 ransciliary filtration for intractable glaucoma” was first presented by Daljit Singh at the 1979 meeting of the Ophthalmological Society of the United Kingdom. In 2000, he successfully used the Fugo blade to do transciliary filtration (TCF) in a case of keratoprosthesis. Making a track through the highly vascular tissue of the ciliary body was possible because the Fugo blade ablates both tissue and blood vessels in the line of incision, and does so without the charring seen with cauterizing devices. After early successes, TCF surgery was extended to other cases of glaucoma.
ransciliary filtration for intractable glaucoma” was first presented by Daljit Singh at the 1979 meeting of the Ophthalmological Society of the United Kingdom. In 2000, he successfully used the Fugo blade to do transciliary filtration (TCF) in a case of keratoprosthesis. Making a track through the highly vascular tissue of the ciliary body was possible because the Fugo blade ablates both tissue and blood vessels in the line of incision, and does so without the charring seen with cauterizing devices. After early successes, TCF surgery was extended to other cases of glaucoma.
TCF can be performed in any case of glaucoma in which the posterior chamber is intact and no vitreous blocks the internal opening of the filtering track. The filtration track passes through the anterior part of the sclera, the longitudinal and the circular fibers of ciliary muscle, and the ciliary processes. Since the ciliary body structure is narrowest anteriorly, the more anterior the track formation, the shorter the path to the posterior chamber.
Anatomy of the Posterior Chamber
The posterior chamber is the aqueous-filled space immediately behind the iris but in front of the lens. It is triangular in shape, the apex being toward the pupil and a 1-mm-wide base laterally. The anatomy of the lateral wall is an important consideration for TCF procedures. The ciliary body lies posterior to the iris and has two components: the ciliary muscle and the ciliary processes. The ciliary muscle is triangular in cross section, the apex pointing posteriorly, ending at the ora serrata. The outermost longitudinal fibers attach to the corneoscleral meshwork and the scleral spur. Internal to the ciliary muscle, the ciliary processes form the pars plicata. Approximately 70 radially arrayed major ciliary processes project into the posterior chamber. Their anterior borders arise from the iris root, sweeping behind the iris to form the ciliary sulcus. These major processes are approximately 2 mm long, 0.5 mm wide, and 1 mm high and possess an irregular surface. Smaller minor ciliary processes lie between the major processes and do not project as far into the posterior chamber as the major processes. Approximately two ciliary processes exist for every millimeter of the circular ciliary body. In phakic eyes, the ciliary processes are anchored to the lens via the zonular fibers; therefore, the processes do not move freely, as the iris does. It is possible that the ciliary body as a whole moves slightly during accommodation or under the effect of mydriatics or miotics. Theoretically, this sliding movement could close a surgically created track.
During the process of TCF track formation, the ablating tip of 100 or 300 µm (the fully activated plasma tip adds an additional 100µm) ideally enters into open space in the posterior chamber. Alternatively, it can partially or fully penetrate the ciliary body. As such, Fugo blade tip penetration into the posterior chamber can vary depending on where it successfully communicates with aqueous. When the ablating tip passes through the anterior part of the ciliary muscle, the overall distance the tip travels is less than when the track is made more posteriorly. The success of the TCF procedure depends on how the tissues of the ciliary process, ciliary muscle, sclera, and tenon capsule react to the traumatic creation of a new drainage channel and the flow of the aqueous through them.
TECHNIQUE
Anesthesia
We recommend topical anesthesia combined with peribulbar or retrobulbar injection of 1% lidocaine.
Surgical Technique
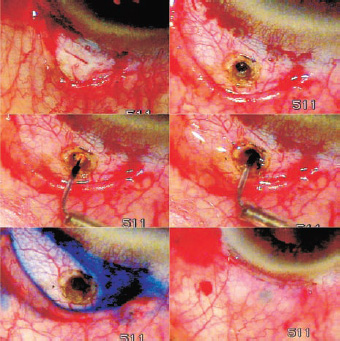
Figure 31.1. Transciliary filtration procedure. After opening the conjunctiva from the limbus a mark is made 1 mm behind the limbus. A scleral pit to the ciliary body made is with a 600-µm Fugo blade tip. The pit is beveled, especially anteriorly. An activated 100-µm Fugo blade passes through the ciliary body into the posterior chamber. Flow of aqueous is demonstrated with a drop of trypan blue. The conjunctiva is sutured at the limbus.
- Open the conjunctiva at the limbus for 5 to 6 mm, then remove fibrous tissue to bare sclera (Fig. 31.1). You may extend the edge of either side of the incision radially to loosen the conjunctival flap and excise the thick tenon capsule. If you apply adjunctive mitomycin, the tenon capsule is preserved.
- Inspect the episcleral surface. Touch any episcleral bleeding that does not stop spontaneously in 2 to 3 minutes with a 600-µm Fugo blade tip at the lowest setting. Avoid blanching the episclera with bipolar cautery to preserve normal vascularity of the scleral surface.
- Visualize the ciliary body by transillumination, which is particularly useful in large globes. The ablation path passes through the sclera and ciliary body to the lateral wall of the posterior chamber. This is achieved with the plasma blade in two steps: first, create an ablated pit in the sclera; second, pass through the ciliary body. You must clearly understand the technique for creating the scleral pit. Make the pit with the 600-µm Fugo blade tip; it can be anywhere from 1 to 1.5 mm behind the limbus. Making a scleral pit beyond 1 mm with a 600-µm tip effectively extends the upper edge of the pit to about 1.8 to 2 mm from the limbus. The pit is vertical and extends through the suprachoroidal space. A part of the ciliary muscle may also be ablated in the process. The depth of the scleral pit occasionally makes it difficult to correctly maintain the proper plane when entering the posterior chamber. Modifications to the scleral pit can be made as follows to suit immediate surgical needs:
- The pit can be undermined in all directions to produce a larger ablated pit.
- It can be undermined anteriorly, stopping short of entering the anterior chamber. The thinned cornea can be opened later with an yttrium– aluminum–garnet (YAG) laser, if necessary. Anterior chamber filtration with TCF (Atwal’s approach) can be integrated with the procedure by creating one or more tracks through the anterior wall of the scleral pit.
- It may be beveled all around, for easier egress and draining of outflowing aqueous.
It is not yet certain whether the distance of the scleral pit from the limbus has an effect on the postoperative response of the tissues. We do know that the limbus abounds in stem cells, yet we know nothing about their contribution to the success or failure of the surgery after filtration.
- The pit can be undermined in all directions to produce a larger ablated pit.
- You may apply mitomycin C 0.05% (MMC) at this stage to the scleral pit, under the conjunctival flap, or both. For the former, administer MMC as a small droplet on the tip of a 30-gauge needle; dip it into the pit and leave it there for 3 to 4 minutes. For the second option, lift the conjunctival flap and apply a small sponge soaked with MMC to the episclera, being careful not to expose the edge of the flap. Vigorously irrigate the area with saline after 2 to 3 minutes.
- To make the transciliary track, proceed with ablation through the ciliary body and its processes. The shortest distance through the ciliary body to the posterior chamber is near its attachment at the scleral spur. The depth of the ciliary body increases as the track orientation moves posteriorly. While creating an anteriorly placed track, direct the ablating tip 45 degrees. If the scleral entry point moves posteriorly, keep the 100-µm (or 300-µm) tip more parallel to the iris plane. The ideal point for scleral pit opening is as yet undetermined. Penetrating the ciliary body has many variables. You can use any of the three sizes (100, 300, or 600 µm) of Fugo blade tips.
You may ablate the ciliary body with a 600-µm tip at medium power and medium energy, making a deep wide track completely into the posterior chamber. This is easier to do if the track is made near the anterior aspect of the suprachoroidal space.
Stop partial ablation with a 600-µm tip at any point and create the remaining track with a 300-µm or 100-µm tip.
Make the track through the ciliary body with the 300- or 100-µm tip (the classic TCF). Set the energy level at high and move the ablating tip slowly, thereby allowing more energy absorption and creation of a larger ablation track. Entry into the posterior chamber results in vigorous flow of aqueous with specks of pigment from the ciliary body. Occasionally, a thin stream of blood may appear that oozes for a couple of minutes. Do not try to stop it by pressure, as the blood may collect in the posterior chamber. Confirm the flow of aqueous by inserting a drop of trypan blue diluted by aqueous. Confirm the track’s patency by introducing air into the scleral pit through a large-bore cannula. The air passes under the iris and through the pupil into the anterior chamber. In cases with a shallow anterior chamber with or without iris bombe the anterior chamber deepens the moment the fluid starts begins to drain from the posterior chamber.
- Suture the conjunctiva to the limbus.
- To make the transciliary track, proceed with ablation through the ciliary body and its processes. The shortest distance through the ciliary body to the posterior chamber is near its attachment at the scleral spur. The depth of the ciliary body increases as the track orientation moves posteriorly. While creating an anteriorly placed track, direct the ablating tip 45 degrees. If the scleral entry point moves posteriorly, keep the 100-µm (or 300-µm) tip more parallel to the iris plane. The ideal point for scleral pit opening is as yet undetermined. Penetrating the ciliary body has many variables. You can use any of the three sizes (100, 300, or 600 µm) of Fugo blade tips.
Intra-operative Complications
Creating a scleral pit may promote bleeding, even before the ablating tip reaches the ciliary body. Avoid creating a pit at or near a large vessel. When bleeding occurs after the track has been made through the ciliary body, wait until it stops. (The site for TCF can be moved to an adjacent area.) In addition, it is advisable to irrigate the posterior chamber to make sure that no blood collects there.
A misdirected track can penetrate into the anterior chamber or into the vitreous. In the latter case, close the scleral opening with one tight suture and make a new TCF track. When the track errantly enters into the anterior chamber, direct the same ablating tip more posteriorly to and then enter the posterior chamber. Do this after filling the anterior chamber with saline and following with an air bubble; both maneuvers done to inflate the posterior chamber.
Postoperative Management
At the end of the operation, lightly patch the eye and apply a shield. Have the patient open the eye after 3 to 4 hours, when the effect of the facial block has worn off. Request that the patient instill topical steroid drops six to eight times a day. Use steroid–antibiotic ointment at bedtime.
The anterior chamber may be shallow, but is rarely, if ever, flat. Choroidal detachment is rare and recovers spontaneously. Although microscopic hyphema is frequently seen, layered hyphema is uncommon; if it does occur, it does not interfere with the filtration track. It may be left untreated and will spontaneously absorb.
The success or failure of filtration after TCF is the main postoperative concern. Early failure may occur because of a blood clot formation. Conjunctival scars may form quickly, especially in younger patients and in darkly pigmented patients. Tenon cyst formation is also a sign of a vigorous repair process. The role of the conjunctival lymphatics in the drainage of normal aqueous from the uveoscleral route and their role in aqueous management after filtration surgery should not be underestimated. Every effort should be made to minimize trauma: mechanical, thermal, or chemical. Histologic studies of TCF-operated animal or cadaver eyes are not yet available.
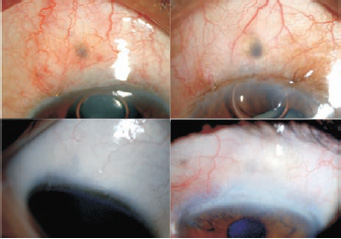
Figure 31.2. Top: Blebs in the early postoperative period. Bottom: The same TCF blebs years after surgery.
Blebs after Transciliary Filtration
Although nothing is standard about blebs in any particular glaucoma surgery technique, TCF blebs have certain characteristics. Because the TCF track is direct, it promotes symmetric aqueous distribution under the conjunctiva and produces a broad, borderless bleb (Fig. 31.2).
Concurrent Transciliary Filtration and Phacoemulsification
Because of predictable adequate anterior chamber depth, TCF may be considered a preferable filtering procedure to combine with phaco-emulsification. Scleral ablation is done before phaco-emulsification, whereas penetration into the posterior chamber is completed after phaco-emulsification. It is important to pay attention to adequate volume reconstitution of the anterior and posterior chambers at the end of the phaco procedure to ensure ample egress of aqueous fluid when the posterior chamber is entered.
Neovascular Glaucoma
Cases of neovascular glaucoma are treated well by TCF because this procedure requires no manipulation of the iris. Oozing blood from the angle resulting from operative relative hypotony usually does not interfere with the aqueous outflow through the posterior chamber. We suggest the concurrent use of intravitreal bevacizumab (off-label).
Reoperation after Transciliary Filtration
The two approaches to reoperation after TCF are (1) opening the conjunctiva from the limbus and revising the track (open revision) and (2) performing transconjunctival transciliary filtration (TCTCF) (closed revision).
Open Revision of Transciliary Filtration
Surgical Technique
Open the conjunctiva as previously described. If present, scar or tenon cyst formation is removed from the field with the 600-µm Fugo blade tip. The filtration track may start working spontaneously or may be revived by additional ablative treatment in the same site. Loss of filtration may occur because of a clot within the pit or deeper in the track. Once retreated, verify the egress of the fluid with a drop of trypan blue and resuture the conjunctiva (Fig. 31.3)
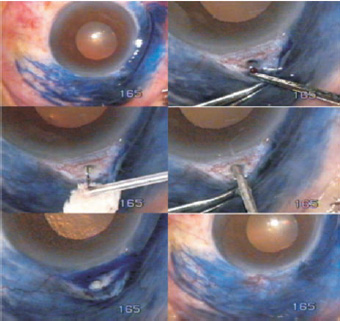
Figure 31.3. Filtration after failed TCF. Lymphatic charting showed a healthy network. On opening the conjunctiva, a blood clot was observed in the scleral pit. The track was reopened with a 100-µm Fugo blade tip, aqueous flow was confirmed with trypan blue, and the conjunctiva was sutured back to the limbus.
Closed Revision of Transciliary Filtration
Surgical Technique
In closed revision of TCF (TCTCF) (Fig. 31.4), pull down and stretch redundant conjunctiva while passing an activated 300-µm Fugo blade tip through the conjunctiva into the old TCF track until it draws aqueous from the posterior chamber. The relative ease and efficacy of TCTCF surgery have led some to consider TCTCF as a primary surgery for glaucoma.

Figure 31.4. Revision of a filtering bleb. The conjunctiva from the fornix side is folded over the original track. A 300-µm Fugo blade tip ablates through the conjunctiva and the previously created track, and aqueous begins to flow. The conjunctival opening is closed with a suture. A broad, low bleb is the result.
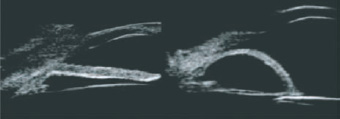
Figure 31.5. Ultrasound biomicroscopy aids in visualizing the posterior chamber, finding the best site for filtration and enabling the surgeon to determine the best anatomic approach to the posterior chamber.
Role of Ultrasound Biomicroscopy in Transciliary Filtration
Ultrasound biomicroscopy (UMB) allows visualization of the anatomy of the posterior chamber (Fig. 31.5). UMB images orient the surgeon to the site of the scleral pit and the direction of the ciliary body ablating tip. It is possible to judge the volume of the posterior chamber and the expected flow of the aqueous when the posterior chamber is reached.
Future Role of Fiberoptic Cameras
Currently, the operating microscope provides lighting and magnification of the operative field. Ablating the ciliary body is done blindly, assisted primarily by the surgeon’s instinct and sense of direction. Microfiberoptic cameras with amazing resolution are expected to become available in the future. These cameras are capable of revealing the internal as well as the external microanatomic detail of the surgical site, allowing for complete control of Fugo blade ablation. This technologic advance will bring about a new era of directly visualized microsurgery that will likely become the standard for glaucoma surgery.
Summary
After a century-long search for better anterior chamber filtration, posterior chamber filtration is an interesting alternative. It is accomplished without disturbing the existing natural drainage and, in fact, enhances functioning by reducing the potential for iris bombe and encroachment on the corneoscleral trabeculae.
Suggested Readings
Dow CT, deVenecia G. Transciliary filtration (Singh procedure) with the Fugo plasma blade. Ann Ophthalmol (Skokie). 2008 Spring;40(1):8–14.
Fugo R. Regarding transciliary filtration. Trop Ophthalmol. 2002;2:7–8.
Fugo R. Transciliary filtration procedure offers new approach to glaucoma. Ocular Surgery News. 2005; 23:4–26.
Guttman C. Transciliary filtration provides improved safety and simplicity. Ophthalmol Times. 2005;30:28.
Kent C. FDA approves new glaucoma filtration procedure. Rev Ophthalmol. 2004;11:6–8.
Kent C. Transciliary filtration—without bleeding. Ophthalmol Manage. 2002;6:84–87.
Singh D. Singh micro-filtration for glaucoma: a new technique. Trop Ophthalmol. 2001;1:7–11.
Singh D. Transciliary filtration & lymphatics of conjunctiva— a tale of discovery. Trop Ophthalmol. 2002;2:9–13.
Singh D, Singh K. Transciliary filtration using the Fugo blade. Ann Ophthalmol. 2002;34:183–187.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree