Vitreous
Marilyn C. Kincaid
CONGENITAL ANOMALIES
PERSISTENT PRIMARY VITREOUS
Normally, the primary vitreous, or hyaloid system, regresses late in fetal development and is completely resorbed. However, remnants may persist, although they are usually curiosities, without functional significance. Rarely, at term the entire hyaloid system may be present in the eye.
Anteriorly, such remnants typically persist as Mittendorf’s dot, a small whitish opacity on the posterior capsule, just inferonasal to the posterior pole, which corresponds to the anterior site of attachment of the hyaloid artery.1
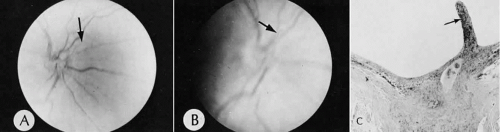
Posteriorly, glial and vascular remnants of the hyaloid artery may persist at the disc and extend into Cloquet’s canal, the visible central space formed by the encroaching secondary vitreous. The glial remnant, called Bergmeister’s papilla, existsas delicate strands or as a membrane overlying the optic nerve head (Fig. 1). Vascular remnants may be filled with blood and may be confused with neovascularization at the disc; however, the remnants do not leak fluorescein.1
PERSISTENT HYPERPLASTIC PRIMARY VITREOUS
Persistent hyperplastic primary vitreous (PHPV) is present at birth and nearly always is unilateral. Because it can cause a white pupil and poor vision, it is part of the differential diagnosis of retinoblastoma.2 However, these eyes are often microphthalmic, whereas eyes with retinoblastoma are normal in size unless there has been involution of the retinoblastoma and secondary shrinkage of the globe. As the name implies, PHPV is the hyperplastic counterpart of persistence of the hyaloid system. PHPV tends to be unilateral, especially in otherwise healthy patients, but has been reported to be bilateral.3 In patients with systemic abnormalities, such as trisomy 13, PHPV is more often bilateral.4
The anomaly consists of vascular mesenchymal tissue, which proliferates behind the lens and pushes it forward. This mesenchymal tissue can contain, in addition to fibroblasts and vessels, adipose tissue, smooth muscle, and cartilage.4 The proliferating tissue draws the ciliary processes inward so that they may be visible through a dilated pupil if the lens is clear. The lens usually becomes cataractous, and frequently the mesenchymal tissue extends through the ruptured capsule posteriorly.5 Rarely, capsular rupture can give rise to a phacoanaphylactic reaction.6
Glaucoma may result from a variety of mechanisms in this anomaly. The angle structures may be immature; therefore, PHPV is part of the differential diagnosis of congenital glaucoma, although angle immaturity is seldom an isolated cause.4,5 These eyes are microphthalmic, so that the anterior segment is crowded and the lens is anteriorly placed. This situation is aggravated by the mesenchymal tissue mass pushing the lens further forward, allowing pupillary block glaucoma to ensue. Other mechanisms of increased intraocular pressure include uveitis and intraocular hemorrhage.4
CONGENITAL CYSTS
Congenital cysts are free-floating cysts in the vitreous cavity that may be clear or pigmented and range from 2 to 12 mm in diameter. They can be bilateral.7 If they are large or centrally located, they can interfere with vision.8 Some are probably traumatic in origin, but other patients have had no history of trauma or surgery. In two reports of congenital vitreous cysts, the cyst wall was composed of pigmented and nonpigmented epithelial cells.8,9 The cells contained mature and immature melanosomes, implying a congenital origin.8 They are usually stable and do not require intervention.
VITREOUS ADHESIONS
POSTTRAUMATIC AND POSTSURGICAL
The vitreous can act as a scaffolding for fibrous proliferation when adherent to adjacent ocular tissues. Trauma and inflammation usually are the inciting causes. With fibrous proliferation, shrinkage and wrinkling of tissues occurs. Electron microscopic examination has shown that the fibrocytes and other proliferating cells often have condensations of filaments near the cell membrane.10 These 60- to 70-nm filaments are composed of actin; this contractile protein explains the ability of these fibrous membranes to shrink, pulling at whatever tissue to which they are attached.11 This formation of contractile filaments is called myofibroblastic differentiation and is a frequent finding in fibrosis and fibrous ingrowth of any cause.12 Actin, however, probably is not the only cause of membrane contractile behavior.13
Adhesion of vitreous to the ciliary body with fibrous proliferation can lead to cyclitic membranes.11 Vitrectomy can lead to fibrous ingrowth overlying the pars plana, at the entry site of the instruments.14
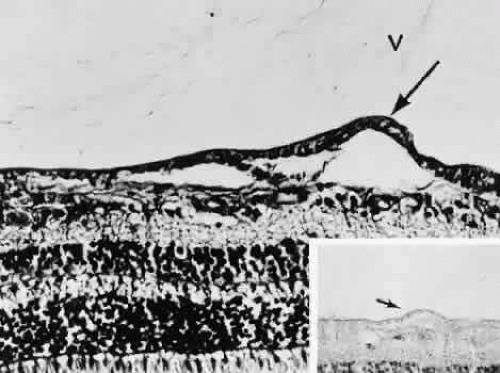
The vitreous normally is adherent around the fovea. Increased traction on the macula by the vitreous is thought to play a role in postoperative cystoid macular edema15 and in the formation of macular holes.16 Previously, most macular holes were assumed to be traumatic in origin. However, with better techniques of biomicroscopy, it has been found that atraumatic holes in older patients are much more common than previously realized. The pathogenesis of these atraumatic idiopathic macular holes has been controversial. It now appears that tangential traction by the vitreous causes a detachment of the foveola with subsequent hole formation.16 Histologic examination of the surgically removed opercula has shown that many contain only glia, without photoreceptors.17
The vitreous is also often adherent along the major vessels. As the vitreous detaches, it peels away from the retina, so that if areas of increased adhesion exist (Fig. 2), a tear may result. There can be hemorrhage because this tear normally occurs across a blood vessel. The vitreous may pull out a fragment of partial-thickness retina, leaving retinal pits, or full-thickness retina, resulting in holes.18,19 The fragment of removed retina, the operculum, gradually resorbs.
VITREOUS OPACITIES
ACQUIRED VITREOUS STRANDS AND FLOATERS
Acquired vitreous strands and floaters are annoying but generally harmless fragments of formed vitreouswith glial proliferations. The strongest attachment of the vitreous to the retina posteriorly is around the optic nerve head. This entire ring sometimes will detach intact, so that a ring is visible in the visual field. Vitreous floaters move as the eye moves.
Vitreous detachment increases in frequency with increasing age. As the vitreous liquefies posteriorly, the formed vitreous collapses anteriorly (Fig. 3). The most firm area of vitreal attachment is the vitreous base, overlying peripheral retina and adjacent pars plana; the vitreous does not spontaneously detach from its base.20
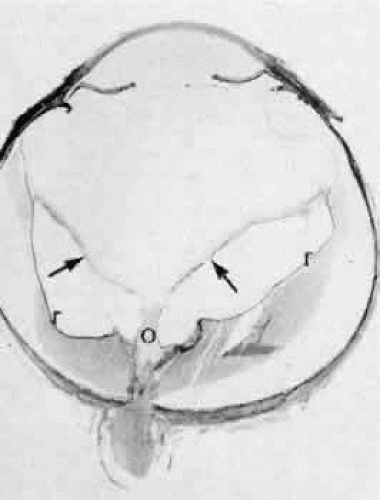 Fig. 3. Vitreous detached posteriorly (arrows) everywhere except over the optic nerve (o). The retina ® is also detached. (hematoxylin and eosin, original magnification, × 5) |
INFLAMMATION
Inflammation in the vitreous may be infectious or noninfectious. Because the vitreous is a good culture medium, organisms of exogenous and endogenous origin may flourish there. Bacterial endophthalmitis often leads to diffuse vitreous haziness, decreased vision, and pain. Vitrectomy can be diagnostic and therapeutic,23 but depending on the clinical setting, vitreous biopsy may be adequate and can be done under sterile conditions in the office.24
Bacteria of exogenous origin generally gain access to the eye from traumatic injury, including surgical injury, either being introduced by a foreign body or through contamination of the inner eye by way of an open wound. Particularly with postoperative endophthalmitis, the normal colonizers of the periocular surface are the most frequent causes.24 Occasionally, the inflammation is more low grade, with a chronic, smoldering course. Such cases can be difficult to diagnose and require biopsy.25
An unusual cause of exogenous infection occurs in so-called sequestered endophthalmitis. Bacteria of low virulence, typically Propionibacterium acnes, apparently are introduced into the lens capsular remnants at the time of cataract surgery. Weeks to months later, they cause a low-grade uveitis.26 In some cases, YAG laser capsulotomy has led to a fulminant endophthalmitis.27 Several cases have been examined histologically after the lens remnants have been removed. The organisms appear as clusters within the capsular remnants.28
Endogenous bacterial infection is usually seen in immunosuppressed patients; bacteremia in immunocompetent patients rarely leads to endogenous infection.29
Whipple disease is an unusual disease of the gastrointestinal tract and manifests as malabsorption and steatorrhea. It is characterized by foamy, periodic acid-Schiff-positive macrophages in the intestinal mucosa. These macrophages also are occasionally present in the vitreous. Vitrectomy can be diagnostic.30 The disease has been shown to be caused by a bacillus.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree