(1)
Department of Ophthalmology, St. Thomas’ Hospital, London, UK
5.1 Introduction
5.2 Aetiology
5.3 Natural History
5.5 Investigation
5.6 Ultrasound
5.7 Management
5.8 Surgery
5.9 Vitrectomy
5.10 Summary
Abstract
Vitreous haemorrhage is a common accompaniment to disorders of the retina and will often profoundly reduce vision. A small amount of haemorrhage can reduce the vision severely. Occasionally, a good visual acuity can be recorded because the patient through eye movements is able to momentarily visualise the test chart through a clear section of vitreous before the opacified vitreous obscures the vision again. The haemorrhage may be situated in the gel of the vitreous (intragel) or behind a detached gel (retrohyaloid). There may be haemorrhage in the sub-ILM, subretinal or suprachoroidal spaces depending upon the aetiology.
5.1 Introduction
Vitreous haemorrhage is a common accompaniment to disorders of the retina and will often profoundly reduce vision. A small amount of haemorrhage can reduce the vision severely. Occasionally, a good visual acuity can be recorded because the patient through eye movements is able to momentarily visualise the test chart through a clear section of vitreous before the opacified vitreous obscures the vision again. The haemorrhage may be situated in the gel of the vitreous (intragel) or behind a detached gel (retrohyaloid). There may be haemorrhage in the sub-ILM, subretinal or suprachoroidal spaces depending upon the aetiology.
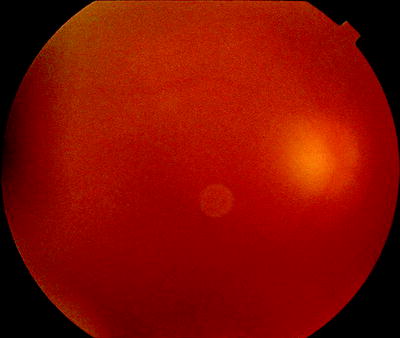
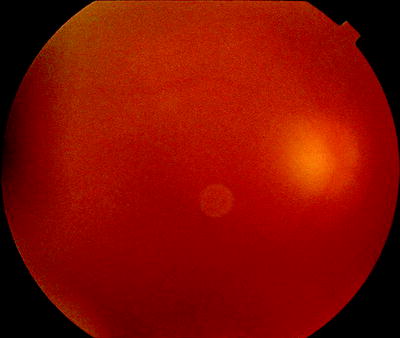
Fig. 5.1
Vitreous haemorrhage may be diffuse in the vitreous gel
5.2 Aetiology
A primary cause of spontaneous vitreous haemorrhage is retinal neovascularisation secondary to retinal ischaemia (commonly diabetic retinopathy or retinal vein occlusion). This usually is associated with PVD, that is, the mobile vitreous tears the fragile new blood vessels in which case subhyaloid haemorrhage is common, but can be seen with vitreous attached if the blood vessels burst either spontaneously or during a period of raised systemic blood pressure (e.g. during isometric exertion).
The cause requiring most urgent management is vitreous haemorrhage from retinal tears associated with posterior vitreous detachment.
Haemorrhage elsewhere in the eye will often disperse into the vitreous cavity, for example, suprachoroidal blood in trauma, subretinal blood secondary to choroidal neovascularisation or blood under the internal limiting membrane in Terson’s syndrome.
Other common causes of vitreous cavity haemorrhage are retinal macroaneurysm (often vitreous is attached) and posterior vitreous detachment without retinal tear formation.
In infants, retinopathy of prematurity is possible. In children, 73 % of cases are due to manifest or occult trauma; other common cause is regressed retinopathy of prematurity (Spirn et al. 2006). Shaken baby syndrome from nonaccidental injury should be considered in bilateral vitreous haemorrhage in children. Rarer causes are juvenile retinoschisis, familial exudative vitreoretinopathy, intermediate uveitis, other uveitis and tumours.
