisions may be blocked in the posterior orbit before their insertion into the rectus muscles, but it is necessary to keep in mind the proximity of the optic nerve, the ophthalmic vein, and the anterior muscular branches to the oculomotor branches in this region (see Fig. 3). Because the nerve and artery supplying the inferior oblique muscle insert more anteriorly, they are more vulnerable to needle trauma from peribulbar or retrobulbar blocks delivered along the floor of the orbit.48 The superior oblique muscle is innervated and receives its blood supply in the posterior orbit. Because it is relatively immobile in the superotemporal orbit, it is possible to injure this muscle with blocks in this area.
Blocks delivered in the anterior or middle orbit depend on diffusion of the anesthetic agent into either the posterior orbit, to the origin of the nerve branches, or into the muscles themselves at the point where distal branches insert into myoneural junctions. The first process is dependent on the anatomy of the connective tissue planes that subdivide the orbit into compartments (see Fig. 4). This architecture varies among patients. The classic teaching of a single intermuscular septum that connects the rectus muscles and divides the orbit into an intraconal and an extraconal space is overly simplified. Histologic examination of the orbit reveals an arrangement of roughly parallel and partially broken septa of various thicknesses, with and without fenestrations.48 This anatomic variability, therefore, accounts for the variability in akinesia seen with orbital blocks.
Atkinson16 discussed supplementing incomplete akinesia by injecting 0.5 to 1.0 mL of anesthetic solution 3 cm back along a rectus muscle, if it was still active after retrobulbar block. He grasped a horizontal rectus muscle with forceps and rotated the eye away from the needle, or placed a muscle hook under the eyelid and separated it from a vertical rectus muscle before injection.16 Because the rectus muscles measure 40 to 42 mm in length without their tendons, which in turn may vary from 3.7 mm for the medial rectus to 8.8 mm for the lateral, Atkinson’s injection was administered 14 to 21 mm anterior to the origin of the muscle. This would place it anterior to the insertion of the oculomotor branch innervating the muscle. Because akinesia can be achieved with this technique, the anesthetic must be diffused within the muscle, blocking distal branches of the oculomotor divisions at their most distal myoneural junctions. However, these injections may produce myotoxicity with prolonged muscle paresis.53,54
Because permanent extraocular muscle damage is more a product of intramuscular or intraneural injection than of the concentration of anesthetic injected,48,55 a less traumatic delivery of anesthetic can be used around the extraocular muscles to achieve akinesia without risking either myotoxicity or needle trauma to the adjacent optic nerve and orbital vessels. Using the sub-Tenon’s space for this delivery allows for such atraumatic akinesia.
GENERAL ANESTHESIA
Although a discussion of the specific techniques for induction of general anesthesia is beyond the scope of this chapter, it is important to consider the indications, contraindications, ophthalmic effects, and complications of this procedure. In 1955, Atkinson16 wrote that the indications for general anesthesia in eye surgery included operations on young children, on adults undergoing extensive orbital surgery, and on those who objected to local anesthesia. General anesthesia also may be considered in patients unable to cooperate, such as the mentally retarded or those with general movement disorders, nystagmus, an inability to lie flat, excessive anxiety, or claustrophobia.
An inability to communicate with the patient may contribute to the decision to choose general anesthesia, but an interpreter can often be employed to instruct a patient preoperatively or even intraoperatively, thus facilitating surgery under local anesthesia. It is also advisable for the surgeon to learn a few crucial phrases in the patient’s language. It can be helpful to have an interpreter write down translations of “look up,” “look down,” “don’t move,” “open the eye,” and “close the eye,” and tape them to the wall of the operating room or to the microscope. Patients with hearing impairment should be encouraged to wear their hearing aids.
Although bleeding disorders have in the past been considered a relative indication for general rather than local anesthesia, newer techniques such as sub-Tenon’s/parabulbar and topical anesthesia avoid the risks of retrobulbar hemorrhage and thus eliminate the advantage of general anesthesia in these cases.
In the 1950s, when intracapsular cataract surgery was the state of the art, general anesthesia was thought to be helpful in the prevention of vitreous loss through “relief of abnormal muscle tone due to fear of pain.”2 Studies of the era compared a 7% loss of vitreous under local anesthesia to a 3% loss under a general anesthesia.56 Stress was constantly placed on the importance of a stay suture to close the eye quickly should the patient lighten under general anesthesia and put a strain on the endotracheal tube. Cataract surgery currently is executed in a more controlled manner, within a closed system. The occasional intracapsular extraction is still performed, of course, as in the case of a subluxed lens with a large zonular dehiscence. In these cases, the lessons of the past should not be forgotten.
