Fig. 19.1
Graphical representation of various surgical procedures. The blue area depicts the donor tissue. In a PKP the entire thickness of the central cornea is replace. In a DSEK/DSAEK the host Descemet’s membrane is removed and replaced with donor Descemet’s membrane and about 150 μm of donor stroma. In the DMEK the host endothelium is replaced with only donor endothelium
From external to internal, the cornea consists of a thin epithelial layer with its associated underlying Bowman’s layer. Deeper to the epithelium lies the cornea stroma which makes up the majority of the corneal substance. This is composed of a disparate population of keratocytes interspersed between layers of collagen. The most internal structure is a single layer of endothelium, which rests upon its basement membrane, called Descemet’s membrane. The average thickness of a human cornea is about 550 μm. Despite its small size, pathology can be limited to a single layer of the cornea. For example, Fuchs Dystrophy results in primary endothelial cell loss, which, in advanced states produces corneal edema and decreased vision. Despite the fact that the pathology is initially confined to one layer of the cornea, for many years the surgical therapy involved a full thickness penetrating keratoplasty (PKP). While largely successful, PKP can be fraught with both intraoperative and postoperative complications. The eye is a pressurized system and a rapid decrease in this pressure, as is caused by the corneal incision in PKP, can result in intraocular or suprachoroidal hemorrhage and loss if intraocular contents. Postoperatively, the success of transplantation requires intensive topical steroid use. This can result in cataract formation and glaucomatous optic neuropathy. The localized immunosuppression also puts the recipient at risk for bacterial and fungal corneal infections which can be visually devastating.
The concept of lamellar corneal transplantation, or replacing just a layer of the cornea, is not new [2]. Early attempts at corneal transplantation included lamellar surgery in animals as well as in humans. In 1838, Richard Sharp Kissam attempted to transplant the anterior portion of a pig cornea onto a human cornea without success. For decades following, surgeons struggled with keratoplasty techniques but the anterior lamellar technique remained the predominant attempted form. These techniques fell out of favor with the success of the full thickness technique in the 1900s.
It was not until 1998 when Dutch ophthalmologist, Gerrit Melles, described a technique for replacing the inner layers of the cornea that a resurgence of interest in lamellar surgery came about [3]. Never before had successful attempts been made to selectively replace damaged endothelial tissue do largely to difficulties in surgical technique. Melles’s technique involved creating a large (~9 mm) corneal scleral pocket that extended circumferentially into the clear cornea. The donor tissue was prepared in a similar fashion by hand dissecting the posterior corneal stroma to create a circular button. The donor tissue was placed into the eye and tucked into corneal pockets that had been created during the initial dissection. The technique relied upon air to aid in the dissection of the recipient bed as well as for holding the donor tissue in position. This technique was termed Posterior Lamellar Keratoplasty (PLK) [3].
Shortly after Melles’s initial description of the technique, American ophthalmologist, Mary Terry described a revision of the technique, which he termed Deep Lamellar Endothelial Keratoplasty (DLEK) [4, 5]. In this technique, the eye is filled with a viscoelastic material rather than air and then the inner ~90 μm of posterior corneal tissue is dissected from the adjacent stroma and removed from the eye. The surgeon performs a similar dissection of donor tissue and then places it within the anterior chamber through a smaller (~5 mm) incision. The graft is oriented and then air is placed below it to hold it in place against that posterior host stroma. In addition, a circular corneal pocket is dissected into which the donor tissue is tucked. This surgery preserves the natural corneal curvature and spares the patient a large incision. However, it is technically very difficult and time consuming to perform. In addition, the postoperative best corrected visual acuity is generally less than that seen with a traditional PKP [6]. The reduction in vision has been attributed to scar tissue and haze that forms at the interface between the two hand dissected tissue planes [7]. Due to its difficulty, DLEK surgery was not widely adopted by cornea surgeons throughout the world.
In 2001 Melles again made history by describing an advancement in the above technique in which there was no tedious dissection of the host stromal tissue [2, 8]. Rather, Descemet’s membrane is scrolled in the periphery and then removed from the eye. A donor lenticule consisting of endothelium, Descemet’s membrane, and about 120 μm of stroma is then placed into that anterior chamber (Figs. 19.2 and 19.3). Similar to DLEK surgery, air is placed within the eye to facilitate attachment of the donor tissue to the posterior corneal surface (Fig. 19.4). Eliminating the technically difficult dissection of the host corneal stroma results in a much easier surgical procedure as well as better visual results. In some instances, the results approach perfection and rival those obtained with PKP. This procedure was termed Descemet’s stripping endothelial keratoplasty (DSEK).
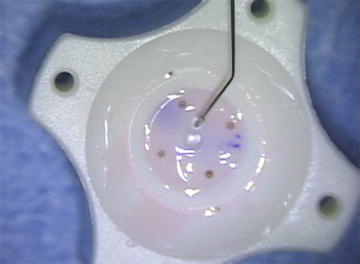
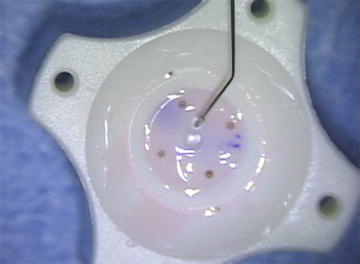
Fig. 19.2




DSAEK donor tissue after cutting with a trephine. The donor endothelium is facing up and the tissue has been inked in the periphery to aide in orientation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