Causes (Lauer et al. 2002; Zhao et al. 2000; Kuhn et al. 1998; Dana et al. 1993; el Baba et al. 1986; Lean and Gregor 1980; Sarrafizadeh et al. 2001)
Diabetic retinopathy
Branch retinal vein occlusion
Retinal tear and rhegmatogenous retinal detachment
Choroidal neovascular membrane
Macroaneurysm
Posterior vitreous detachment
Trauma
Sickle cell retinopathy
Central retinal vein occlusion
Terson’s syndrome
Retinal vasculitis
Intermediate uveitis
Retinoschisis
Needlestick injury
Tumour (vasoproliferative)
Familial exudative vitreoretinopathy
Retinal telangiectasia
Valsalva manoeuvre
5.3 Natural History
The blood in the vitreous gel initially forms a localised clot, but subsequent fibrinolysis causes dispersion of the haemorrhage throughout the gel. During haemolysis, biconcave erythrocytes lose most of their enclosed haemoglobin and change to spheroidal erythroclasts. Biodegradation of the released haemoglobin produces pigments, which often stain the gel an ochre-yellow or orange colour. Such staining of a detached erythroclast-clogged vitreous cortex produces an ‘ochre membrane’ at the posterior hyaloid face.
The mechanisms of spontaneous absorption of vitreous haemorrhage have not been clearly elucidated, though phagocytosis by macrophages, outflow of cells through the trabecular meshwork and syneretic disintegration of the gel play a part. Cells in the trabecular meshwork can reduce aqueous drainage causing raised intraocular pressure and ‘erythroclastic glaucoma’. Another rare consequence of vitreous haemorrhage is ‘synchysis scintillans’, a localised form of cholesterolosis bulbi. It is characterised by the presence of cholesterol crystals in the vitreous cavity, which tend to sediment inferiorly but may be seen to scatter and shower throughout the vitreous cavity after eye movements.
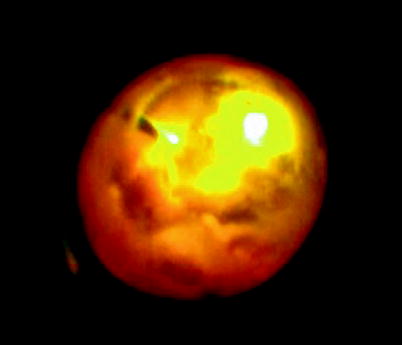
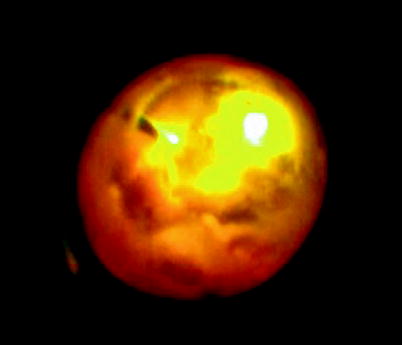
Fig. 5.2
Very thick vitreous haemorrhage has an ochre colour as in this patient with Behcet’s disease
5.4 Erythroclastic Glaucoma
The macrophage-mediated removal of red blood cells clogs up the trabecular meshwork causing a rise in IOP. If a vitreous haemorrhage is left in the eye for weeks or months, glaucoma is an occasional risk. If undetected and untreated, a cupped optic disc can result. If you plan not to operate on an eye with vitreous haemorrhage and are awaiting spontaneous resolution of the haemorrhage, the eye will require periodic IOP checks. If glaucoma occurs, the definitive therapy is removal of the blood by PPV.
5.5 Investigation
The priority with vitreous haemorrhage is determining the aetiology because some causes require immediate intervention. Many cases can be determined from the history of the patient:
Diabetic retinopathy
Branch retinal vein occlusion with a previous symptomatology
Previous loss of vision 1 year ago/laser
Trauma
Traumatic history
Central retinal vein occlusion
Loss of vision 2 years ago
Terson’s syndrome
Headache, neurological signs and symptoms
Needlestick injury
Careless anaesthesia
Sickle cell
Race and blood tests
Retinal vasculitis
Previous treatment
Others are not so obvious:
Branch retinal vein occlusion previously asymptomatic
Choroidal neovascular membrane
Often the presenting complaint in these patients with or without signs of AMD in the other eye.
Macroaneurysm
Posterior vitreous detachment with or without retinal tears
Flashes and floaters may have been present but inconclusive clinical features.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


