CHAPTER 187 Velopharyngeal Dysfunction
Functional Anatomy
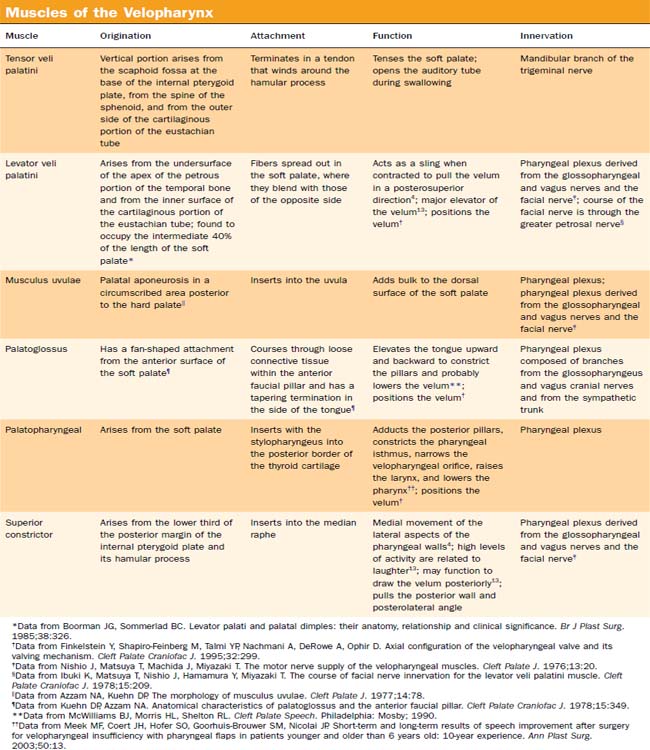
The velopharyngeal port closes as the velum moves in a posterior-to-superior direction. The lateral pharyngeal walls may move medially. Occasionally, anterior movement of the posterior wall will be seen. The muscles of the velopharynx contribute to this closure (Table 187-1).
The elevation and posterior motion of the velum are attributed to the levator veli palatini (LVP). This is the main muscle mass of the velum.1 Variation in the angle of insertion to the base of skull may change the elevation.2 The palatoglossus and palatopharyngeus muscles pull the palate down, opposing the LVP. The palatopharyngeus muscle pull tends to stretch the velum laterally, thereby increasing the velar area and altering the shape of the contact.2 This muscle can make subtle changes to velar height, especially when the velum is in the elevated position.3 The musculus uvulae adds bulk to the dorsal side of the velum.
Lateral wall motion varies from person to person and depends on speech context. The greatest movement usually is below the levator eminence at the level of the full length of the velum and hard palate.4 This movement is attributed to selective movement of the uppermost fibers of the superior constrictor. Because of the relationship between the lateral fibers of the superior constrictor and the palatopharyngeus, it has been suggested that this muscle is involved in the lateral wall motion as well.5
Passavant’s ridge is a posterior wall feature seen in some persons during speech or swallow. It has been associated with lateral wall motion and is thought to be caused by a similar movement of the uppermost fibers of the superior constrictor and palatopharyngeus.6 It may be involved in velopharyngeal closure in as many as one third of patients in whom Passavant’s ridge is observed.7,8 Its movement also can be seen below the level of the velopharyngeal port and therefore does not assist in the closure.
Causes of Velopharyngeal Dysfunction
Velopharyngeal dysfunction refers to abnormal function of the velopharyngeal sphincter mechanism. However, it does not identify the cause. Perceptually, this dysfunction is considered a dysphonia because it affects the sound quality of the voice. The cause of the dysphonia needs to be identified. Campbell and associates9 reported on 427 children referred to a pediatric voice and resonance clinic for voice problems. Of those children, 16% were actually found to have velopharyngeal, rather than laryngeal dysfunction. Different terminology has been used to describe the causes of VPD, and relevant terms and concepts are used inconsistently throughout the medical literature. In this chapter, we use the definitions summarized by D’Antonio and Crockett.10 Velopharyngeal inadequacy refers to any type of VPD and can be divided into three etiologic categories: insufficiency, incompetence, and mislearning. Velopharyngeal insufficiency encompasses structural defects that result in insufficient tissue to accomplish closure—a well-known example being cleft palate. Incompetence describes impairment of motor control secondary to neurologic dysfunction, such as paresis or paralysis. Causes of incompetence include the sequelae of skull base surgery and tumors around the jugular foramen and vagus nerve, or central nervous system (CNS) impairment from brainstem stroke. Mislearning is the result of etiologic factors that are independent of structural defects or neuromotor pathology.
Congenital anatomic conditions affecting velopharyngeal function most commonly are attributable to clefting of the palate. VPD in the absence of an overt cleft palate also occurs. Affected children may have other anatomic abnormalities or functional disorders causing velopharyngeal insufficiency. These include congenital short palate, palatopharyngeal disproportion, a less overt palate deficiency called occult submucous cleft palate (absence of the musculus uvulae), and longitudinally oriented levators. Hypertrophic tonsils occasionally can cause insufficiency by impeding palate closure. Neurogenic causes of velopharyngeal incompetence include muscular dystrophies, myasthenia gravis, traumatic brain injury, Down syndrome, and velocardiofacial syndrome (22q11 deletion). An adenoidectomy can create or unmask VPD in any of these settings. In velopharyngeal insufficiency, a large adenoid can compensate for a short palate. In velopharyngeal incompetence, adenoidectomy can compensate for a poorly mobile palate. With removal of the adenoidal tissue, the mechanism of compensation is eliminated. Velopharyngeal inadequacy has been reported to occur after 1 in 1500 adenoidectomies.11,12
Assessment
Perceptual Speech Analysis
Hyponasal resonance is most noted in the sounds /m/, /n/, and /ng/. These nasalized consonants will be altered with decreased nasal airflow. The /m/ will be changed to sound like /b/, the /n/ changed to sound like /d/, and the /ng/ to a hard /g/. Humming the /m/ sound will not change with nose plugging if the nose is already occluded. In addition, the examiner will not feel nasal vibrations. Normally, a mirror held under the nose should fog with voicing of the nasal consonants (Fig. 187-1). If the voice quality is the same with or without occlusion of the nose, then nasal or nasopharyngeal obstruction is present. Hyponasal resonance can be described as that quality of speech associated with the congestion of a common cold. Large adenoids or congested nasal turbinates also may be seen. Repetition of words or sentences that are loaded with nasal consonants will aid in documentation of this abnormality (Table 187-2). The velopharynx continues to be active during production of words and phrases with nasal consonant sounds but will be between a relaxed and a closed state.
Table 187-2 Examples of Tasks to Evaluate
| Nasal Consonants | |
| Ma ma | Money |
| Na na | Monkey |
| Momma made lemon jam | Nancy is a nurse |
Hypernasality or increased nasal resonance will be noted with production of non-nasal phonemes (Table 187-3). Because most sounds (vowels and consonants) in the English language are non-nasal, there are many phonemes to work with. The early phonologic repertoire usually includes the bilabial plosives /p, b/ and lingua-alveolar phonemes /t, d/. Using phonemes—words and sentences loaded with these sounds—allows the listener to assess speech resonance (normal or hypernasal). Plugging the nose while the child repeats the /p, b, t, d/ sounds or during sustained production of /s/ or /sh/ will result in noticeable change in resonance if there is hypernasality on these sounds. The use of a mirror beneath the nose during speech tasks also will assist in the detection of the nasal air escape (see Fig. 187-1). Fogging of the mirror typically is observed only for production of nasals and nasalized vowels. Increasing the complexity of the tasks (i.e., sounds to words to phrases to sentences) may document deterioration of the velopharyngeal competence. The degree of openness is determined by the phonetic environment. Some children will do less well if nasal and non-nasal phonemes are mixed. Repetition of tasks during a period of minutes may unmask velopharyngeal fatigue, as seen in myasthenia gravis. Velar height or elevation is most pronounced during the “high” vowels of /i/ and /u/13 and the fricative /s/.14 Even if velopharyngeal function is improving, production of these sounds may remain difficult.
Table 187-3 Examples of Tasks to Evaluate
| Non-Nasal Consonants | ||
| Pa pa pa | Daddy did it | Sustain “s” |
| Baby | Too tight | Sustain “sh” |
| Puppy | Go get an egg | Count from “sixty to seventy” |
| Puffy | Forty-four fat fish | Baby bib |
| Daddy | Sissy saw it | Get it out |
The clinician also may encounter “phoneme-specific” VPD, or mislearning. In this entity, one or more phonemes are produced abnormally with increased resonance, while the rest of the speech is normal.15 It most often is noted with production of /s/, /sh/, /z/, and rarely, /f/ phonemes. A nasal fricative substitution is characteristic. Because these are predominant sounds in the English language, the patient often is believed to be globally hypernasal. Because other non-nasal sounds demonstrate no air escape, however, the velopharynx should be recognized to be otherwise functional. Appropriate articulation therapy usually will correct this abnormality.
The diagnosis of hypernasality may be confounded by concomitant dysphonia or hyponasality. Hoarseness will distort the sound enough that mild VPD may be overlooked. More than 40% of children with VPD also have dysphonia.16 The use of the mirror test helps separate VPD from laryngeal pathology.
The presence of velopharyngeal insufficiency has a significant impact on the child’s and the family’s quality of life. Emotional and communication aspects are primarily affected. Parents seem to be an appropriate proxy in determining the impact of the altered speech on the child’s quality of life.17
Nasometry
Nasometry is an objective standardized assessment that measures the ratio of sound intensity between the nose and the mouth. This typically is done with voicing of standard phrases and passages. Standardized values exist for specific tasks. Calculation of the number of standard deviations from normative values for each phonemic set yields a measure of the severity of the resonance pattern. Nasometry can be used in the initial evaluation to document the degree of dysfunction. Perhaps more important, it is used in assessing progress during speech therapy or in following other interventions.18 A discrepancy may exist between nasal scores and the perceived degree of hypernasality.19 Figure 187-2 shows the Kay Elemetrics headgear used for this test.
Pressure Flow
Pressure and airflow measurement is another method of assessing velopharyngeal function during speech.20–22 The nose is covered with a small mask to permit accurate measurement of nasal airflow. A probe is placed into the mouth to measure oral pressure. In the child with normal velopharyngeal function, no airflow will be detected during production of non-nasal phonemes. Oral pressure will be present if nasal air escape is detected during non-nasal sounds. An advantage to the pressure-flow technique is the ability to determine the timing of the air escape.14 The pressure-flow technique also is used to calculate the cross-sectional nasopharyngeal airway area from the pressure-flow measures.
Imaging Studies
An imaging study of the velopharyngeal mechanism is indicated when speech therapy is not progressing, if speech evaluation reveals significant hypernasality, if a diagnostic dilemma is present, or when surgery is under consideration. Lateral cephalometric x-ray studies were done in the past but are limited by a sagittal plane view and do not provide information on dynamic movement of the velopharyngeal mechanism. Current methods of imaging velopharyngeal function include speech videofluoroscopy and speech nasal endoscopy. Endoscopy has largely supplanted videofluoroscopy in most clinics today. Children older than 3 years of age most often will cooperate with the evaluation. The speech nasal examination may not be useful, however, in the child with significant developmental delays. If the child cannot produce appropriately articulated phonemes, the study will not give adequate speech information. The accuracy of articulation has a direct effect on the closure.23 Velopharyngeal closure on swallow does not yield information regarding speech.6 To be of value, the assessment requires appropriate articulation of phonemes.
Speech Videofluoroscopy
Videofluoroscopic evaluation has been a standard tool in assessment of the speech mechanism.24 Generally, a speech-language pathologist attends this examination with a radiologist in the hospital imaging department, as is done for modified barium swallow studies. A small amount of barium is introduced through the nose to coat the velopharynx and improve visualization. While under fluoroscopy, the child repeats or reads a set of phoneme-specific speech tasks. Because the velopharyngeal sphincter functions in several planes of movement, accurate analysis will require at least two and preferably three views. The lateral view demonstrates the length, thickness, anterior-posterior, and superior motion of the palate, as well as the anterior movements of the posterior pharyngeal wall (Passavant’s ridge). The anterior-posterior view assesses the lateral wall motion. An en face view (e.g., Towne’s or submental vertex view) will look down the velopharynx and demonstrate lateral wall, velar, and posterior wall motion.
Videofluoroscopy has some limitations. Because of the radiation exposure, the speech sample may need to be shortened. Cooperation of the patient is still needed. Interpretation of the radiographs requires experience with analysis of the images. The examining team must include both a radiologist and a speech therapist with experience in this area of practice. With videofluoroscopy, closure patterns can be well defined and the level of Passavant’s ridge and its participation in closure can best be assessed. Nevertheless, this assessment may still miss small fistulas and intermittent closure patterns. In addition, it is difficult to evaluate postsurgical changes. Many teams are moving toward the use of endoscopy as the standard first-line assessment tool.25,26
Speech Endoscopy
Speech endoscopy is now considered the most useful tool for evaluation.27 Many otolaryngologists and some speech-language pathologists are experienced in the use of this minimally invasive diagnostic test. Ideally, the test is conducted with both the physician and speech-language pathologist in the room at the same time. If this is not possible, the examination can be video recorded for review. After topical anesthesia of the nose has been accomplished, a flexible nasopharyngoscope is introduced into the velopharynx.
The best image is obtained with the scope positioned higher in the nasopharynx to reduce parallax and fish-eye distortions. Passing the flexible scope in the middle meatus region (rather than along the floor) of the nose facilitates this optimal positioning. As with speech videofluoroscopy, a series of words, phrases, and sentences are spoken while the endoscopic images are recorded. It is important to use a microphone and record the voice, not just the video images. Endoscopy allows assessment of the static anatomy such as the nasal septum, eustachian tube orifice, adenoid pad, and structure of the musculus uvulae. Absence of the musculus uvulae is seen with occult submucous clefting (Fig. 187-3).
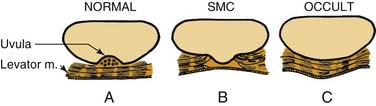
Figure 187-3. Muscle orientation of normal (A), submucous cleft (B), and occult submucous cleft (C). SMC, submucous cleft.
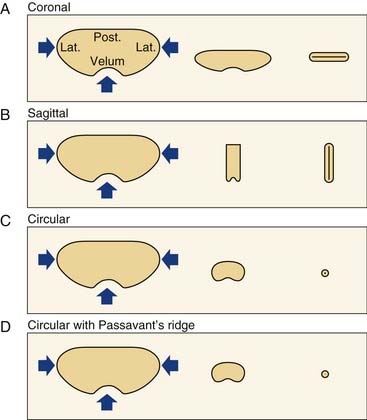
Four primary velopharyngeal closure patterns have been observed, as depicted in Figure 187-4.28 These can be seen in both endoscopy and speech videofluoroscopy. These patterns are best understood in terms of the residual gap orientation on incomplete closure of the velopharynx.
The closure pattern may assist in prescribing surgical or prosthetic intervention. Knowing where the “gap” is should allow the clinician to decide how best to obturate that gap, as discussed next.29–31