In 1980, Badear and co-workers57 published a study demonstrating that elderly patients with a history of myocardial infarction had a significantly higher risk of developing a second infarction with general anesthesia than with local anesthesia. However, a study conducted 3 years later by Lang58 at the Massachusetts Eye and Ear Infirmary demonstrated a low rate of morbidity and mortality with both techniques. In reviewing nearly 15,000 cases between 1977 and 1979, Lang found that they were evenly divided between the two types of anesthesia, and that there were only two postoperative deaths, also equally divided between the two groups. The only two myocardial infarctions occurred in the local group; both were in patients who had a history of infarction more than 6 months before surgery. In comparing the two groups, however, it must be kept in mind that these patients were not randomly selected, and that the patients who were given local anesthesia had a significantly higher average age. What this study does highlight is the overall safety of eye surgery when the appropriate anesthetic technique is chosen for a given patient. Again, the choice of anesthetic should be based on factors other than the type of surgery being performed. As early as 1974, Lynch and co-workers59 compared the rate of vitreous loss and iris prolapse during cataract extractions performed under local to the rate of those performed under general anesthesia and found no significant difference.
The broad range of contraindications to general anesthesia is a chapter in itself, but those that are of special interest in ophthalmology are mentioned here. Up to 90% of patients with myotonic dystrophy, for example, develop cataracts in their early years.60 The myotonia and muscular dystrophy seen in these patients increase the risks of general anesthesia.61 These patients may develop significant bradycardia with a prolonged P-R interval that can be unresponsive to atropine. They also may experience respiratory complications caused by their decreased vital and maximum breathing capacities, resulting in prolonged postoperative respiratory depression. In addition, they experience an increased risk of aspiration caused by delayed gastric emptying and abnormal swallowing. All of these factors make local anesthesia the preferred method in these patients.
Care also must be taken when considering general anesthesia in patients with Marfan’s syndrome. These patients have a high prevalence of cardiovascular abnormalities, such as incompetent or prolapsed valves, arrhythmias, and aortic aneurysms that may dissect with an elevation in blood pressure.62 In addition, pulmonary anomalies such as bronchogenic cysts, abnormal lobulations, and emphysematous changes can lead to spontaneous pneumothorax. The risk of tension pneumothorax increases during controlled breathing.63 For all these reasons, local anesthesia may be safer for such individuals.
When deciding whether to use general anesthesia, the patient’s total physical condition must be taken into account, as must any medications the patient may be taking that could interact with the anesthetic. If possible, smoking should be discontinued. A history of significant prostatic enlargement should be followed up by a urologic consultation before surgery. Patients who are difficult to intubate, such as those with cervical spondylosis, should be identified and carefully evaluated. Previous reactions to general anesthesia should be investigated, as should a family history of unexplained perioperative death or malignant hyperthermia.
Although the incidence of malignant hyperthermia is cited as 1 in 15,000 anesthetic events in children and 1 in 50,000 in adults,64 the true incidence varies with the condition and the anesthesia used. A Danish study estimated an incidence of 1 in 5,000, if episodes of fever, unexplained tachycardia, and masseter muscle rigidity were included in cases where succinylcholine and an inhalation agent were used.65 The specific diagnosis and treatment of malignant hyperthermia is beyond the scope of this chapter, but it is important to remember that with current treatment the mortality rate is approximately 10%. Therefore, in adult patients who may be susceptible to this condition, local anesthesia is obviously preferable to general anesthesia.
When general anesthesia is required in pediatric cases, a history of susceptibility to malignant hyperthermia triggers a cascade of precautionary steps. These include intravenous dantrolene, continuous body temperature monitoring, and the use of drugs considered to be relatively safe for this population, such as narcotics, benzodiazepines, barbiturates, and nondepolarizing muscle relaxants. Careful postoperative monitoring of these patients should be continued for at least 8 hours.
A thorough review of all medications the patient is taking must be made before eye surgery, especially when it is to be performed under general anesthesia. Guidelines for preanesthetic management include the cessation of diuretics, which could cause urinary retention in patients with unsuspected prostatic enlargement, and the discontinuation of those psychotropic drugs that might interact with general anesthetics, such as monoamine oxidase (MAO) inhibitors, which intensify and prolong the anesthetic effect. However, vasodilators and antiarrhythmic agents should be continued through the day of surgery. Their elimination could lead to rebound hypertension and tachycardia, conditions that, along with congestive heart failure and unexplained anemia, represent the major cardiovascular contraindications to general anesthesia.
Because people with diabetes are overrepresented among patients undergoing nearly every type of eye surgery, the perioperative management of insulin and oral hypoglycemics deserves special attention here. General anesthesia and surgery cause a major disruption of the daily routines of a diabetic patient, and the patient’s treatment regimen must be altered accordingly. Type 1 diabetics tend to be more affected by changes in therapy than insulin-dependent, type 2 diabetics, so these juvenile-onset patients should have surgery scheduled as early in the day as feasible.64 Both groups should be given one-third to one-half of their standard morning dose of intermediate- or long-acting insulin. The blood glucose level should be checked before insulin administration and at hourly intervals throughout the perioperative period, and any hyperglycemia should be treated with small amounts of short-acting insulin. Hypoglycemia should be treated with a continuous intravenous infusion of 5% dextrose; the rate of administration should be guided by blood sugar levels.
Oral hypoglycemics should be discontinued on the day of surgery. Patients taking them should have a fasting blood sugar level in the morning, and a continuous intravenous infusion of dextrose as guided by frequently monitored blood sugar levels. Once the patient is able to resume a regular diet, which with most eye surgeries should be relatively soon after the procedure, the normal insulin or oral therapy is resumed.
In patients with diabetes, the type of anesthesia used does not determine the morbidity and mortality of the surgery. Rather, the preexisting status of the diabetes, specifically the presence or absence of retinopathy, nephropathy, and neuropathy, as well as peripheral vascular and cardiovascular disease is predictive of the surgical risk. In a study of diabetics undergoing nonocular procedures, the overall risk of complications was 15%.66 Those with peripheral vascular disease had the greatest risk (35%), and patients with none of the conditions mentioned had a complication risk of approximately 5%.
Ophthalmic medications used in the treatment and preparation of patients undergoing eye surgery also may interact with general anesthetic agents. Epinephrine, for example, may be used on a long-term basis by glaucoma patients for the reduction of intraocular pressure. It also may be used intraoperatively in cataract surgery for its mydriatic effect; in patients who are inadequately dilated, an infusion of epinephrine into the anterior chamber can help to enlarge the pupil enough so that surgery may be performed without the aid of iridectomy, sphincterotomy, or iris hooks. Epinephrine is also routinely added to the fluid used for intraocular irrigation during cataract surgery.
But what are the implications of its use, and how much is safe? The major concern is the interaction between epinephrine and halogenated hydrocarbon anesthetics, which can potentiate ventricular fibrillation. This effect may be especially dramatic with epinephrine and cyclopropane, and this combination surely should be avoided. However, epinephrine can be safely used with halothane, the maximal safe dose having been reported as 68 µg/kg, infused into the anterior chamber.67
The rate of administration is also important. It has been estimated that 10 mL of a 1:100,000 solution of epinephrine may be safely administered in 10 minutes in the presence of halothane; as much as 30 mL per hour may be administered in a healthy 70-kg patient.68 Complications such as hypertension, syncope, headache, diaphoresis, tachycardia, and extrasystoles have been reported in patients using topical epinephrine.69,70 Because as little as 0.5 mg may trigger these effects, and because one drop of a 2% solution contains this amount, it may be advisable to substitute another glaucoma treatment in patients scheduled for general anesthesia.
A glaucoma treatment that is less commonly used but that may be seen in the setting of aphakia is echothiophate, a long-acting anticholinesterase. If a patient has received this drug in the 4 weeks before surgery, anesthetic agents that are metabolized by plasma pseudocholinesterase should be avoided, or at least significantly restricted.71 These include succinylcholine, cocaine, procaine, and chloroprocaine. The use of succinylcholine in this setting can lead to prolonged apnea.
Acetazolamide is a carbonic anhydrase inhibitor used in the long-term treatment of glaucoma, and in the short-term treatment and prophylaxis of postoperative intraocular pressure elevation. Both ocular and renal carbonic anhydrase activity are inhibited by this drug, so that bicarbonate, water, sodium, and potassium are wasted with its use. Patients undergoing long-term acetazolamide therapy are often hypokalemic and hyponatremic, a combination that can potentiate significant arrhythmias under general anesthesia. Because these electrolyte imbalances are worsened by hepatic or renal failure, acetazolamide should be avoided in such cases. It also should be avoided in patients with chronic obstructive pulmonary disease who have a tendency to retain carbon dioxide and therefore to become acidotic. Short-term treatment of intraocular pressure with intravenous acetazolamide has become a popular technique. The drug begins to have an effect in 5 minutes and peaks by 30 minutes. It should be noted that this is a sulfonamide derivative, and so carries a risk, however rare, of anaphylaxis, Stevens-Johnson syndrome, erythema multiform, and aplastic anemia.
General anesthesia is more likely to cause adverse systemic effects than local or ocular complications. Those ocular problems that do occur usually are not serious. They include corneal abrasion, chemical keratitis, hemorrhagic retinopathy, and, rarely, retinal ischemia.
The incidence of corneal abrasion from general anesthesia has been reported to be as high as 44%.72 But simple precautions, such as instilling a bland ointment or taping closed the lids of the unoperative eye, may prevent surface trauma produced by the surgical drape, anesthetic mask, or exposure. Decreased tear production under general anesthesia, proptosis, and poor Bell’s phenomenon may worsen corneal exposure, requiring eyelid suturing in some susceptible patients. Another potential danger to the cornea is the inadvertent trauma by the anesthesiologist during induction.73 Reusable masks also may cause chemical injury to the cornea because of the liquid disinfectants used on them.74 Disposable masks or those that can be autoclaved are simple solutions to this problem.
Postoperative vomiting, difficult extubation, and straining on the endotracheal tube may lead to the formation of retinal hemorrhages, a condition dubbed Valsalva retinopathy.75 This is usually benign, because its source is the venous circulation and the location is intraretinal. These hemorrhages clear without interrupting vision unless they are located in the macula.
Retinal ischemia is by far the most serious adverse effect of general anesthesia. It can be caused by an oversized anesthetic mask, inadvertent pressure exerted by an assistant, or the surgeon’s leaning on the unoperative eye. In the case of posterior segment surgery, it can also result from expansion of intraocular gases in the presence of high concentrations of nitrous oxide.76 Fortunately, this condition is rare, and can be readily prevented if kept in mind during surgery.
RETROBULBAR ANESTHESIA
In 1985, 76% of the members of the American Society of Cataract and Refractive Surgeons, responding to an annual survey, indicated their preference for retrobulbar anesthesia with a facial nerve block for cataract surgery.77 Another 16% preferred retrobulbar without the facial block. Thus 92% of these surgeons selected retrobulbar blocks as their procedure of choice a little less than two decades ago. The same survey published in 2004 listed 9% as preferring retrobulbar plus facial block and 11% as choosing retrobulbar alone, a decline from 92% to 20% overall.132
The technique that most respondents still preferred varies from Atkinson’s42 classic description published in 1955, but not substantially. He wrote:
Good results will be obtained and orbital hemorrhage rarely occurs if the following directions are observed: An intradermal wheal is made. A 3.5-cm 23-gauge needle with a rounded point is introduced through this wheal at the inferior temporal margin of the orbit and the skin is moved upward with the needle until the point just clears the orbital margin. About 0.5 cc of the anesthesia solution is now injected so that pain is not experienced when the orbital septum is pierced. Incidentally, the septum can be pierced more easily close to the orbital margin and is pierced more easily if the needle is rotated producing a boring effect. A pause of a few moments allows the anesthesia to work, during which time the patient is directed to look upward and away from the site of injection. This is done to move the inferior oblique muscle and fascia between the lateral and inferior rectus muscles forward and upward, out of the way. The needle is directed straight back close to the floor of the orbit, until the point is beyond the globe and fascia before directing it upward toward the apex of the orbit for a depth of 2.5 to 3.5 cm depending on the size of the orbit. When the needle has reached the proper depth, one should aspirate before injecting the anesthetic solution in order to determine whether or not the needle has entered a vessel. However, in this location, it would be most unlikely unless there is an abnormally large vessel. The anesthetic solution is then slowly injected, the amount depending on the size of the orbit, the operation that is to be done and whether or not hyaluronidase has been added to the anesthetic solution. When hyaluronidase is not used, 1.5 mL (of anesthetic) is considered a safe amount for intraocular operations. At least 5 minutes should elapse before the operation is begun … more effective results are obtained for cataract extractions and larger injections may be given if hyaluronidase is added to the anesthetic solution. It may be safely injected until there is a noticeable proptosis, which usually occurs after injecting 2 to 3 cc in the average orbit. The hyaluronidase causes the solution to diffuse rapidly and the proptosis quickly subsides. Pressure over the eye, combined with moving it in the orbit for at least 5 minutes, produces still greater diffusion of the anesthetic solution, enhances anesthesia and akinesia, and increases hypotony. Each is an important defense against vitreous loss and other complications.
The biggest change in this technique as used today is the direction of gaze the patient is asked to assume during the block. This came about because of a 1981 study conducted by Unsold and associates, in which computed tomographic images of retrobulbar needle placement in a cadaver, using two different techniques, were studied.78 On one side of the cadaver, the eye was sutured into the position described by Atkinson. Next, a 3.5-cm 25-gauge needle was introduced just above the orbital rim, and was directed superomedially toward the optic canal. On the other side, the eye was sutured into a position of inferotemporal gaze, and the needle was directed in a more inferior direction. In the first case, computed tomography (CT) demonstrated that the needle tip was extremely close to the optic nerve, having crossed underneath it and stopped medially in front of the optic canal. By having the patient look upward and inward, the anesthesiologist would have caused the optic nerve to rotate downward and outward, into or at least very near the path of the needle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree