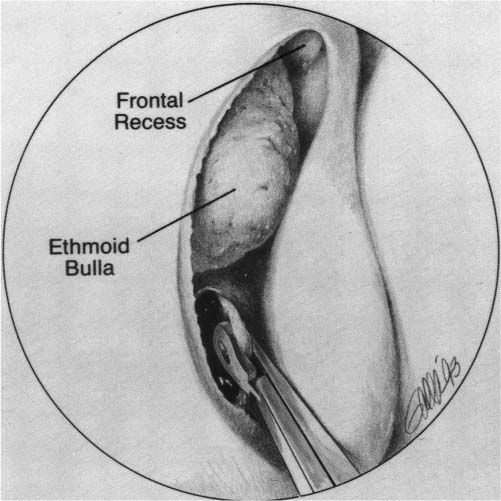
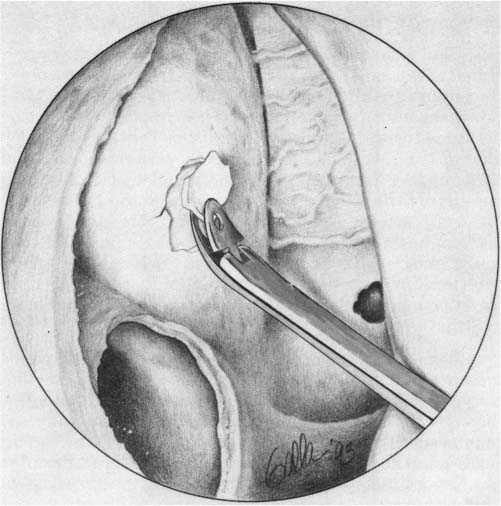
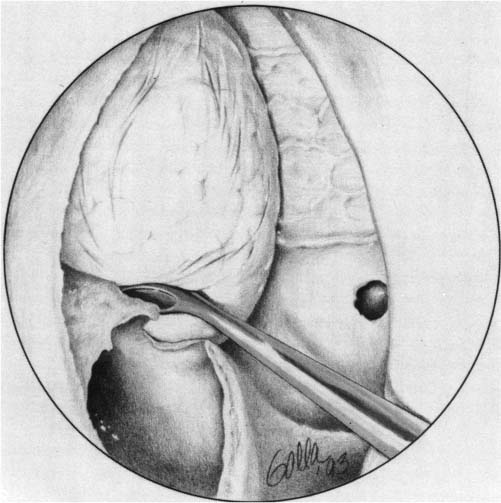
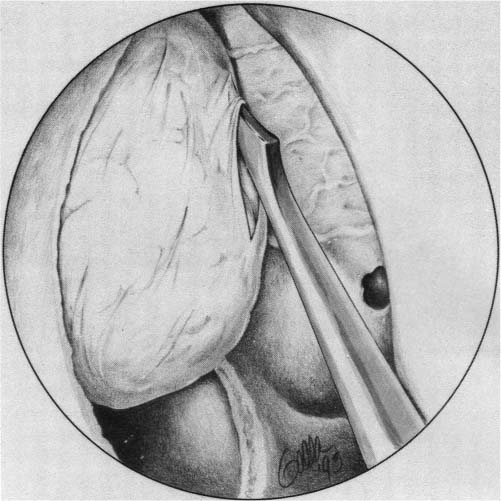
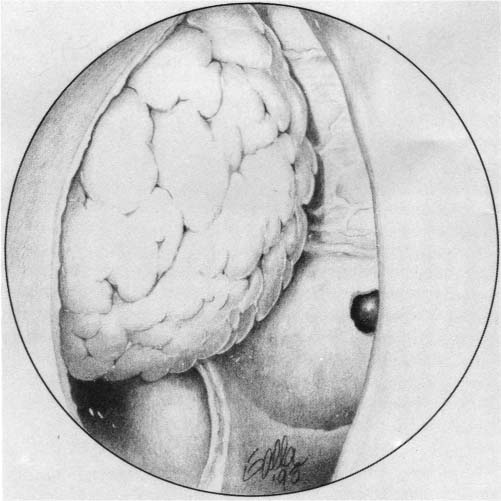
20 The Maxillary Sinus and Surgical Treatment of Graves Orbitopathy Graves disease is a systemic autoimmune disorder that can affect the thyroid, skin, and orbit. Although hyperthyroidism is the most common presenting manifestation, up to 80% of persons with Graves disease develop ocular findings, known as Graves orbitopathy.1 Severe orbital disease poses a threat to vision in 3 to 5% of patients with Graves orbitopathy.1,2 The orbital symptoms associated with Graves disease represent an autoimmune process, although the exact mechanism is not completely understood. Accumulation of lymphocytes and deposition of mucopolysaccharides in orbital soft tissues lead to enlargement of extraocular muscles and orbital fat. In the restrictive confines of the bony orbit, the discrepancy between orbital volume and its expanded contents causes anterior displacement of the globe and posterior pressure on the orbital apex, which can result in exophthalmos and optic nerve compression. It is important to note, however, that the degree of proptosis does not correlate with the overall severity of disease because patients with poor compliance of the orbital septum may not exhibit significant proptosis, but can have severe compression at the orbital apex with optic neuropathy. Clinical manifestations of Graves orbitopathy range from mild findings, such as tearing, photophobia, and conjunctival injection, to severe symptoms, such as disfiguring exophthalmos, diplopia, corneal ulceration from exposure keratopathy, and visual loss from optic neuropathy. The orbital manifestations of Graves disease follow a distinct and independent clinical course from the thyroid disease. The clinical course of Graves orbitopathy can be divided into acute and chronic phases. Whereas the acute phase is characterized by active inflammation and lasts 6 to 18 months, the chronic phase is characterized by stable fibrosis.3 Medical treatment of Graves orbitopathy includes systemic corticosteroids and orbital radiation, which seem to be most effective during the acute phase of the disease. When medical treatments fail, however, surgical decompression of the orbit may be necessary and is preferably performed during the chronic phase when the orbitopathy has stabilized. A variety of surgical techniques have been described to decompress the orbit by removing any combination of 1 to 4 bony walls.4–7 In 1930 Oskar Hirsch was the first to report removal of the orbital floor for decompression of the orbit in a patient with exposure keratopathy due to Graves disease. The operation represented the first description of decompression of orbital contents into the maxillary sinus and resulted in resolution of corneal exposure.4,5 In 1936 Edward Sewall developed an external ethmoidectomy approach to removal of the medial orbital wall.6 This technique ultimately evolved into the transantral approach to orbital decompression with removal of the medial orbital wall and floor, introduced by Walsh and Ogura in 1957.7 The Walsh–Ogura technique was the mainstay of surgical treatment for Graves orbitopathy for many decades. This procedure enabled otolaryngologists to remove the orbital floor and medial wall through the familiar Caldwell–Luc approach, allowing for decompression of the enlarged orbital muscles and fat into the maxillary and ethmoid sinuses. Their technique involved a sublabial incision to expose and enter the maxillary antrum. A transantral ethmoidectomy was performed and the medial orbital wall was skeletonized. Bone of the lamina papyracea was removed up to the ethmoid roof, and bone along the orbital floor was removed, sparing the infraorbital nerve. Although effective decompression was achieved with this method, the incidence of postoperative diplopia was high. In 1993, Garrity et al reported on a series of 428 patients undergoing transantral orbital decompression for Graves orbitopathy and found a 64% incidence of new-onset postoperative diplopia.8 Furthermore, patients undergoing unilateral decompression often developed hypoglobus with one eye appearing lower than the other. Other disadvantages of the Walsh–Ogura technique included paresthesia along the distribution of the infraorbital nerve and poor visualization of the skull base when performing the transantral ethmoidectomy. Soon after the introduction of endoscopic instrumentation for the performance of sinus surgery in the mid-1980s, surgeons began to experiment with an entirely transnasal approach to treat diseases of the orbit, circumventing the need for external or sublabial incisions and reducing patient morbidity. Endoscopic orbital decompression was pioneered by Kennedy et al and Michel et al in the early 1990s.9,10 Because high-resolution endoscopes provided improved visualization in key anatomic regions, including the orbital apex and skull base, this technique soon gained widespread acceptance for the treatment of patients with Graves disease, largely replacing the transantral approach. Indications for endoscopic orbital decompression include severe exophthalmos, which may result in exposure keratopathy, corneal ulceration, or disfiguring proptosis; compressive optic neuropathy, which may present with color blindness, decreased visual fields, or decreased visual acuity; and diplopia in preparation for strabismus or eye muscle surgery. Surgery is best performed during the chronic phase of the disease when the orbitopathy has stabilized. In some cases, however, severe orbital symptoms may necessitate decompression during the active phase, such as for sight-threatening optic neuropathy that is refractory to medical treatment. The decision to operate must be a team decision involving both the ophthalmologist and the otolaryngologist. Preoperative evaluation includes a complete head and neck examination, ophthalmologic evaluation, and computed tomography scans of the orbits and paranasal sinuses in coronal and axial planes. Ophthalmologic evaluation should include visual acuity, visual fields, conjunctival and corneal examination, Hertel exophthalmometry measurements, and extraocular motility testing. Preoperative and postoperative photography are recommended. The patient is positioned in the supine position, and topical vasoconstriction is achieved with pledgets soaked in oxymetazoline or cocaine 4%. Draping is the same as with standard endoscopic sinus procedures, and the eyes are exposed in the surgical field, but protected with corneal shields. Image guidance systems may be used at the surgeon’s discretion. Lidocaine 1% with epinephrine 1:100,000 is injected along the lateral nasal wall in the region of the maxillary line (a bony eminence that extends from the anterior attachment of the middle turbinate to the root of the inferior turbinate). Surgery begins with an incision just posterior to the maxillary line through the uncinate process (Fig. 20.1) (see Video 20.1). The uncinate process is medialized and removed allowing for visualization of the natural ostium of the maxillary sinus. It is important to open the maxillary sinus widely to achieve good access to the orbital floor and prevent blockage of the ostium from orbital fat, which protrudes after decompression (Fig. 20.2). The ostium can be opened to the floor of the orbit superiorly, the back wall of the maxillary sinus posteriorly, the thick bone of the frontal process of the maxilla anteriorly, and the inferior turbinate inferiorly. A sufficiently widened antrostomy measures ~9 to 16 mm in a well-pneumatized maxillary sinus. If the antrostomy is extended beyond the frontal process of the maxilla anteriorly, there is risk of damage to the nasolacrimal duct. Using a 30-degree endoscope, the wide antrostomy should allow easy visualization of the infraorbital nerve as it courses along the floor of the orbit. Fig. 20.1 View of the right nasal cavity at the start of decompression surgery. The uncinate process is incised just posterior to the maxillary line, an eminence that extends from the anterior attachment of the middle turbinate to the root of the inferior turbinate.(From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:952. Reprinted with permission.) Fig. 20.2 The maxillary sinus ostium is enlarged superiorly to the floor of the orbit, posteriorly to the back wall of the maxillary sinus, anteriorly to the frontal process of the maxilla, and inferiorly to the inferior turbinate. A large maxillary antrostomy is necessary to optimize exposure and removal of the medial orbital floor. (From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:952. Reprinted with permission.) A spoon curette is used to penetrate the thin bone of the lamina papyracea. This bone is elevated while preserving the underlying periorbita. Bone removal proceeds superiorly to the ethmoid roof, inferiorly to the orbital floor, and anteriorly to the maxillary line, and posteriorly to the face of the sphenoid sinus (Fig. 20.3). Bone is not removed in the region of the frontal recess to prevent herniation of orbital fat, which could lead to postoperative obstruction of the frontal sinus. When removing the anterior portion of the lamina papyracea, it is not uncommon to remove fragments of the adjacent lacrimal bone. In this case, the thick white fascia of the underlying lacrimal sac may be uncovered, but should not be opened. Thick bone anterior to the maxillary line protects the majority of the lacrimal sac and need not be removed. As bone removal proceeds in a posterior direction, the underlying periorbita thickens and becomes white in appearance in the region of the orbital apex within 2 mm of the sphenoid face. This tissue corresponds to the annulus of Zinn, from which the extraocular muscles originate, and represents the posterior limit of decompression. Removal of the orbital floor may be the most technically challenging portion of the procedure. Only the portion of the floor medial to the infraorbital nerve is removed. A spoon curette is used to engage the orbital floor at its medial extent and to down-fracture the bone (Fig. 20.4). The bone of the orbital floor is thicker than that of the medial orbital wall, and significant force may be required for this maneuver. If the spoon curette is not sturdy enough for this portion of the procedure, a more robust mastoid curette can be used. The floor may fracture in one large piece, typically with a natural cleavage plane along the infraorbital canal. More commonly, the floor fractures into several small pieces, in which case a 30-degree endoscopic and curved instrumentation may facilitate bone removal. The infraorbital canal is preserved as the lateral limit of dissection. No attempt is made to remove the dense bone lateral to the infraorbital canal, as it serves to support the globe and prevents postoperative hypoglobus. Once the lamina papyracea and medial orbital floor have been removed, the periorbita is fully exposed. A sickle knife is typically used to incise the periorbita (Fig. 20.5). Care must be taken to avoid burying the tip of the knife, which could injure the underlying orbital contents, including the medial rectus muscle. The periorbital incision should be initiated at the posterior limit of decompression (just anterior to the sphenoid face) and brought anteriorly so that prolapsing fat does not obscure visualization. Parallel incisions are typically made adjacent to the ethmoid roof and orbital floor. To prevent prolapse of the medial rectus muscle and reduce the risk of postoperative diplopia, a sling of fascia overlying the medial rectus muscle may be preserved, while the remainder of the periorbita is removed using angled Blakesley forceps.11 In patients with optic neuropathy, the fascial sling technique is not used to allow maximal decompression. A ball-tipped probe and sickle knife may be used to identify and divide any remaining fibrous bands, which often course superficially between lobules of orbital fat. On completion of the procedure, a generous prolapse of fat into the opened ethmoid and maxillary cavities should be observed (Fig. 20.6). Fig. 20.3 A Blakesley forceps is used to remove bony fragments of the medial orbital wall and expose the underlying periorbita.(From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:952. Reprinted with permission.) Fig. 20.4 A spoon or mastoid curette is used to down-fracture the medial portion of the orbital floor. Only bone that is medial to the infraorbital canal is removed.(From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:953. Reprinted with permission.) Nasal packing is not used to avoid compression of the exposed orbital contents and the optic nerve. The patient is discharged the morning after surgery with a prescription for antistaphylococcal oral antibiotics and instructions to begin twice-daily nasal saline irrigations. At the first postoperative visit one week after surgery, crusting is cleaned from the surgical site under endoscopic guidance. For patients with severe comorbidities, a strong preference for local anesthesia, or in whom surgery is being performed on an only seeing eye, decompression may be accomplished under local anesthesia with sedation.12 This approach allows the surgeon to monitor the patient’s vision throughout the procedure. Sedation may be achieved with an intravenous bolus of propofol (0.4–0.8 mg/kg) before injection of local anesthesia, followed by an infusion of 75 to 95 μg/kg during the procedure. Local anesthesia is administered initially with 4% cocaine pledgets followed by injection of lidocaine 1% with epinephrine 1:100,000 as described for patients undergoing general anesthesia. Patients often report discomfort during incision of the periorbita. This sensation may be relieved by infiltration of a small amount of additional anesthetic solution into the medial orbit. The goals of orbital decompression vary depending on the indication for the procedure. In patients with compressive optic neuropathy, restoration of visual deficits is the key outcome, whereas in patients with corneal exposure or severe proptosis, ocular recession may be the primary endpoint. The rate of improvement after endoscopic orbital decompression for Graves orbitopathy ranges from 22 to 89%.9,13–15 This wide variation in results reflects the diverse patient populations and definitions of improvement. Postoperative deterioration of visual acuity occurs in less than 5% of patients.9,13–15 Ocular recession as a result of endoscopic decompression alone averages 3.5 mm (range 2–12 mm). The addition of concurrent lateral decompression to the endoscopic procedure provides an additional 2 mm of globe recession.14 Fig. 20.5 The exposed layer of periorbital fascia is incised with a sickle knife and removed. (From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:953. Reprinted with permission.) Fig. 20.6 Herniated orbital fat is seen bulging into the maxillary and ethmoid sinuses at the completion of the decompression.(From Metson R, Dallow RL, Shore JW. Endoscopic orbital decompression. Laryngoscope 1994;104:953. Reprinted with permission.) Diplopia is a frequent complication of orbital decompression with 15 to 63% of postoperative patients reporting new-onset diplopia or worsening of preexisting symptoms.8,10,14–17 This complication is believed to be a result of a change in the vector pull of the extraocular muscles. Decompressive surgery rarely alleviates preexisting diplopia. Patients who have diplopia after decompressive surgery frequently require strabismus surgery for correction. All patients should be informed of the possibility of postoperative double vision and the potential need for further surgical intervention. Several methods to decrease postoperative diplopia have been reported. Multiple authors have described the preservation of a strut of inferomedial bone between the decompressed floor and medial wall.13,18 When this strut is maintained, however, it is technically difficult to remove the orbital floor through a purely endoscopic approach. The maintenance of a fascial sling in the region of the medial rectus has been shown to decrease postoperative diplopia.11 This technique provides similar support as the medial strut technique, but allows for endoscopic access to decompress the medial orbital floor. The concept of a balanced decompression (concurrent medial and lateral decompression) has also been shown to decrease postoperative diplopia.15,19,20 When operating for compressive optic neuropathy, techniques designed to limit diplopia may also limit the extent of decompression, and postoperative diplopia often is accepted as a concession to improved vision. Postoperative bleeding after decompression is best approached through endoscopic identification and direct cauterization of the bleeding site. Nasal packing generally is not used so as to avoid pressure on the exposed orbital apex and optic nerve. Postoperative infection is minimized through the use of postoperative antibiotics with staphylococcal coverage. A large maxillary antrostomy and limited bone removal in the frontal recess region minimize the risk of developing postoperative obstructive sinusitis. Epiphora may develop if the maxillary antrostomy is extended too far anteriorly with transection of the nasolacrimal duct. This complication may be treated with an endoscopic dacryocystorhinostomy. Leakage of cerebrospinal fluid, blindness, and hypesthesia along the infraorbital nerve distribution are rare complications that have been reported primarily after nonendoscopic decompression techniques. During endoscopic orbital decompression for treatment of Graves orbitopathy, the maxillary sinus serves as the gateway to the orbital floor. Successful endoscopic decompression depends on the creation of a wide maxillary antrostomy, which provides adequate access for removal of the orbital floor and prevents postoperative sinusitis due to obstruction of the maxillary ostium. • A large maxillary antrostomy must be performed during endoscopic orbital decompression to allow for adequate exposure and access to the medial orbital floor. The wide maxillary antrostomy should allow visualization of the infraorbital canal with a30-degree endoscope. • A large maxillary antrostomy decreases the risk of postoperative sinusitis due to obstruction of the maxillary ostium by herniating fat. • To obtain maximal orbital decompression, the medial orbital floor can be removed as far laterally as the infraorbital canal. • Preservation of the lateral orbital floor during decompression allows for adequate support of the globe and prevents postoperative hypoglobus. • Epiphora may occur following orbital decompression if the maxillary antrostomy is extended too far anteriorly with transection of the nasolacrimal duct. If this complication occurs, it can be treated with an endoscopic dacryocystorhinostomy.
 Surgical Treatment of Graves Orbitopathy
Surgical Treatment of Graves Orbitopathy
 Endoscopic Orbital Decompression
Endoscopic Orbital Decompression
Patient Selection and Work-Up
 Surgical Technique
Surgical Technique
Results
Complications
 Conclusion
Conclusion
The Maxillary Sinus and Surgical Treatment of Graves Orbitopathy
Pearls
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree