CHAPTER 168 Vestibular and Balance Rehabilitation
Program Essentials
Vestibular exercises were first described in the early 1940s by Drs. Cooksey and Cawthorne for the treatment of surgically induced vestibulopathies. Their simple eye, head, and body movements assist in habituation and are still in use today. Modern vestibular and balance rehabilitation therapy (VBRT) programs have evolved into multidisciplinary efforts in which physicians and therapists collaborate in a team approach, frequently in association with sophisticated vestibular testing facilities. A sufficient number of prospective, controlled studies have now been conducted to demonstrate both the efficacy and cost-effectiveness of vestibular rehabilitation.1 Accordingly, this treatment has become widely available and is the primary management technique for a large proportion of patients with complaints of imbalance and dizziness.
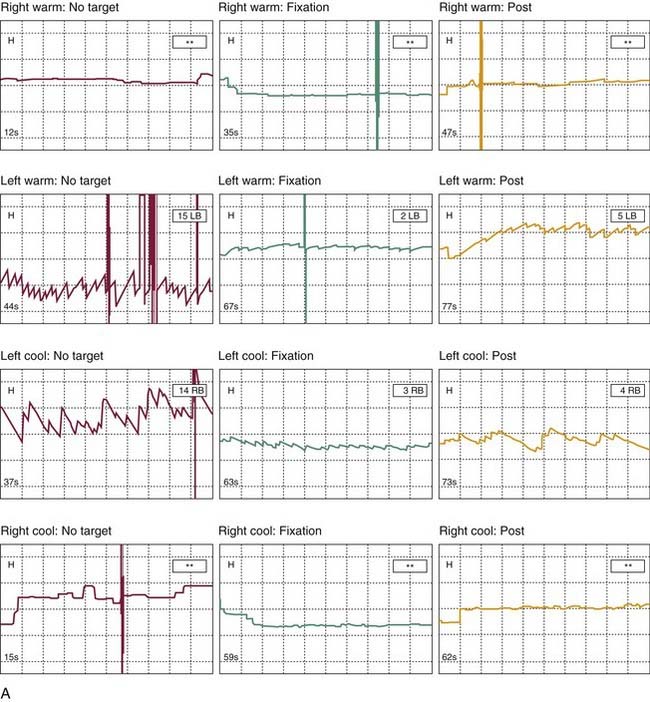
The two overall goals in a VBRT program are (1) to advance the central vestibular compensation process (Fig. 168-1), resulting in reduction in symptoms under static and dynamic conditions, and improvement in the function of the vestibulo-ocular reflex (VOR); and (2) improvement in the functionality of static and dynamic balance and gait. This second goal can be a process that is achievable independent of complete central compensation.
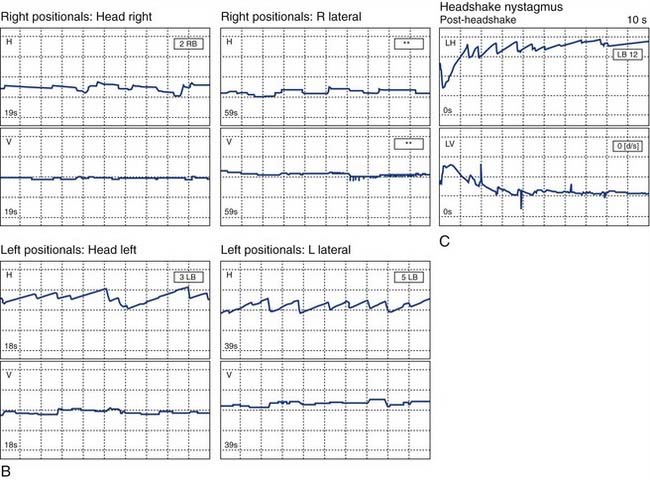
Figure 168-2. Adaptation exercises given to the patient whose videonystagmography results are shown in Figure 168-1. A, The “times 1” adaptation exercise. In the times 1 viewing, the target is held still and the patient focuses on a letter on the card and oscillates her head in a small arc in the horizontal plane as fast as she can while maintaining clear visual imaging of the target. B, Progression to a “times 2” viewing exercise. In the times 2 viewing, the task is the same, of maintaining clear visual imaging on the letter on the card; however, this time, as the head is moved to the right, the target is moved to the left, doubling the amount the eyes have to move for the same head movement shown in A.
These elements form the basis for the programs discussed in this chapter. A full, in-depth discussion of all of the aspects of a VBRT program is available in Herdman’s definitive work on vestibular rehabilitation.13
Physiologic Rationale for Vestibular and Balance Rehabilitation
A unique feature of the central nervous system is its ability to adjust to asymmetries in peripheral vestibular inputs and, to a lesser degree, to fix insults within the central vestibular pathways.14 This adjustment process is referred to as vestibular compensation and occurs naturally after most vestibular insults, provided that the affected person resumes an active lifestyle. Such adaptive plasticity requires active neuronal changes in the cerebellum and the brainstem nuclei in response to the sensory conflicts produced by central or peripheral vestibular pathology. In most instances, this process will reliably relieve vestibular symptoms, provided that the lesion is either stable or producing only gradual progressive deterioration. The underlying physiologic components of this process are the foundations of vestibular and balance rehabilitation. At least four distinct components of vestibular compensation are recognized: static compensation, which occurs regardless of movement, and three dynamic compensatory processes, adaptation, habituation, and sensory substitution, each of which is promoted by various exercise techniques targeted in VBFT.
Static Compensation for Peripheral Vestibular Lesions
Vertigo of acute onset is accompanied by nystagmus and a variety of neurovegetative symptoms, such as nausea and vomiting. This symptom complex is a result of a persistent asymmetry of vestibular input, often seen after ablative surgical procedures or with acute insults to the peripheral system. The acute or static phase of recovery is mediated by tonic rebalancing of the resting activity in the vestibular nuclei. These changes minimize side-to-side discrepancies between the tonic firing rates in the second-order neurons originating in the nuclei and occur without the need of head movement or vision.14–18 This activity generally provides relief from the most intense symptoms of vertigo and vomiting within 24 to 72 hours. Nevertheless, the patient continues to experience considerable dysequilibrium, because the system is unable to respond appropriately to the dynamic aspects of vestibular input produced by normal head movements. Thus, even after the intense vertigo has been controlled, continued motion-provoked vertigo is common until dynamic compensation is achieved.
Dynamic Compensation
To eliminate persisting dysequilibrium and residual motion-provoked vertigo after a vestibular lesion, the system must adjust to produce accurate responses to head movements. The dynamic compensation phase seems to be accomplished by reorganization of brainstem and cerebellar pathways, without modulating the neural input to the vestibular nuclei from the peripheral system.14 This process is much slower than static compensation and typically requires reprogramming of eye movements and postural control responses to head movements. The necessary reprogramming is accomplished by exposure to stimuli that challenge both the gaze stabilization and postural control systems. Because of the brainstem commissural pathways connecting the vestibular nuclei, appropriate central vestibular responses can be produced from inputs arriving from one functioning labyrinth. This feature of the compensation process is critical to recovery after extensive pathologic insults or ablative vestibular surgery, such as labyrinthectomy or vestibular nerve section. As discussed next, three major areas are active in the process of dynamic compensation: adaptation, habituation, and sensory substitution.
Adaptation is the neurologic mechanism that allows for long-term changes in the neuronal response to head movement-provoked gaze stabilization. The neural signals that induce the adaptation are generated primarily by “retinal slip” of the visual image on the retina. This phenomenon is generated by a disordered VOR response, when a head movement produces a perceived motion of a stable object in the visual environment. The resulting error signal can lead to fairly prompt and long-term changes in the functional performance of the VOR.4 This process of adaptation produced by retinal slip seems to be context-dependent, so that specific adjustments must be made for movements of different frequency, directions of head movement, eye position in the orbit, and distances from the visual target.3,19 The complexity of the adaptation process helps explain why residual symptoms are almost unavoidable even in a fairly well-compensated patient. Postural stability also is improved by reducing abnormal visual influences on postural control mechanisms secondary to retinal slip.
Habituation is the long-term reduction of a response to a noxious stimulus resulting from repeated exposure to the stimulus.20 This phenomenon seems to be context-dependent and does not generalize well from one head movement to another. This mechanism is essential for a variety of conditions that can produce sensitivity to head movement or motion in the visual surroundings. Although peripheral asymmetry is one common cause of these symptoms, other common causes are central lesions, anxiety disorders, and migraine disorders.5 Although the adjustments produced by habituation are made fairly quickly and are reasonably accurate, the central system requires consistency in the inputs to use them properly for habituation. For this reason, it is essentially impossible to “compensate” for an unstable vestibular lesion such as Meniere’s disease.
The primary goals of both adaptation and habituation are to produce gaze stability and postural stability in both static and dynamic situations. The response frequency ranges for gaze and postural stability are very different. To achieve gaze stability, the responsible mechanisms must function properly in a range from static position (no motion) up to movements that correlate with head motions as quick as 10 Hz. Postural stability is predominantly a task that requires responsiveness only below 4 Hz.21,22
In addition to adaptation and habituation, another critical component of dynamic compensation involves sensory substitution. This process requires the adoption of alternate strategies for gaze and postural control, in order to replace the compromised sensory function. For example, the patient with bilateral loss of peripheral vestibular function becomes dependent primarily on visual or proprioceptive inputs to maintain postural stability. Although these mechanisms may need to be fostered in a therapeutic setting, many patients will have developed some of these out of necessity before coming for evaluation. Although sensory substitution may be helpful, it may be maladaptive in some environmental settings. For example, a patient may be overly dependent on vision and therefore cannot use proprioceptive and residual vestibular inputs to successfully navigate in darkness. In addition to the common substitution of visual and proprioceptive inputs, some of the other mechanisms that may be invoked in the setting of vestibular loss include (1) activation of the cervico-ocular reflex, which is not particularly active in healthy persons10; (2) use of the smooth pursuit tracking system11; and (3) use of anticipatory or corrective saccades. Patients with both unilateral and bilateral vestibular deficits use corrective saccades to adjust for the reduction of VOR-induced eye movements after head movement. With central preprogramming through exposure to specific eye-head coordinated movements, these eye movements can be applied automatically to help maintain gaze stability when the VOR is deficient.7,8
Research findings suggest that initial central vestibular compensation for a peripheral lesion can be enhanced by head movement but is delayed by inactivity.23–26 It also is hampered by central vestibular dysfunction of any cause.27 Medications that typically are used for acute symptoms of vertigo, such as meclizine, scopolamine, and benzodiazepines, all cause sedation and central nervous system depression. Although they may provide helpful symptomatic relief during the initial stages of an acute labyrinthine crisis, their effects are potentially counterproductive with respect to vestibular compensation, especially with use over extended periods.24,28 In addition, chronic anxiety or other psychiatric disorders may delay or disrupt the compensation process.29,30
Assessment of Vestibular Compensation
Role of the Clinical History
A complete neuro-otologic history probably is the single most important component of the diagnostic evaluation of the patient with a balance disorder. Balance function study results must be interpreted in light of the presenting symptoms and medical history.31 In general, the information sought should include the onset of symptoms and their characteristics at that time, the progression of symptoms over time, the nature and duration of typical spells, any predisposing factors in the medical history, and use of medications or other management strategies. Complicating features of anxiety, depression, or excessive dependence on medications should be addressed. Some effort should be extended to identify the degree of disability produced by the patient’s vestibular complaints with respect to his or her professional and social activities. The stability and commitment of the patient’s psychological support system also should be assessed.
Role of Vestibular Testing
The most traditional purpose of balance function studies is site-of-lesion localization addressing the sensory inputs, motor output elements, and neural pathways that may be involved in producing the reported symptoms. Balance function studies also may assess the patient’s functional ability to use sensory input systems in an integrated fashion, as in maintenance of stance before and after induced sway and coordination of head and eye movements during gaze activities. The third assessment goal is to evaluate, in a limited manner, the current degree of physiologic and functional compensation.32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree