Vitrectomy
Frank J. Mccabe
Carl D. Regillo
William E. Benson
In 1968, Kasner introduced the “open-sky” technique for removal of formed vitreous. This technique required a large limbal incision, lensectomy, and mechanical removal of the vitreous with scissors.1 Kasner proved that the eye could tolerate removal of the vitreous without severe complications. Nevertheless, few elective vitrectomies were done until 1971, when Machemer performed the first closed, pars plana, vitrectomy.2,3,4 The instrument for performing the vitrectomy was a single probe called VISC. VISC stood for vitreous-infusion-suction-cutting because this large, bulkyprobe performed all of these functions. Machemer pioneered this technique and later introduced the intraocular fiberoptic light pipe.3,5,6 The next giant step was the separation of the various functions of the single probe into separate probes for aspiration-cutting, illumination, and infusion.7 This ingenious use of a separate infusion line allowed miniaturization and standardization of the size of the various vitrectomy instruments needed for surgery.
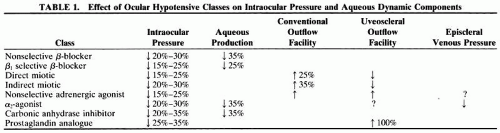
Over the years, considerable advancement has been made in vitreoretinal instrumentation, including high-speed vitrectomy cutters, illuminated forceps and picks,8 and the diamond-dusted silicone tip cannula.9,10 Other improvements include less-toxic irrigating solutions,11,12,13 improved contact lenses, safe intraocular diathermy, flexible iris retractors,14 and endolaser photocoagulation. Motorized scissors have dramatically decreased the incidence of iatrogenic retinal tears because membranes that formerly had to be peeled from the retina can now be segmented. Special mention must be given to the pioneering work by Chang15 with perfluorocarbon liquids (PFCLs), which are a major advance in the unrolling of giant tears and in the evacuation of subretinal fluid in selected cases. Silicone oil (SO), first introduced by Cibis in 1962, has been increasingly used since the early 1980s.16,17 The latest major advance in vitreoretinal surgery has been the introduction of wide-field viewing systems, which allow a panoramic view of the retina.18,19 These technologic advances have helped to expand the indications for vitrectomy greatly (Table 1).
PREOPERATIVE EVALUATION HISTORY TAKING
A complete medical history is obtained from all patients. Many patients who require a vitrectomy have diabetes mellitus and other medical problems. In one report, abnormalities in the cardiovascular or renal function or both were found in 98% of patients with diabetes undergoing vitrectomy.20 Patients requiring renal dialysis may have an increased risk of operative problems as many have a bleeding diathesis. The ocular history is critical because the surgeon must take into consideration other possible causes of decreased vision such as severe glaucoma, ischemic optic neuropathy, macular edema, and arteriolar occlusive disease. The duration of certain conditions influences the visual prognosis. A diabetic macular detachment of 2 months or shorter is twice as likely to achieve a good visual result than those of 13 months’ duration or longer.21 Macular holes of 6 months’ duration or longer are less likely to achieve significant visual improvement.22 Patients with epiretinal membranes and a longer history of blurred vision showed less visual improvement in visual acuity than did patients with a short duration of symptoms.23
OCULAR EXAMINATION
A nearly absolute contraindication to any ocular surgery is no light perception (LP).24 Normal pupillary responses are a significant predictor of successful visual results in patients with diabetes.21 An opaque cornea can now be addressed with various styles of temporary, intraoperative keratopros-theses.25,26,27 The examiner should inspect the eye for iris neovascularization (NVI) with slit-lamp biomicroscopy and gonioscopy. NVI portends a poor prognosis in patients, who should be treated with panretinal photocoagulation (PRP) before vitrectomy if possible.21,28,29,30 In some cases, especially those in which membranes must be peeled or delaminated from the retina, a cataract may need to be removed to permit safe completion of the surgical objectives. It is best to recognize this before surgery so that preparations for placement of a posterior chamber intraocular lens (IOL) and vitrectomy in one operation can be made.31,32,33,34,35,36,37,38 In patients with pseudophakia, the type of lens should be determined. Silicone IOL implants may have SO droplets condense on the back surface of the lens. In addition, silicone implants are more predisposed to have air condense on the posterior surface of the lens.39,40
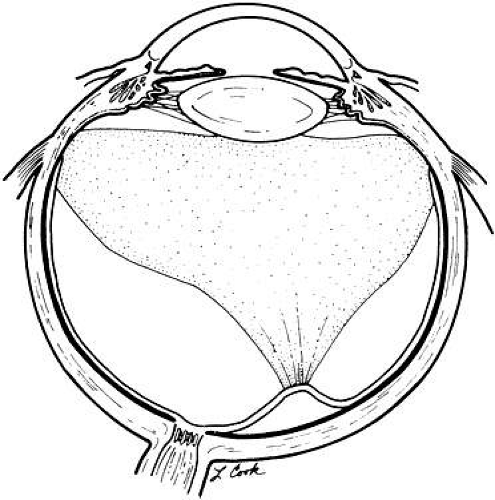
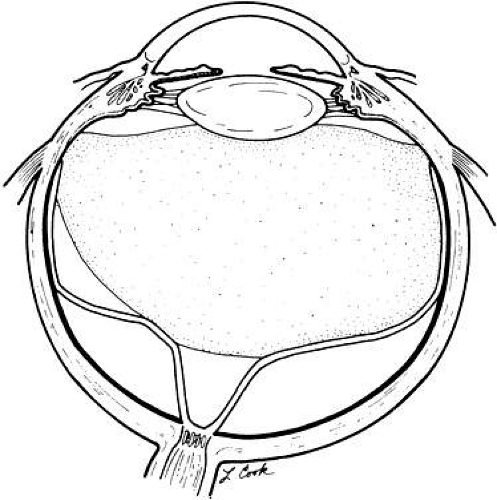
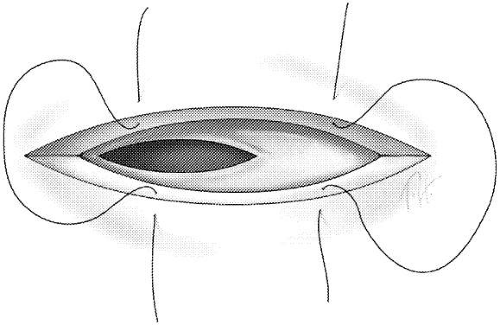
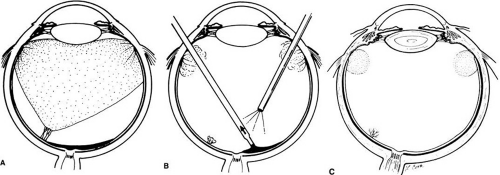
Obviously, a careful retinal examination with indirect ophthalmoscopy and slit-lamp biomicroscopy is essential. The status of the posterior hyaloid should be noted. The location of retinal breaks, the extent and nature of membrane proliferation, and other pertinent findings should all be documented carefully. For example, retinal detachments caused by small areas of vitreoretinal adhesion (Fig. 1) or that have “bridges” between localized detachments are easier to repair than those with broad adhesions (Fig. 2). Iatrogenic retinal holes are more common in patients with longstanding retinal detachment and ischemic, thin retina than in patients with recent detachment and well-vascularized retinas. These factors help determine the patient’s prognosis and the procedure length.
ANCILLARY TESTING
Ultrasonography is an invaluable tool in evaluating eyes with opaque media. Ultrasound can aid in diagnosing vitreous membranes, retinal detachments, intraocular foreign bodies (IFBs), perforating injuries, choroidal detachments, intraocular tumors, and so forth accurately. It is important to recognize the distinctive funnel-shaped pattern that identifies retinal detachment with severe proliferative vitreoretinopathy (PVR).41 Such detachments are challenging and may require more advanced vitreoretinal techniques. Ultrasound in trauma cases also provides prognostic information. Eyes undergoing vitrectomy after penetrating trauma fared worse if preoperative ultrasound detected retinal detachment, subretinal blood, massive choroidal detachments, or posterior exit wounds.42 Ultrabiomicroscopy is a recent ultrasound imaging technique that provides a high-resolution view of the anterior segment. In recurrent vitreous hemorrhages after diabetic vit-rectomy, ultrabiomicroscopy can evaluate the sclerotomy sites for possible neovascularization.43,44
In eyes with opaque media, there also are tests that can assess gross retinal and optic nerve function. Color perception, two-point discrimination, and Maddox rod orientation are of limited value.45 The perception of entoptic phenomenon to assess retinal function has had mixed results.21,45,46 The basis for the blue-field entoptic phenomenon is that patients with normal maculae who stare at a diffuse blue-light can see leukocytes circulating in their macular capillaries. An instrument with a blue light bright enough to penetrate dense vitreous hemorrhage is available. It can predict macular function successfully in patients with traumatic vitreous hemorrhage but, in general, is rarely used in clinical practice.46
Electroretinography (ERG) helps to evaluate the overall functional status of the retina. The standard Grass photostimulator may not provide enough light to stimulate the retina in cases of dense vitreous hemorrhage. The resultant flat tracing may falsely indicate a nonfunctioning retina. However, the bright-flash ERG can penetrate dense vitreous hemorrhages. Some of the light actually transverses the sclera to stimulate the retina. Nevertheless, the ability of a preoperative bright-flash electroretinogram to predict visual outcomes is controversial. A patient may have an excellent visual result after removal of a diabetic vitreous hemorrhage but have a flat preoperative ERG. A decision to operate should not be based on a preoperative ERG as it cannot safely predict the outcome in diabetic vitrectomy.47,48 Focal macular electroretinograms recently have been used before and after surgery in select macular conditions.49,50
Other electrophysiologic tests to evaluate visual function are pattern and flash visual-evoked potentials (VEPs). The pattern VEP evaluates macular function and is not useful in patients with opaque media because the pattern cannot be perceived.51 A normal response to a flash VEP depends on a normally functioning retina and optic nerve. A bright flash is not essential to generate the VEP because this test does not require as much light as does the ERG. Both the latency and amplitude of the tracing provide useful information.52 If the retina is totally detached, the VEP is absent. If it is partially attached, the VEP is reduced. A delayed VEP indicates optic nerve dysfunction. The amplitude of the flash VEP at stimulus rates of 10 flashes per second is largely influenced by the macular status. At 20 to 30 flashes per second, the amplitude depends more on the integrity of the optic pathways. Therefore, the VEP may be an excellent predictor of postoperative visual acuity. However, the prognostic value of a preoperative flash VEP for a diabetic vitrectomy is controversial. Similar to ERG, a decision to operate should not be based on a preoperative VEP as patients may obtain good vision despite a reduced VEP.47,48
Computed tomography scans have been shown to be helpful in localizing foreign bodies in or near the sclera. Computed tomography and ultrasound are more sensitive techniques than are plain x-ray films for detecting and localizing IOFBs.53,54 The sensitivity of computed tomography scan for detecting IOFBs is 100% for objects larger than0.06 mm.55 Magnetic resonance imaging is contraindicated in IOFB cases because of potential movement of magnetic IOFBs by the powerful magnetic resonance imaging magnets.
A new technique that is helpful in preoperative assessment of patients is optical coherence tomography, which is a noncontact, noninvasive imaging technique that produces high-resolution, cross-sectional images of the retina.56 The interaction between the posterior hyaloid and the retinal surfaces can sometimes be difficult to discern. Optical co-herence tomography can assist in diagnosing vit-reomacular traction syndrome and distinguishingfull-thickness holes from pseudoholes, cysts, and partial-thickness holes.57,58,59 This technique also can be used to assess macular hole closure after vitrectomy and macular edema before and after vitrectomy for diabetic macular edema.60,61,62
SURGICAL ANATOMY
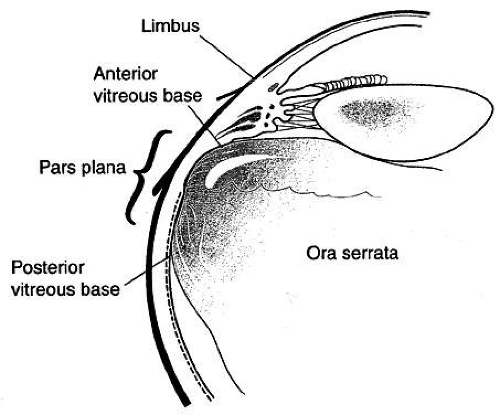
It is essential to be familiar with the surgical anatomy when performing a vitrectomy. The pars plana, the posterior section of the ciliary body, is the entry site to the vitreous cavity for ocular instruments in pars plana vitrectomy (PPV). The pars plana is around 4 mm wide in adults and is nded anteriorly by the pars plicata (ciliary processes) and posteriorly by the ora serrata. In adults, the ora serrata is 6 to 7 mm posterior to the limbus nasally and 6 to 8.5 mm temporally.63 In phakic patients, the pars plana should be entered 4 mm posterior to the limbus and in pseudophakic patients 3 to 3.5 mm posterior to the limbus (Fig. 3). This technique ensures that the entry of the ocular instruments will be anterior to the ora serrata to prevent a retinal tear or detachment and posterior to the well-vascularized pars plicata to avoid hemorrhage. It also is important to enter at the correct angle to avoid damaging the lens.
The vitreous is a gel-like structure that is comprised of collagen fibrils, hyaluronic acid, hyalocytes, and water. The collagen fibrils in the peripheral vitreous condense to form a thin layer called the vitreous cortex, which surrounds the central gel and is adherent to the internal-limiting membrane (ILM) of the retina. The vitreous cortex has varying degrees of retinal adherence. It is most adherent to the ILM at the vitreous base. The vitreous base is a band about 6 mm in width that overlays the ora serrata and pars plana. The vitreous cortex also is more adherent to the optic nerve head, blood vessels, and perifoveal region. In disease states, as discussed below, the vitreous cortex may be strongly adherent to neovascularization, chorioretinal scars, and fibrous proliferation.64 After the vitreous cortex separates from the ILM, the subsequent thin layer is referred to as the posterior hyaloid face.65 Understanding the relationships between the retina and vitreous is extremely important in vitreoretinal surgery.
BASIC VITRECTOMY TECHNIQUE
Anesthesia for PPV can be general or local. General anesthesia should be considered for long cases, for patients unable to tolerate local anesthesia for physical or psychological reasons, and for children. Local anesthesia is used in most cases. The options for local anesthesia are retrobulbar, peribulbar, topical, and sub-Tenon’s injections of an anesthetic solution. Retrobulbar and peribulbar injections are effective forms of anesthesia but rarely can beassociated with significant complications, including globe penetration, hemorrhage, arterial occlusions, and optic nerve damage.66,67,68 Sub-Tenon’s injection with a blunt cannula provides excellent anesthesia and has minimal complications.69,70,71 In select, uncomplicated cases, topical anesthesia has been successful but is not used routinely.72,73
Intraocular irrigating fluids have been studied extensively, and Balanced Salt Solution (BSS)-Plus (Alcon) has been shown to be a safe irrigatingsolution.11,12,13 BSS-Plus contains glutathione, glucose, magnesium, bicarbonate buffer solution, and Ringer’s lactate solution. Whether BSS-Plus is superior to BSS has not been definitely established. In a diabetic vitrectomy, the lens may develop posterior capsular opacification secondary to an osmotic shift of water into the lens. The addition of 3 ml of 50% dextrose to BSS or BSS-Plus has been shown to prevent cataract development during diabetic vit-rectomy.74
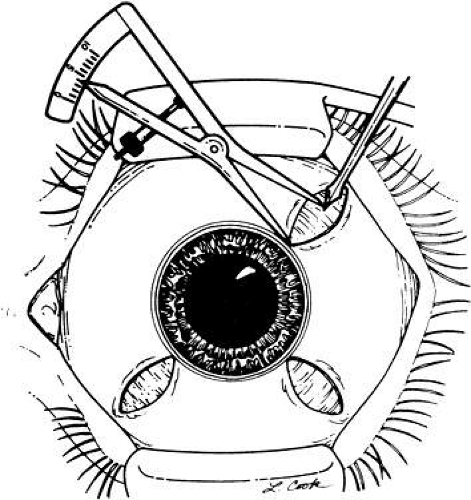
PPV requires an operating microscope. A foot pedal to control the zoom magnification, focusing, and X-Y microscope is essential. A beam splitter for the surgical assistant should be present. There are many types of lenses that can be used with the operating microscope. Planoconcave, hand-held irrigating lenses, such as the Charles lens, often are used. The field of view is about 20 degrees, and the fluid meniscus rinses away debris and allows prism effect. If no assistant is available to hold the lens, Landers sew-on lenses can be used. If the eye is gas filled, biconcave lenses, such as the Machemer lens, need to be used for viewing.75 There are several options for viewing the peripheral retina. The surgeon can use the Charles lens with scleral depression, prismatic lenses, or the recently developed wide-field viewing systems, which require an inverter on the microscope but offer superior depth of focus, a wider angle of view, and are almost independent of the pupil size. They also allow for a superior view through native lens or lens implant opacities, particularly condensation on the posterior lens surface during air-fluid exchange. The binocular indirect ophthalmoscope is a noncontact wide-field viewing system that is used often (Fig. 4).18,19 One recent study suggested that wide-field viewing systems decrease surgical time and allow more complete laser treatment.76 Another study showed that the binocular indirect ophthalmoscope has a decreased rate of intraoperative corneal epithelial defects.77
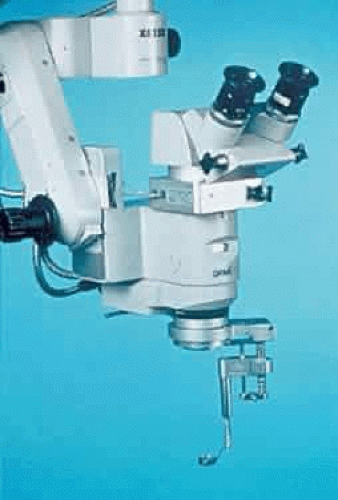 Fig. 4. Binocular indirect ophthalmoscope is shown attached to the operating microscope. (Courtesy of Insight Instruments Inc, Sanford, FL.) |
A hand support is preferred for vitrectomy surgery (Fig. 5). The surgeon rests both hands throughout the operation, avoiding fatigue and achieving fine control for intravitreous manipulations. The level of the hand support usually is at the patient’s ears but should be individualized for the surgeon and patient. A sterile plastic drape, used to cover the patient, is pushed down into the space between the patient’s head and the hand support. This forms a trough to collect fluid that would otherwise spill onto the floor. The microscope also can be covered with a sterile plastic drape.
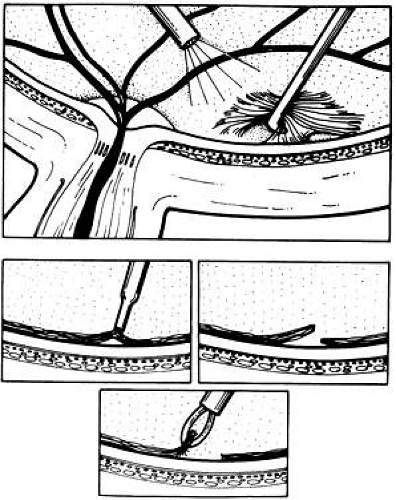
Small radial or triangular incisions through the conjunctiva and Tenon’s capsule are made superonasally, superotemporally, and inferotemporally. Hemostasis is maintained with bipolar diathermy. The entry incisions are parallel to the corneoscleral limbus and are 4 mm posterior to it in phakic eyes and 3 to 3.5 mm in aphakic and pseudophakic eyes (Fig. 6). The incisions are made with a 20-gauge microvitreoretinal (MVR) blade. It is important that the incisions (through the sclera, uvea, and pars plana) be just large enough to permit entry of the desired instrument. A 1.4-mm linear incision rounds out to 0.89 mm, the diameter of the blade shaft.78 If the incisions are too long, irrigation fluid leaks around the instrument and out of the eye, making normal intraocular pressure (IOP) difficult to maintain without using large volumes of irrigating solution. In addition, if a total gas-fluid exchange is later attempted, the gas escapes from the eye. All blades used for incisions must be sharp, so that when introduced into the eye, they do not push pars plana epithelium or vitreous base ahead of them, causing a retinal tear or dialysis. The MVR blade should be held at an approximately 70-degree angle and passed toward the optic nerve. It is important to enlarge the sclerotomy incision from the inside out to ensure that the internal opening is as large as the scleral opening (Fig. 7). When the media are clear, the surgeon should push the MVR tip into the eye until it can be seen through the pupil.
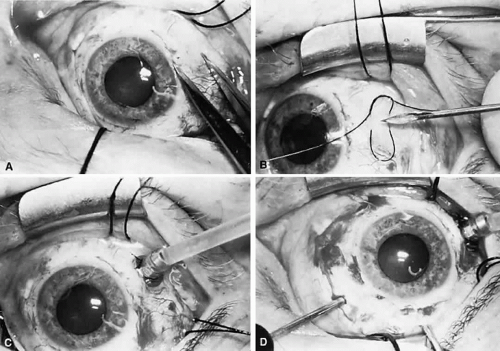
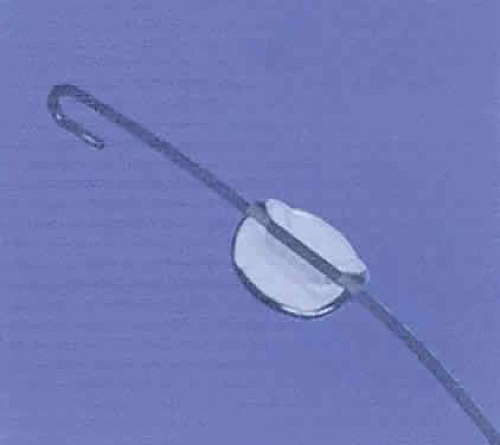
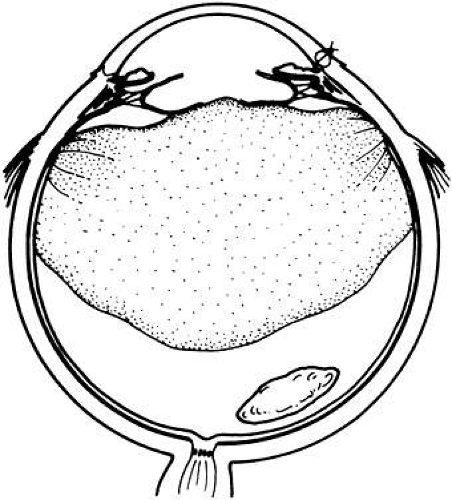
The first incision is for the infusion cannula, which is placed in the inferotemporal quadrant, just inferior to the lateral rectus muscle. If the cannula is placed too far inferiorly, it presses against the lid speculum during inferior rotations of the globe and may hinder access to the inferior portions of the eye. A 5-0 nylon mattress suture, which secures the base of the infusion cannula, is placed before entering the eye (Fig. 8). In most cases, a 4-mm cannula is used. In pseudophakic/aphakic eyes, a6-mm cannula can be used to assist in visualization of the cannula tip in cases of media opacity. The infusion cannula is twisted through the sclerotomy site in an oscillatory fashion, ensuring the bevel is facing the center of the eye. The surgeon, using the indirect ophthalmoscope if necessary, must verify that the cannula has passed cleanly through the pars plana epithelium before turning on the infusion.79 A small pupil may hinder the view of the cannula and the subsequent surgery. Flexible iris retractors are an easy and effective way for enlarging a small pupil (Fig. 9).14 If there are opaque media, the surgeon must provide infusion with a hand-held infusion needle whose tip can be seen until the media are clear enough to see the cannula. It is difficult to place an infusion cannula into the vitreous cavity if there is a choroidal detachment. The safest technique is to drain the detachment while maintain-ing the intraocular volume with irrigating solution through a 22-gauge needle.80 The needle is introduced through the limbus in aphakic eyes and through the pars plana in phakic eyes.
After the infusion is turned on, incisions are made in the superonasal and superotemporal quadrants for the vitrectomy instrument and fiberoptic light pipe. These incisions should be made 150 to 160 degrees apart, just above the lateral and medial rectus muscles. This allows instrument access to both the superior and inferior retina. It is important not to make sclerotomy sites in a “soft” eye. If necessary, fluid should be injected with a 30-gauge needle at the pars plana or limbus to pressurize the eye.
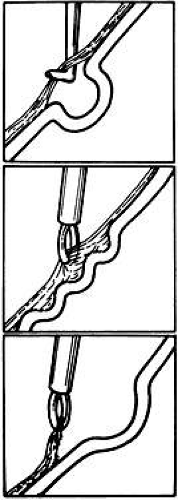
There are two basic types of vitrectors: those that use a rotating or oscillating inner blade and those that use a guillotine-like chopping blade (Fig. 10). Today, guillotine cutters are used most often. A pneumatically driven inner tube moves up and down inside a fixed outer tube. Vitreous is aspirated into the cutter when the openings of the inner and outer tubes are aligned and then chopped off as the inner tube moves up and down. The suction for vitreous aspiration is through the inner tube. For a core vitrectomy, high cut rates (600 to 800 cycles per second) and moderate suction (200 mmHg) should be used. Higher cut rates minimize vitreoretinal traction and decrease the incidence of iatrogenic retinal breaks. The Alcon vitrector is a well-designed, disposable instrument. It is lightweight to prevent fatigue, hourglass-shaped to prevent slippage, and disposable so that the blades are sharp (Fig. 11). Vitrector probes are now available that can achieve cut rates of approximately 1200 cycles per second, which can allow for fine shearing of vitreous close to the retinal surface (Fig. 12).
 Fig. 11. This vitrector is lightweight to prevent fatigue, hourglass-shaped to prevent slippage, and disposable so that the blades are sharp. (Courtesy of Alcon, Fort Worth, TX.) |
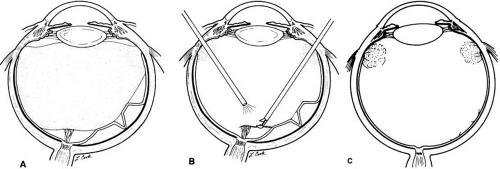
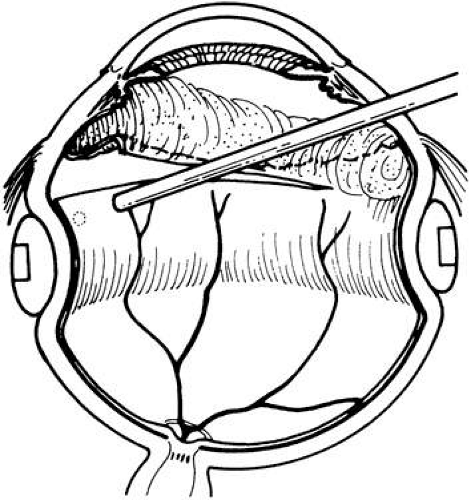
PPV is a bimanual technique. Typically, one sclerotomy port is used for a fiberoptic light source and the other sclerotomy for the vitrector or other instruments. Vitrectomy instruments should be held lightly in the surgeon’s fingertips. It is important to position the instruments at the correct angle to avoid damaging the lens when entering the eye. The initial goals of the vitrectomy are to clear the axial media and to remove anteroposterior vitreoretinal traction. If there are media opacities, they should be removed from the central vitreous (Fig. 13). The status of the posterior hyaloid must be noted. If there is a complete posterior detachment, an edge of the posterior hyaloid should be followed out to the periphery circumferentially (Fig. 14). If there is a partial posterior detachment, the posterior hyaloid should be incised over attached retina and away from the macula. The incised edge should then be followed circumferentially. If there is preretinal blood, it can be removed with the vitrector on suction or with an extrusion cannula (Fig. 15). If the hyaloid is completely attached, the central vitreous should be removed with the cutter. Application of active suction with the vitrector or soft-tipped extrusion cannula over the optic nerve head should elevate the posterior hyaloid face. The soft-tippedcannula bends with engagement of the posterior hyaloid, which is called the fish-strike sign (Fig. 16). The elevated hyaloid can be incised with the cutter and an edge followed out to the periphery circumferentially.
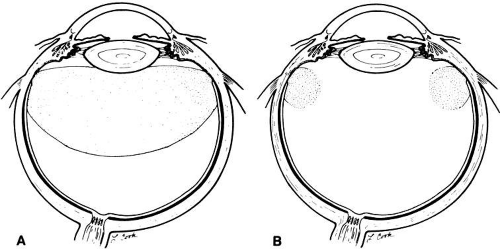 Fig. 13. A. Vitreous hemorrhage with complete posterior vitreous detachment. B. The central vitreous has been removed. |
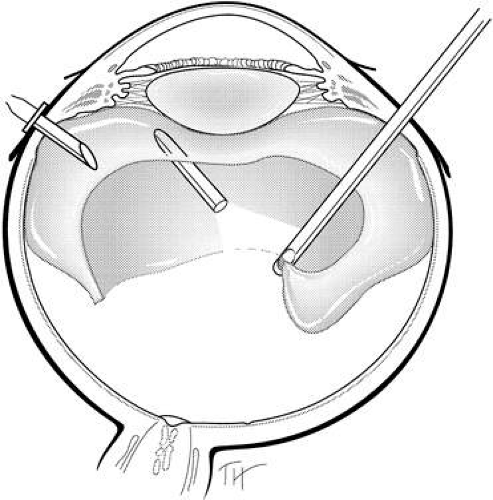 Fig. 14. The vitrector is on the edge of the posterior hyaloid in an eye with a complete posterior vitreous detachment. |
Once the media are cleared and anteroposterior traction has been removed, attention can be turned to the specifics of the case. After the case is completed, the sclerotomy sites should be closed temporarily and the periphery inspected for any breaks or detachments. Regardless of the indication for surgery, inspection should be performed before any gas or air injection in the eye as small breaks may be missed under partial or complete air- or gas-filled eyes. The sclerotomy sites also should be inspected carefully for any retinal or vitreous incarceration. The sclerotomy sites are closed with 7-0 polyglactin (Vicryl) sutures in a figure-eight configuration. The IOP should be checked. If the eye is soft, BSS can be injected at the pars plana or limbus to repressurize the eye. The conjunctiva is closed with 8-0 Vicryl sutures. Subconjunctival injections of a steroid and antibiotic are placed inferiorly, away from the rectus muscles.
SPECIAL VITRECTOMY TECHNIQUES LENSECTOMY
When an eye with a significant cataract requires a PPV, cataract extraction is essential for safe completion of the surgical objectives, especially if membranes must be peeled or delaminated from the retina. It has become increasingly common to perform phacoemulsification with implantation of a posterior chamber IOL via an anterior segment approach and PPV at the same operation.31,32,33,34,35,36,37,38 This technique avoids aphakia, which requires a contact lens or a second operation to implant a lens. In addition, aphakic diabetic eyes have a higher rate of postoperative neovascular glaucoma (NVG).81
If a pars plana lensectomy needs to be performed, the MVR blade is passed through the superotemporal sclerotomy site and into the lens at the lens equator. This creates an opening for the phacofragmotome (Fig. 17) or vitrector. A bent 21-gauge needle is connected to a separate infusion line and inserted into the lens via the superonasal sclerotomy. The infusion fluid keeps the capsular bag distended so that the lens can be removed with capsular preservation. This also prevents lens fragments from falling posteriorly. The central nucleus is removed first with the phacofragmotome, and the residual cortical material can be aspirated with the vitrector (Fig. 18). In some cases, such as anterior PVR, the capsule needs to be removed entirely. The central capsule can be removed with the vitrector and residual elements stripped with a forceps.82
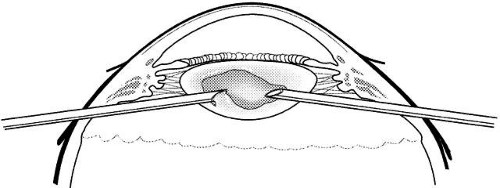 Fig. 18. The phacofragmotome (left) removes the central nucleus, and the 21-gauge needle (right) provides infusion. |
Vitrectomy techniques have been shown to be helpful in removing spontaneously dislocated lenses, in removing nuclei and cortex dislocated during cataract surgery (Fig. 19), and in retrieving and positioning posteriorly dislocated IOLs.83,84 If the nucleus is mildly sclerotic, a vitrectomy instrument, introduced through the pars plana, removes the fragments easily. Sometimes, a second instrument, such as a bent needle, is helpful. Firm pieces of nucleus can be crushed between it and the vitrectomy instrument. Dislocated nuclei with moderate or advanced sclerosis are best removed by holding them with a light pick and phacofragmenting them in the vitreous cavity (Fig. 20). The introduction of PFCLs in vitrectomy surgery had enabled the surgeon to inject this heavier-than-water liquid into the eye after vitrectomy to float the lens particles or IOL off the retina.85,86 The PFCL allows removal of the posteriorly dislocated lens or IOL with minimal retinal trauma and is especially useful when there also is a retinal detachment present.
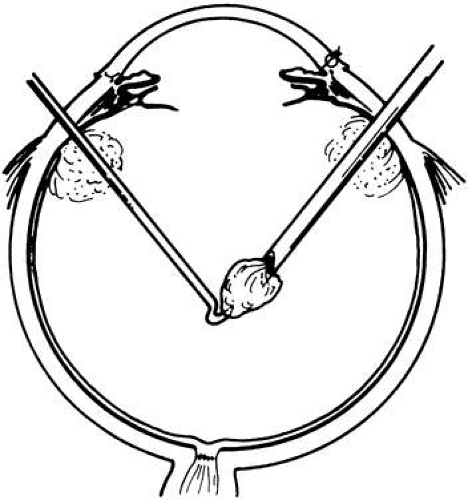 Fig. 20. After the vitreous has been removed, the nucleus is held by a bent needle and phacofragmented in the vitreous cavity. |
MEMBRANE PEELING, DELAMINATION, AND SEGMENTING
After the media have been cleared and the anteroposterior traction removed, the tangential traction on the retina must be addressed. Preretinal membranes can be seen in a host of conditions, such as proliferative diabetic retinopathy (PDR), idiopathic macular pucker, and PVR. The preretinal membranes can be vascular or avascular. There are multiple cell types involved, including glial cells, fibrocytes, retinal pigment epithelial cells, hyalocytes, and inflammatory cells. Membrane peeling, delamination, and segmentation are the three basic techniques to address preretinal membranes.
Membrane peeling is the removal of a preretinal membrane with tangential and perpendicular force (Fig. 21). The membrane peeling can be performed with a pick or forceps (Fig. 22). Illuminating light picks allow a bimanual removal approach.8 With some membranes, an edge can be initially grasped with forceps and gently peeled from the retina. In other cases, an edge must be created with a pick, MVR blade, or soft-tipped extrusion needle.87 A new tool for membrane peeling is the Tano scraper, which is a diamond-dusted silicone tip cannula that grasps membranes and facilitates removal. In cases of anterior membranes, scleral depression or a wide-field viewing system adds in visualization of the membranes. Currently, ILM peeling is being performed in macular hole surgery. The technique is similar to that of preretinal membrane peeling, but an edge in the ILM is created with a sharp MVR blade and an ILM maculorhexis performed with fine forceps or the Tano scraper.88
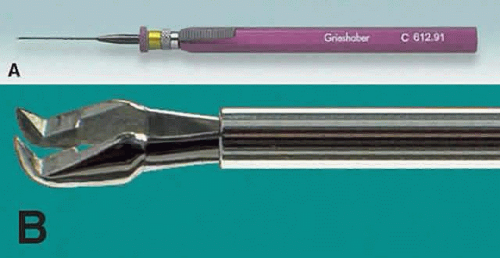 Fig. 22. A. Sutherland De Juan forceps. B. Tips of vitreoretinal forceps. (Courtesy of Alcon, Fort Worth, TX.) |
PVR occurs in 5% of all retinal detachments when retinal pigment epithelial cells, glial cells, or bothproliferate on both surfaces of the retina and on vitreous membranes. Signs of PVR include fixed folds, detachment of the nonpigmented epithelium of the pars plana, and equatorial folds. Preretinal and subretinal membranes cause shortening of the retina (Fig. 23). If a higher scleral buckle does not close the retinal breaks, release of traction is essential for reattachment. The first step is to search carefully for any open retinal breaks. In recurrent retinal detachment, look at the original break or breaks first. In reoperations for PVR, breaks on the posterior slope of a previously placed buckle at the edge of a cryotherapy scar account for 40% of all new or previously identified breaks.89 The vitrectomy instrument is used to remove as much formed vitreous as is safely possible and to cut transvitreous membranes, releasing vitreous traction. Bent needles or forceps are used to peel preretinal membranes from the retinal surface to restore retinal flexibility (Fig. 24).
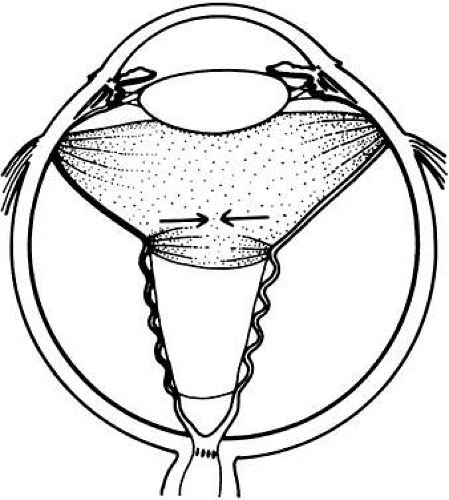 Fig. 23. Retinal detachment with proliferative vitreoretinopathy. Transvitreous traction pulls the retina toward the center of the eye. Preretinal membranes shorten the retina. |
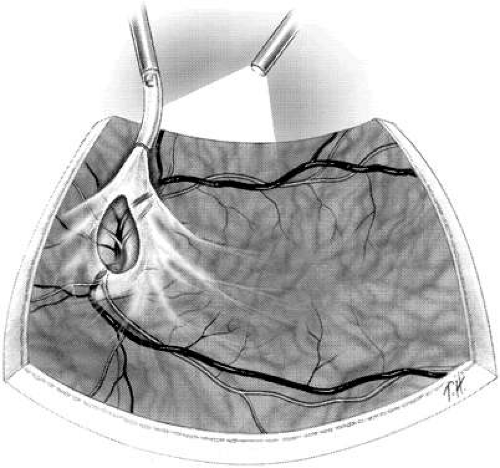
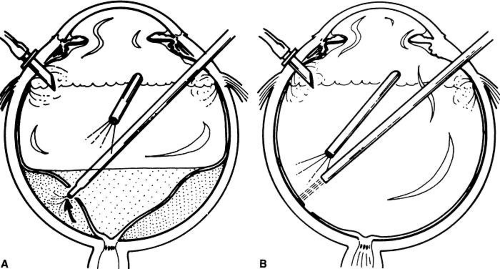
Membrane delamination usually is a bimanual technique for vascularized membranes such as in PDR. Using an illuminating pick to elevate the vascularized membrane, adhesions between the fibrovascular tissue and retina are cut with horizontal scissors (Fig. 25). Fibrovascular membranes often are extremely adherent to the retina and may overlay thin, ischemic retina. If a retina break is created in membrane removal, all traction must be removed completely from the retina. Viscodelamination, which is the use of a viscoelastic solution to create a cleavage plane between the membrane and retina, may assist in delamination.90,91 The delamination technique is used for en bloc resection of membranes.92,93,94,95 With the en bloc technique, the posterior hyaloid is left intact after a core vitrectomy. The hyaloid provides counter-traction to the membranes being delaminated. The delaminated membranes and posterior hyaloid are then removed as a single unit (en bloc).
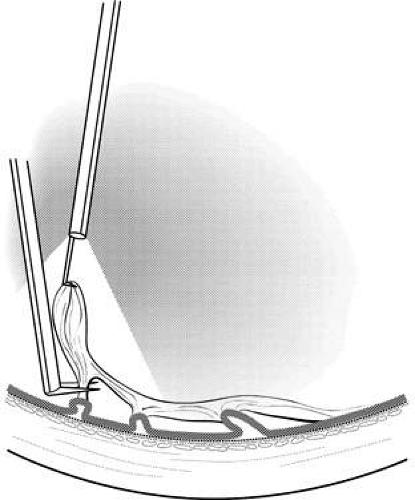 Fig. 25. An illuminated pick elevates the fibrovascular membrane as the horizontal scissors cuts the adhesions between the retina and the fibrovascular membrane. |
Membrane segmentation is used to relieve tangential retinal traction by cutting membranes, which are interconnected and producing retinal traction (Fig. 26). This technique does not involve the removal of membranes but after segmentation, membrane peeling and delamination may be easier to perform. Segmentation usually is performed with vertical scissors, which can be automated or manual (Fig. 27). To prevent intraoperative bleeding, fibrovascular membranes should be treated with diathermy before they are cut. If vessels are cut inadvertently, they should be diathermized promptly after occluding them by raising the IOP.
RETINOTOMY AND RETINECTOMY
A retinotomy is a full-thickness incision in the retina. The size, location, and indications for a retinotomy are variable. Drainage of subretinal fluid in vitrectomy for retinal detachments is one of the most common reasons for a retinotomy.96 A full-thickness retinal hole is made with an endodia-thermy probe in a detached retina. If possible, the retinotomy is positioned superiorly so that it is supported by intraocular gas longer and nasal to the optic head to avoid macula involvement if there is a hemorrhagic complication. A tapered extrusion cannula is inserted through the retinal hole to extrude subretinal fluid with a complete fluid-air exchange (Fig. 28). Endolaser is applied to the borders of the retinotomy after the subretinal fluid is removed.
Retinotomies also can be made to access thesubretinal space for removal of lesions such as fibrous bands,97 infectious organisms,98,99 subretinal hemorrhage,100,101,102,103 and choroidal neovascular membranes (CNVs).104,105,106 These access retinotomies are made with a bent MVR blade or a 36-gauge retinal pick in attached retina. In 1991, Thomas and Kaplan107 performed surgical excision successfully for CNV associated with presumed ocular histoplasmosis syndrome (POHS). The surgical technique involves PPV and removal of the posterior hyaloid. A small retinotomy is created with a bent MVR blade, and a small gauge (33- to 41-gauge) needle is used to infuse BSS under the retina. A submacular pick or spatula is then used to break adhesions around the membrane. The membrane is grasped with submacular forceps and extracted through the retinotomy. Large membranes fit through small retinotomies. An air-fluid exchange is then performed (Fig. 29). Small macular access retinotomies in such settings do not need to be sealed with laser.
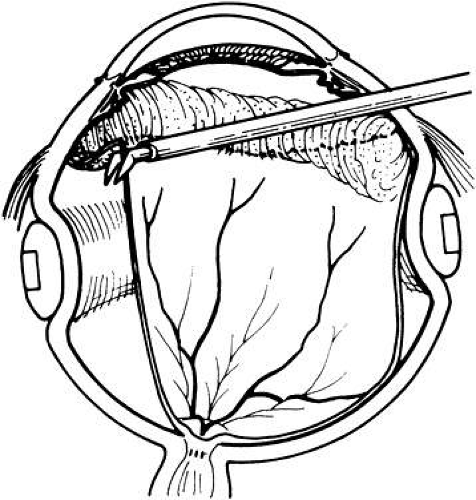
A relaxing retinotomy is made to release retinal traction.108 It is made only after all attempts to remove retinal traction by membrane peeling have failed to mobilize the retina.109 The most common indication for a relaxing retinotomy is PVR, particularly anterior PVR.110,111,112 In the Silicone Study, 29% of all eyes underwent a relaxing retinotomy.113 In anterior PVR, the vitreous in the area of the vitreous base becomes adherent to the iris or ciliary body, pulling the detached retina anteriorly. Treatment requires meticulous removal of the connections between the retina and the anterior structures (Fig. 30). Occasionally, the retina is so shortened that even with these procedures, it does not flatten, requiring the surgeon to make large incisions in the retina (relaxing retinotomies) so that it can be approximated to the retinal pigment epithelium. Endodiathermy is applied to the area of the retina that needs to be incised. The incision should be as far anterior as possible, circumferential, and involve the entire length of contracted retina. The incision can be made with the vitrector or intraocular scissors (Fig. 31). The retina anterior to the incision should be removed with the vitrector. With the advent of PFCLs, the surgical approach is to remove the posterior membranes and instill PFCL. The PFCL tamponades the posterior retina so that anterior membrane dissection and retinotomy can proceed without a mobile, bullous retina in the surgical field. The edge of the relaxing retinotomy should be treated with laser (Fig. 32).
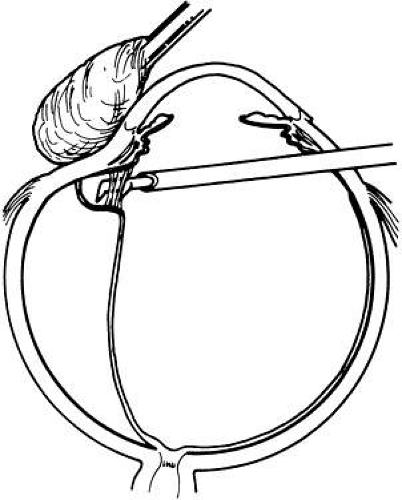 Fig. 30. To cut the traction on the vitreous base in anterior proliferative vitreoretinopathy, the eye is indented with a cotton-tipped applicator. |
Retinectomy is the excision of retinal tissue. The retina anterior to a retinotomy or giant retinal tear should be excised to remove a potential scaffold for future PVR. The flap of a horseshoe tear also should be excised to remove all anteroposterior vitreoretinal traction so the hole does not extend anteriorly after surgery. Focal retinal incarceration at a sclerotomy site or from trauma may sometimes require a retinectomy.114
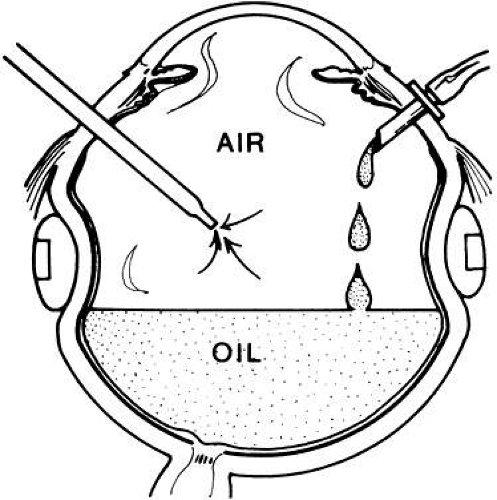
AIR-FLUID AND AIR-GAS EXCHANGE
An air-fluid exchange is used to remove subretinal fluid and provide internal retinal tamponade.115 Charles116 first performed this technique manually. Now, the surgeon removes the intraocular fluid with an extrusion cannula as an automated pump forces air through the infusion cannula.117,118,119 By following the air-fluid meniscus posteriorly, the fluid can be replaced entirely by air. If there is subretinal fluid, it is removed by placing the extrusion cannula through a posterior retinal break or retinotomy (see Fig. 28).120 As mentioned above, if the patient is pseudophakic or phakic, a Machemer lens or wide-field viewing system must be used to operate in an air- or gas-filled eye. With an aphakic eye, the surgeon can use no lens or a planoconcave lens. If the view is limited from corneal folds, sodium hyaluronate in the anterior chamber may facilitate the air-fluid exchange.121 An air-gas exchange or air-silicone exchange can be performed after the air-fluid exchange (Fig. 33).
LASER PHOTOCOAGULATION
The introduction of a system that delivers laser photocoagulation through the indirect ophthalmoscope122 has been a major advance in the treatment of retinal breaks (Fig. 34). More important, it decreases the need for extensive cryotherapy. There is some evidence from animal research that cryotherapy releases viable retinal pigment epithelial cells from Bruch’s membrane.123,124 Scleral indentation after cryotherapy facilitates this release. It is postulated that these cells later undergo metaplasia, transforming themselves into fibroblasts that contribute to PVR.125 The laser-indirect ophthalmoscope allows treatment of even the most anterior breaks after the retina has been flattened by air-fluid exchange. Thus, a thermal adhesion is obtained without release of pigment epithelial cells into the vitreous.
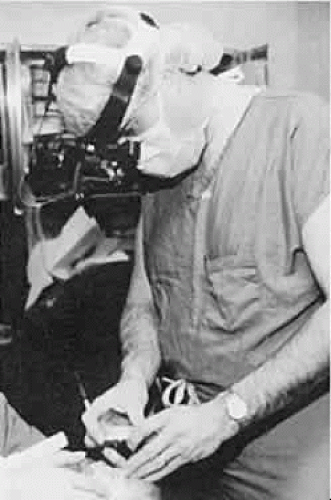 Fig. 34. The laser indirect ophthalmoscope, which is used to treat a neonate who has retinopathy of prematurity. (Courtesy of J. Arch McNamara, Wills Eye Hospital, Philadelphia.) |
Another major benefit of the laser indirect ophthalmoscope is that it can be used to treat breaks that cannot be treated with cryotherapy, such as breaks that lie over choroidal detachments or over previously placed scleral buckles. Finally, this instrument permits postoperative treatment of breaks through a gas bubble. The patient is simply positioned to move the breaks away from the bubble, allowing treatment.
Laser photocoagulation also can be delivered through an endoprobe.126 This technique allows precise placement of laser burns such as around a retinotomy site. In addition, particularly with the wide-field viewing systems, endophotocoagulation is an excellent means to apply PRP.
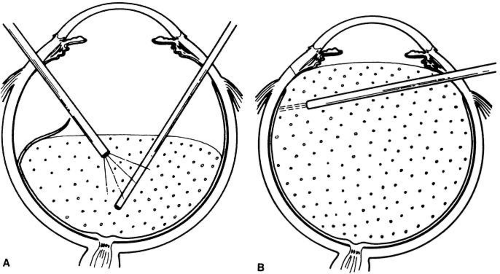
VITREOUS SUBSTITUTES PERFLUOROCARBON LIQUIDS
Perfluorocarbon liquids are transparent heavier-than-water compounds that have a low viscosity and immiscibility with water, SO, and blood.15,127,128 These characteristics make them ideal for removing subretinal fluid. Injected slowly over the optic disc, they force the subretinal fluid out through the anterior break (Fig. 35). This works nicely, even incases in which the break causing the detachmentcannot be found. Funnel retinal detachments can beopened with perfluorocarbons because of their large tamponade force. They also can be used as a “third hand” to stabilize the retina during epiretinal membrane removal. It must be mentioned, however, that if significant traction remains, the perfluorocarbon can pass into the subretinal space from where it can be removed only with difficulty. When the retina is flat, all breaks are treated with the endolaser or the laser-indirect ophthalmoscope. The perfluorocarbon liquid is then removed by an air-fluid exchange. Perfluoro-n-octane (Perfluoron) and perfluoroper-hydrophenanthrene (Vitreon) are two commonly used PFCLs. Studies suggest that Perfluoron is easier to remove and retained less than Vitreon.129,130
GASES
Intraocular air was first used as an intravitreous tamponade in 1938.131 Since then, air and inert gases such as sulfur hexafluoride (SF6) and perfluoropropane (C3F8) have been used for intraocular tamponade.132,133 The surface tension between the gas bubble and the aqueous interface allows the tamponade of retinal breaks.134 An air-fluid exchange, as described above, is performed. Intraocular air does not remain in the vitreous cavity long enough to provide an effective tamponade. Therefore, an air-gas exchange is performed for a long-acting retinal tamponade. This tamponade keeps the retina flat until cryotherapy or laser scars are firm. To perform the air-gas exchange, a mixture of gas and air is drawn up into a 50-ml syringe. The surgeon must be careful to use a nonexpansile mixture because expansile mixtures can raise the IOP high enough to close the central retinal artery. For SF6, this is 18% to 20%. For C3F8, this is 12% to 15%. In phakic eyes, the half-life of SF6 is 2.8 days and that of C3F8 is 5.7 days. The half-life for both is less in aphakic eyes than it is in phakic eyes.135 The syringe with the air-gas mixture is attached to the infusion cannula and manually pushed into the eye. A tapered infusion cannula, held in a sclerotomy port, allows efflux of the air. Flushing with at least 25 ml of the gas mixture replaces 99% of the air.136
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree