The corneal epithelium is a highly differentiated cell type that is entirely regenerated approximately every 7 days. In the mechanically abraded cornea (eg, total epithelial debridement during vitrectomy surgery or following photorefractive keratectomy), reepithelialization and restoration of a relatively normal corneal surface occur in 5 days, on average. Numerous studies have demonstrated that the central corneal epithelium is maintained by continued centripetal movement of peripheral corneal epithelium toward the visual axis, as well as by anterior movement of the basal epithelial cells.
The source of the peripheral corneal epithelium is believed to be stem cells that reside in the basal layer of the limbus. Eyes that have a normal reservoir of functioning stem cells possess the ability to rapidly replace and maintain the corneal epithelium. However, when there is damage to the limbal stem cells, the conjunctival epithelium resurfaces the cornea. It was long believed that conjunctival cells retained the capacity for phenotypic change into corneal epithelium, but we now know this is not the case. Conjunctival cells do not have the pluripotency of limbal stem cells and cannot differentiate into the corneal phenotype. Replacement of the corneal epithelium by conjunctival epithelium is characterized by abnormal epithelium on the cornea, vascularization, surface irregularity, absence of the limbal palisades of Vogt, and poor epithelial adhesion, a process called conjunctivalization.
Surgical Procedures of the Ocular Surface
Limbal Transplantation
As discussed in the previous section, the absolute necessity of repopulating the corneal surface epithelium with stem cells forms the rationale for syngeneic or allogeneic (cultured cell or tissue) limbal stem cell transplantation.
If total loss of limbal stem cells occurs unilaterally, an autograft of limbal epithelium from the fellow eye can repopulate the diseased cornea with normal corneal epithelium (Fig 14-1). In this procedure, corneal epithelium, conjunctiva, and superficial pannus are removed from within 2 mm outside the limbus of the recipient eye, and 2 thin limbal autografts from the fellow eye are then attached to the limbus and allowed to regenerate and proliferate.
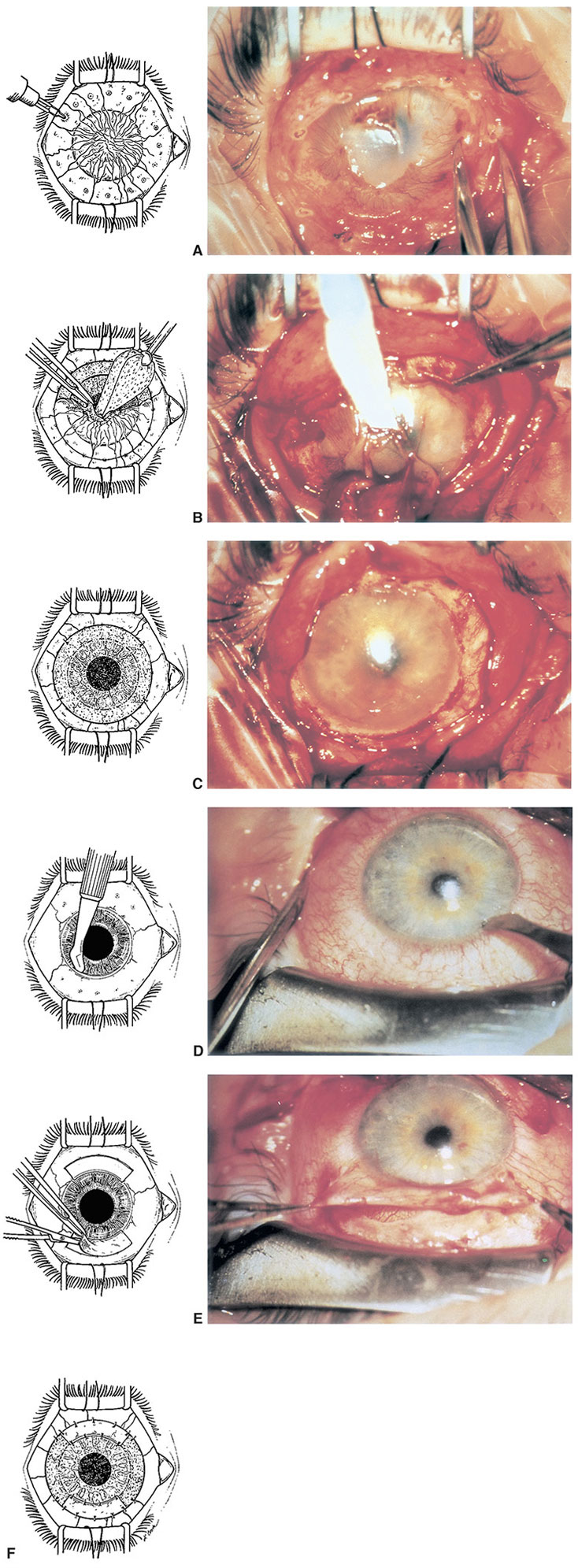
Figure 14-1 Limbal autograft procedure. A, With disposable cautery, the area of bulbar conjunctiva to be resected is marked approximately 2 mm posterior to the limbus. B, After conjunctival resection, abnormal corneal epithelium and fibrovascular pannus are stripped by blunt dissection using cellulose sponges and tissue forceps. C, Additional surface polishing smooths the stromal surface and improves clarity. D, Superior and inferior limbal grafts are delineated in the donor eye with focal applications of cautery approximately 2 mm posterior to the limbus. The initial incision is made superficially within clear cornea using a disposable knife. E, The bulbar conjunctival portion of the graft is undermined and thinly dissected from its limbal attachment. F, The limbal grafts are transferred to their corresponding sites in the recipient eye and are secured with interrupted sutures, 10-0 nylon suture at the corneal edge and 8-0 polyglycolic acid suture at the conjunctival margin. (Reproduced by permission from Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96(5):709–723.)
If total loss of limbal stem cells occurs bilaterally, the options for ocular surface transplantation are more limited. A limbal stem cell allograft from a living related donor may be considered. A similar procedure, keratolimbal allograft, uses corneolimbal rims from eye bank donor eyes. Although host cells may eventually reject or replace such tissue, good long-term results have been reported. Technical difficulties, poor epithelial viability, and rejection problems requiring systemic immunosuppression have limited the usefulness of this modality, but dramatic success has been observed in selected desperate cases.
Stem cell expansion by means of cell culture has proven an effective method of cell surface repopulation. Corneal stem cells have been used for this purpose, but the long-term survival of these grafts remains uncertain. Epithelial cells present in the oral mucosa and the human umbilical cord are emerging as important sources of cultured stem cells. At present, these approaches are experimental and available in few centers worldwide.
Biber JM, Skeens HM, Neff KD, Holland EJ. The Cincinnati procedure: technique and outcomes of combined living-related conjunctival limbal allografts and keratolimbal allografts in severe ocular surface failure. Cornea. 2011;30(7):765–771.
Burillon C, Huot L, Justin V, et al. Cultured autologous oral mucosal epithelial cell-sheet (CAOMECS) transplantation for the treatment of corneal limbal epithelial stem cell deficiency. Invest Ophthalmol Vis Sci. 2012;53(3):1325–1331.
Chan CC, Biber JM, Holland EJ. The modified Cincinnati procedure: combined conjunctival limbal autografts and keratolimbal allografts for severe unilateral ocular surface failure. Cornea. 2012;31(11):1264–1272.
Holland EJ, Mogilishetty G, Skeens HM, et al. Systemic immunosuppression in ocular surface stem cell transplantation: results of a 10-year experience. Cornea. 2012;31(6):655–661.
O’Callaghan AR, Daniels JT. Concise review: limbal epithelial stem cell therapy: controversies and challenges. Stem Cells. 2011;29(12):1923–1932.
Sangwan VS, Basu S, Vemuganti GK, et al. Clinical outcomes of xeno-free autologous cultivated limbal epithelial transplantation: a 10-year study. Br J Ophthalmol. 2011;95(11):1525–1529.
Autologous Conjunctival Transplantation
Autologous conjunctival transplantation is appropriate for cases in which conjunctival loss, inflammation, or scarring is not complicated by extensive damage to or destruction of the limbal epithelial stem cells. This technique is essentially a free conjunctival graft designed to repair a focal or localized defect in the conjunctiva. The most common indication for conjunctival autograft transplantation is advanced primary and recurrent pterygium. See Chapter 12 for additional discussion of pterygium. Pterygium excision and conjunctival autografting, including surgical technique, are discussed in the following section.
Another indication is an enlarged pinguecula, which, in rare cases, may cause chronic irritation, requiring removal combined with an autologous conjunctival replacement graft. Occasionally, unilateral fornix foreshortening occurs after localized disease, retinal detachment surgery, strabismus surgery, or excision of ocular surface tumors or nevi. This foreshortening can be remedied with placement of a conjunctival autograft from the fellow eye. Usually, however, conditions associated with fornix obliteration (mucous membrane pemphigoid, Stevens-Johnson syndrome) are bilateral, so uninvolved conjunctiva is not available for grafting. Mucous membrane transplantation using buccal and even nasal mucosa (if possible, because of the systemic nature of some diseases) or amniotic membrane is an option for ocular surface replacement in such instances (discussed later in this chapter).
Pterygium Excision
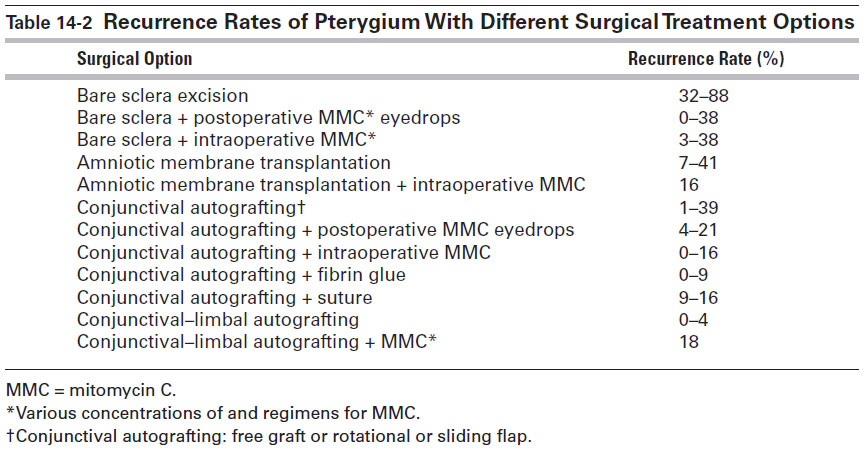
Indications for pterygium excision include persistent discomfort, vision distortion and induction of irregular astigmatism, significant (>3–4 mm) and progressive growth toward the corneal center/visual axis, and restricted ocular motility. The aim of microsurgical excision of a pterygium is to achieve a normal, topographically smooth ocular surface. The procedure is performed on an outpatient basis using topical anesthesia and, in some cases, peribulbar or retrobulbar anesthetic, especially in recurrent cases complicated by scarring. A traction suture (eg, 6-0 silk or polyglycolic acid on a spatulated needle) placed at the 12 o’clock position, which can then be clamped down in various positions to the surgical drape, facilitates maximal exposure of the pterygium and the graft site. A common surgical technique is to remove the pterygium using a flat blade or an angled crescent blade, which allows a smooth plane of dissection toward the limbus. Although it is preferable to dissect down to bare sclera at the limbus, the surgeon should be careful when dissecting Tenon tissue medially, as doing so can sometimes lead to bleeding and later scarring from inadvertent trauma to subjacent muscle tissue and muscle check ligaments. After excision, light cautery is usually applied to the sclera for hemostasis. It is important to remove as much of the fibrovascular scar tissue as possible. If the medial rectus muscle is restricted, it must be isolated and carefully freed of all scar tissue. A smooth surface at the site of dissection is a desirable endpoint. With the eye rotated to expose the involved quadrant, the size of the defect is measured with calipers. Options for wound closure include the following (Fig 14-2; Table 14-2 lists the recurrence rate of pterygium with some of these options):
- Bare sclera. No sutures or fine, absorbable sutures are used to appose the conjunctiva to the superficial sclera in front of the rectus tendon insertion, leaving an area of exposed sclera. Note that this technique has an unacceptably high recurrence rate and is therefore strongly not recommended.
- Simple closure. The free edges of the conjunctiva are secured together (effective only when the conjunctival defect is very small).
- Sliding flap. An L-shaped incision is made adjacent to the wound to allow a conjunctival flap to slide into place.
- Rotational flap. A U-shaped incision is made adjacent to the wound to form a tongue of conjunctiva that is rotated into place.
- Autologous conjunctival transplantation. As mentioned previously, this is a free graft, usually from the superior bulbar conjunctiva. The graft is excised to correspond to the size of the wound and is then moved and either sutured into place or fixated with a tissue adhesive (fibrin sealant made from pooled human plasma). This technique is described in more detail below.
- Autologous conjunctival–limbal transplantation. This is also a free graft, but it includes limbal stem cells in addition to the conjunctival graft. (See below for surgical technique.)
- Amniotic membrane transplantation. A free amniotic membrane graft may be an alternative to conjunctival autograft, although free conjunctival grafting is still more successful and is the preferred technique. Amniotic membrane is indicated particularly when there is a shortage of autologous conjunctiva. These grafts may be most useful with large pterygia, where a wide excision is needed. There are insufficient data to comment on the efficacy of amniotic membrane grafting as an adjuvant in pterygium surgery.
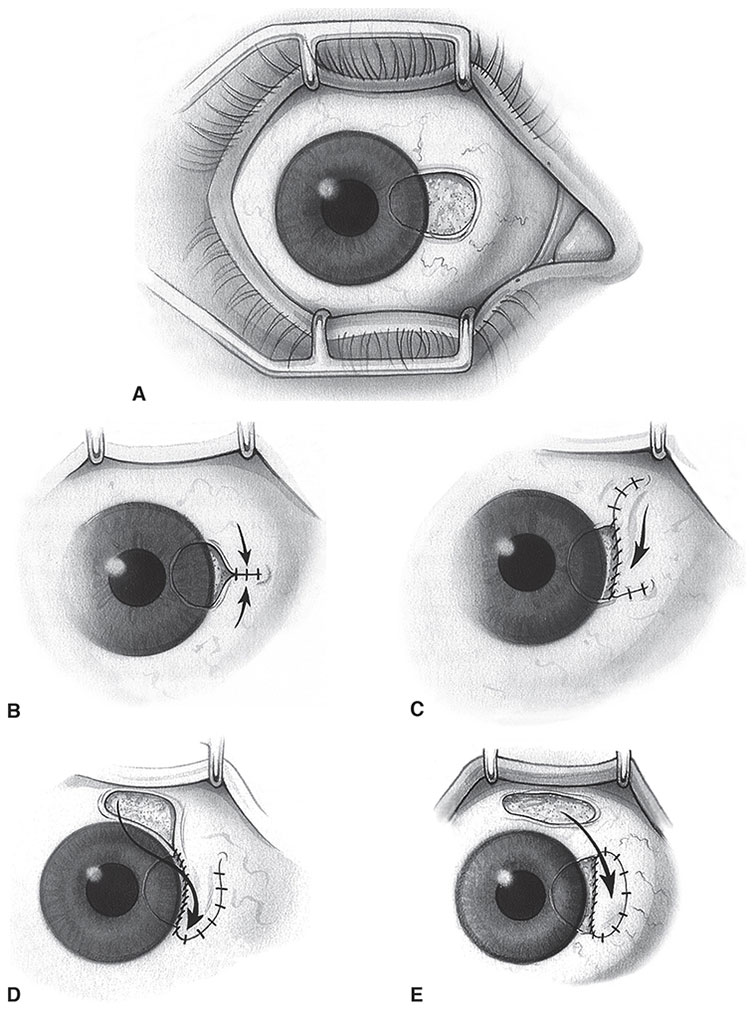
Figure 14-2 Surgical wound closures following pterygium excision. A, Bare sclera. B, Simple closure with fine, absorbable sutures. C, Sliding flap that is closed with interrupted and/or continuous suture. D, Rotational flap from the superior bulbar conjunctiva. E, Conjunctival autograft that is secured with interrupted and/or continuous suture. (Reproduced with permission from Gans LA. Surgical treatment of pterygium. Focal Points: Clinical Modules for Ophthalmologists. San Francisco: American Academy of Ophthalmology; 1996, module 12. Illustration by Christine Gralapp.)
Table 14-2
If autologous conjunctival transplantation is to be performed, then the eye is turned down to expose the superior bulbar conjunctiva, and the area to be harvested is marked with a surgical pen. The most important aspect of the harvesting is to procure conjunctival tissue with only minimal or no Tenon included. This may be facilitated by injection of a small amount of anesthetic between the conjunctiva and Tenon capsule. Some surgeons make a special point of harvesting limbal stem cells along with the conjunctiva and orienting the donor material in the host bed so that the stem cells are adjacent to the site of corneal lesion excision. It is best to allow a little extra tissue for grafting, so the harvested tissue should be approximately 0.5–1.0 mm larger than the size of the defect in the area of the excised pterygium.
The donor site is usually left bare. After the graft is freed, it is transferred to the recipient bed and secured to adjacent conjunctiva (with or without incorporating episclera) with 7-0 to 10-0 polyglycolic acid (absorbable) or nylon (nonabsorbable) suture or with tissue adhesive. Many authors have described the use of commercially available fibrin tissue adhesive to fixate the conjunctival autograft, thereby eliminating the need for suture fixation. Elimination of sutures decreases postoperative pain and reduces surgical time as well as the recurrence rate, compared with bare sclera techniques (see Table 14-2). Fibrin tissue adhesive mimics natural fibrin formation, ultimately resulting in the formation of a fibrin clot. Several fibrin sealants have been approved by the US Food and Drug Administration (FDA) and are commercially available and distributed by US companies, including Tisseel Fibrin Sealant (Baxter Healthcare Corporation, Westlake Village, CA), Evicel Fibrin Sealant (Ethicon, Inc, Somerville, NJ), and BioGlue Surgical Adhesive (CryoLife, Inc, Kennesaw, GA). There is also the CryoSeal FS System (ThermoGenesis Corp, Rancho Cordova, CA), which can be used in the automated preparation of fibrin sealant from the patient’s own plasma. Currently, use of these products in pterygium surgery is considered off-label. Also, because both pooled human plasma and bovine products are used to obtain some components of these products, careful consideration should be given to the potential for disease transmission with their use.
If the defect created following dissection of scar tissue is considerably larger than what can be covered with an autologous conjunctival graft, then an amniotic membrane graft may be used in conjunction with a conjunctival graft to cover the entire area of resection. Several authors have noted that this decreases postoperative inflammation and speeds reepithelialization of the surface.
There is evidence that the use of mitomycin C (MMC) with conjunctival autografting reduces the recurrence rate of pterygium after surgical excision (see Table 14-2). However, further studies are necessary to determine the optimal route of administration and dose for MMC, as well as the duration of treatment with MMC and its long-term effects. In studies, the concentration of intraoperative MMC, administered locally for 3 to 5 minutes, varies from 0.002% to 0.04%. The concentration of postoperative MMC eyedrops, administered 2–4 times a day, varies from 0.02% to 0.04%. It is important to note that any use of topical MMC can be toxic and may cause visually significant complications such as aseptic scleral necrosis and infectious sclerokeratitis. These complications may occur months, or even years, after use of the drug. If surgery is being performed in a case of recurrent pterygium and MMC use is being considered, it is safer to apply this agent intraoperatively than to give it to the patient for postoperative topical application; in the latter case, overuse may be a problem.
Postoperatively, topical antibiotic–corticosteroid eyedrops are administered frequently for approximately 4–6 weeks, until inflammation subsides. The surgeon should emphasize to the patient that adherence to this regimen will minimize the chance of recurrence.
The use of bevacizumab in primary pterygium excision apparently has no effect on the recurrence rate of this condition.
Al Fayez MF. Limbal versus conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 2002;109(9):1752–1755.
Ari S, Çaca I, Yildiz ZO, Şakalar YB, Dogan E. Comparison of mitomycin C and limbalconjunctival autograft in the prevention of pterygial recurrence in Turkish patients: A one-year, randomized, assessor-masked, controlled trial. Curr Ther Res. 2009;70(4):267–350.
Cano-Parra J, Diaz-Llopis M, Maldonado MJ, Vila E, Menezo JL. Prospective trial of intraoperative mitomycin C in the treatment of primary pterygium. Br J Ophthalmol. 1995;79(5):439–441.
Cardillo JA, Alves MR, Ambrosio LE, Poterio MB, Jose NK. Single intraoperative application versus postoperative mitomycin C eye drops in pterygium surgery. Ophthalmology. 1995;102(12):1949–1952.
Chen PP, Ariyasu RG, Kaza V, LaBree LD, McDonnell PJ. A randomized trial comparing mitomycin C and conjunctival autograft after excision of primary pterygium. Am J Ophthalmol. 1995;120(2):151–160.
Frucht-Pery J, Ilsar M. The use of low-dose mitomycin C for prevention of recurrent pterygium. Ophthalmology. 1994;101(4):759–762.
Keklikci U, Celik Y, Cakmak SS, Unlu MK, Bilek B. Conjunctival-limbal autograft, amniotic membrane transplantation, and intraoperative mitomycin C for primary pterygium. Ann Ophthalmol (Skokie). 2007;39(4):296–301.
Kheirkhah A, Hashemi H, Adelpour M, Nikdel M, Rajabi MB, Behrouz MJ. Randomized trial of pterygium surgery with mitomycin C application using conjunctival autograft versus conjunctival-limbal autograft. Ophthalmology. 2012;119(2):227–232.
Kheirkhah A, Nazari R, Nikdel M, Ghassemi H, Hashemi H, Behrouz MJ. Postoperative conjunctival inflammation after pterygium surgery with amniotic membrane transplantation versus conjunctival autograft. Am J Ophthalmol. 2011;152(5):733–738.
Mahdy RA, Wagieh MM. Safety and efficacy of fibrin glue versus Vicryl sutures in recurrent pterygium with amniotic membrane grafting. Ophthalmic Res. 2012;47(1):23–26.
Ozer A, Yildirim N, Erol N, Yurdakul S. Long-term results of bare sclera, limbal-conjunctival autograft and amniotic membrane graft techniques in primary pterygium excisions. Ophthalmologica. 2009;223(4):269–273.
Pan HW, Zhong JX, Jing CX. Comparison of fibrin glue versus suture for conjunctival autografting in pterygium surgery: a meta-analysis. Ophthalmology. 2011;118(6):1049–1054.
Ratnalingam V, Eu AL, Ng GL, Taharin R, John E. Fibrin adhesive is better than sutures in pterygium surgery. Cornea. 2010;29(5):485–489.
Shahin MM, Elbendary AM, Elwan MM. Intraoperative subconjunctival bevacizumab as an adjunctive treatment in primary pterygium: a preliminary report. Ophthalmic Surg Lasers Imaging. 2012;43(6):459–466. Epub 2012 Aug 10.
Shenasi A, Mousavi F, Shoa-Ahari S, Rahimi-Ardabili B, Fouladi RF. Subconjunctival bevacizumab immediately after excision of primary pterygium: the first clinical trial. Cornea. 2011;30(11):1219–1222.
Tan DT, Chee SP, Dear KB, Lim AS. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol. 1997;115(10):1235–1240.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


