 Tumors of the Nonpigmented Ciliary Epithelium
Tumors of the Nonpigmented Ciliary EpitheliumCongenital Neoplasms (Medulloepithelioma)
Several neoplasms and related lesions can originate in the nonpigmented ciliary epithelium (NPCE). Zimmerman classified these lesions into congenital and acquired types (1). We use the following modification of Zimmerman’s classification:
Congenital
Glioneuroma
Nonteratoid medulloepithelioma (diktyoma)
Benign
Malignant
Teratoid medulloepithelioma
Benign
Malignant
Acquired
Pseudoepitheliomatous hyperplasia
Reactive
Age-related (Fuchs adenoma; coronal adenoma)
Benign epithelioma
Solid
Papillary
Pleomorphic
Malignant epithelioma
Solid
Papillary
Pleomorphic
Some, like glioneuroma, are exceedingly rare. We have only seen one case that may have met criteria for that diagnosis, but this rare tumor is not discussed here. The acquired tumors have generally been called “adenomas.” However, because they are tumors derived from neuroepithelium, we prefer to call them neuroepithelioma or, simply, epithelioma of the NPCE.
Congenital Neoplasms of the Nonpigmented Ciliary Epithelium (Intraocular Medulloepithelioma)
General Considerations
The most important congenital tumor of the NPCE is medulloepithelioma, a nonhereditary, embryonal neoplasm generally diagnosed in the first decade of life (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29). On occasion, the tumor is not recognized until adulthood (13,14,20). It arises from the medullary epithelium, or inner layer of the optic cup, prior to its differentiation into its adult derivatives. It most commonly occurs in the ciliary body, where it presumably arises from the anterior lip of the optic cup. However, medulloepithelioma has occasionally been recognized in the optic nerve (21, 22, 23, 24).
Clinical Features
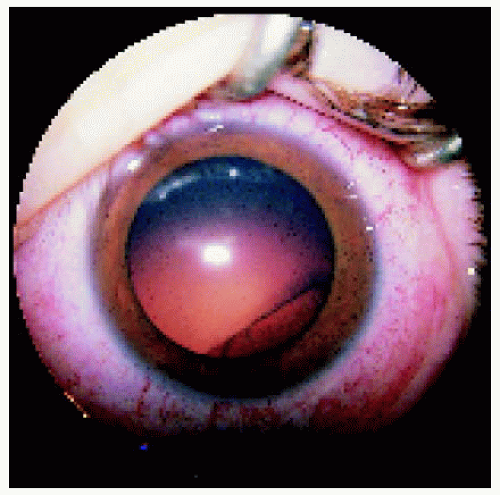
An early clinical feature is a “lens coloboma,” which is actually a notch in the lens due to congenital absence of zonule in the quadrant of the tumor. Examination of the adjacent ciliary body reveals a rather typical fleshy, pink to tan mass. Clear cysts are often present within the mass. The cysts may become a prominent part of the tumor and may even break free from the mass to float freely in the anterior chamber or vitreous cavity (3,4,27). Rarely, a medulloepithelioma may be pigmented (15,25,26).
A characteristic neoplastic cyclitic membrane can develop, sometimes suggesting the diagnosis of persistent hyperplastic primary vitreous (4,8). Secondary glaucoma occurs in 60% of cases and is most often due to iris neovascularization and secondary angle closure (4,17). Retinal detachment is a common complication. There is often a long delay in diagnosis and sometimes misdirected therapy. Patients have often undergone cataract surgery, glaucoma surgery, and vitreous surgery while the underlying tumor remained unsuspected.
Extraocular extension with orbital invasion is an uncommon complication of medulloepithelioma (3,4,10,13). Central nervous system extension has rarely been recognized. It can be fatal due to progressive intracranial growth of the neoplasm (13,27). Tumors that demonstrate extraocular extension, a very rare occurrence, can metastasize to regional lymph nodes and systemic sites.
Diagnostic Approaches
Fluorescein angiography shows early hyperfluorescence and gradual late staining of the mass. Ultrasonography reveals a mass pattern with acoustic solidity and high internal reflectivity (1,6). Areas of cartilage within the mass can produce echoes very similar to those with dystrophic calcification seen with retinoblastoma (7).
Pathology
Medulloepithelioma can be classified histopathologically into nonteratoid and teratoid types, and both can be cytologically benign or malignant. In our experience more than 80% of intraocular medulloepitheliomas are cytologically malignant. The nonteratoid type consists purely of cells that resemble ciliary epithelium and is sometimes called a diktyoma, derived from the Greek word meaning “fish net.” The teratoid type demonstrates heteroplastic elements such as cartilage, rhabdomyoblasts, and brain. Cysts found in both types contain a hyaluronidase-sensitive mucopolysaccharide, identical to vitreous, that is secreted by the tumor cells, forming secondary cysts (1, 2, 3, 4). Recurrent medulloepithelioma tends to have more malignant histopathologic features (10). Melanin granules are occasionally present in the cytoplasm, which explains why some tumors are clinically pigmented (15,25,26). Eyes with medulloepithelioma are often found to have degrees of persistence of the hyaloid system, another developmental abnormality (3,4).
Management
Although most eyes with medulloepithelioma require enucleation, a small, circumscribed medulloepithelioma can be managed by iridocyclectomy. Plaque radiotherapy is an option for localized or recurrent tumor, but its role has not been clearly defined (4,14). Because deaths have occurred only in patients with advanced extrascleral extension, orbital exenteration should be considered if there is extensive orbital involvement. The role of irradiation and chemotherapy for intraocular medulloepithelioma is not established.
Selected References
1. Zimmerman LE. The remarkable polymorphism of tumors of the ciliary epithelium. The Norman McAlister Gregg Lecture. Trans Aust Coll Ophthalmol 1970;2:114-125.
2. Shields JA, Shields CL. Tumors of the nonpigmented ciliary epithelium. In: Shields JA, Shields CL, eds. Intraocular Tumors. A Text and Atlas. Philadelphia: WB Saunders; 1992:461-487.
3. Broughton WI, Zimmerman LE. A clinicopathologic study of 56 cases of intraocular medulloepitheliomas. Am J Ophthalmol 1978;85:407-418.
4. Shields JA, Eagle RC Jr, Shields CL, et al. Congenital neoplasms of the nonpigmented ciliary epithelium (medulloepithelioma). Ophthalmology 1996;103:1998-2006.
5. Canning CR, McCartney ACE, Hungerford J. Medulloepithelioma (diktyoma). Br J Ophthalmol 1988;72:764-767.
6. Hennis HL, Saunders RA, Shields JA. Malignant teratoid medulloepithelioma of the ciliary body. J Clin Neuroophthalmol 1990;10:291-292.
7. Shields JA, Eagle RC, Shields CL, et al. Fluorescein angiography and ultrasonography of malignant intraocular medulloepithelioma. J Pediatr Ophthalmol Strabismus 1996;33:193-196.
8. Shields JA, Shields CL, Schwartz RL. Malignant teratoid medulloepithelioma of the ciliary body simulating persistent hyperplastic primary vitreous. Am J Ophthalmol 1989; 107:296-298.
9. Desai VN, Lieb WE, Donoso LA, et al. Photoreceptor cell differentiation in intraocular medulloepithelioma: an immunohistopathologic study. Arch Ophthalmol 1990;108:481-482.
10. Kivela T, Tarkkanen A. Recurrent medulloepithelioma of the ciliary body. Immunohistochemical characteristics. Ophthalmology 1988;95:1565-1575.
11. Babu N, Dey P. Medulloepithelioma of ciliary body diagnosed by fine needle aspiration cytology. Cytopathology 2003;14:93-94.
12. al-Torbak A, Abboud EB, al-Sharif A, et al. Medulloepithelioma of the ciliary body. Ind J Ophthalmol 2002;50:138-140.
13. Jumper MJ, Char DH, Howes EL Jr, et al. Neglected malignant medulloepithelioma of the eye. Orbit 1999;18:37-43.
14. Davidorf FH, Craig E, Birnbaum L, et al. Management of medulloepithelioma of the ciliary body with brachytherapy. Am J Ophthalmol 2002;133: 841-843.
15. Shields JA, Eagle RC Jr, Shields CL, et al. Pigmented medulloepithelioma of the ciliary body. Arch Ophthalmol 2002;120:207-210.
16. Lloyd WC 3rd, O’Hara M. Malignant teratoid medulloepithelioma: clinicalechographic-histopathologic correlation. JAAPOS 2001;5:395-397.
17. Singh A, Singh AD, Shields CL, et al. Iris neovascularization in children as a manifestation of underlying medulloepithelioma. J Pediatr Ophthalmol Strabismus 2001;38:224-228.
18. Lumbroso L, Desjardins L, Coue O, et al. Presumed bilateral medulloepithelioma. Arch Ophthalmol 2001;119:449-450.
19. Quiones Tapia D, Serrano de la Iglesia JM. Malignant nonteratoid medulloepithelioma. Ophthalmology 1999;106:211.
20. Husain SE, Husain N, Boniuk M, et al. Malignant nonteratoid medulloepithelioma of the ciliary body in an adult. Ophthalmology 1998;105:596-599.
21. Reese AB. Medulloepithelioma (dictyoma) of the optic nerve. Am J Ophthalmol 1957;44:4-6.
22. Green WR, Iliff WJ, Trotter RR. Malignant teratoid medulloepithelioma of the optic nerve. Arch Ophthalmol 1974;91:451-454.
23. O’Keefe M, Fulcher T, Kelly P, et al. Medulloepithelioma of the optic nerve head. Arch Ophthalmol 1997;115:1325-1327.
24. Chavez M, Mafee MF, Castillo B, et al. Medulloepithelioma of the optic nerve. J Pediatr Ophthalmol Strabismus 2004;41:48-52.
25. Pe’er J, Hidayat AA. Malignant teratoid medulloepithelioma manifesting as a black epibulbar mass with expulsive hemorrhage. Arch Ophthalmol 1984;102:1523-1527.
26. Gopal L, Babu EK, Gupta S, et al. Pigmented malignant medulloepithelioma of the ciliary body. J Pediatr Ophthalmol Strabismus 2004;41:364-366.
27. Sosinska-Mielcarek K, Senkus-Konefka E, Jaskiewicz K, et al. Intraocular malignant teratoid medulloepithelioma in an adult: clinicopathological case report and review of the literature. Acta Ophthalmol Scand 2006;84: 259-262.
28. Zhou M, Xu G, Bojanowski CM, et al. Differential diagnosis of anterior chamber cysts with ultrasound biomicroscopy: ciliary body medulloepithelioma. Acta Ophthalmol Scand 2006;84:137-139.
29. Garcia-Feijoo J, Encinas JL, Mendez-Hernandez C, et al. Medulloepithelioma of the ciliary body: ultrasonographic biomicroscopic findings. J Ultrasound Med 2005;24:247-250.
▪ Ciliary Body Medulloepithelioma: Clinical and Gross Pathologic Features
Ciliary body medulloepithelioma can have a variety of clinical manifestations, depending on the size and extent of the tumor at the time of diagnosis.
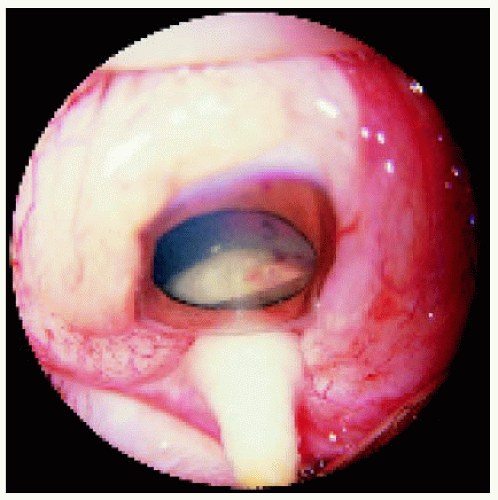 Figure 23.2. Appearance of the same eye shown in Figure 23.1 with a scleral depression, showing a fleshy-white ciliary body mass. The tumor was removed by iridocyclectomy and was found to be a benign nonteratoid medulloepithelioma. |
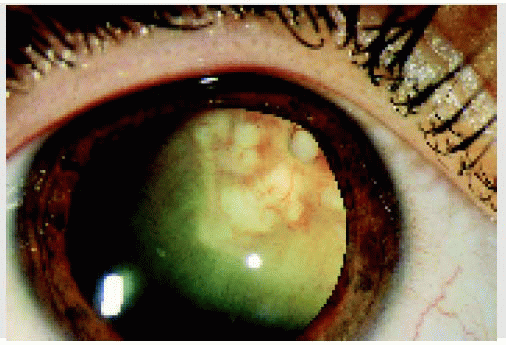
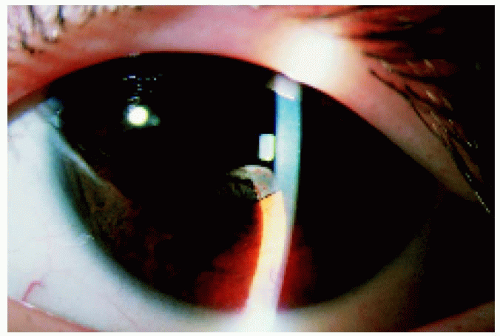 Figure 23.3. Inferior ciliary mass in a 6-year-old boy. The tumor was found after the child underwent surgery for a congenital cataract. It was initially suspected to be a “cyst,” but later examination established the diagnosis of medulloepithelioma. The lesion was removed by iridocyclectomy. A tumor recurrence was treated with a radioactive plaque, and another recurrence necessitated enucleation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|