 echnologic progress forever changes how things are perceived and accomplished. The ear, nose, and throat (ENT) field is quite different now from what it was just a few years ago. Over the course of my 40 years of ENT practice, I gained extensive experience with treatment methods such as suction diathermy, cryosurgery, radiocautery, and the use of both the carbon dioxide laser and the potassium titanyl phosphate (KTP) laser. Although purportedly the most modern and cuttingedge techniques, carbon dioxide and KTP lasers come with their own set of problems.
echnologic progress forever changes how things are perceived and accomplished. The ear, nose, and throat (ENT) field is quite different now from what it was just a few years ago. Over the course of my 40 years of ENT practice, I gained extensive experience with treatment methods such as suction diathermy, cryosurgery, radiocautery, and the use of both the carbon dioxide laser and the potassium titanyl phosphate (KTP) laser. Although purportedly the most modern and cuttingedge techniques, carbon dioxide and KTP lasers come with their own set of problems.
In 2002, I heard about the characteristics of Fugo blade ablation from the ophthalmology department at my institution. I began to incorporate the Fugo blade into my ENT surgeries. Experience with the Fugo blade has shown that it has none of the disadvantages of standard ENT techniques and in fact offers many advantages.
The Fugo blade is a simple and safe tool to use and is easy to maintain. No special precautions must be taken, nor have my colleagues and I encountered any specific complications related to the device, either during surgery or postoperatively. By virtue of the Fugo blade’s ablation and penetration properties, tissue definition is very good. The heat produced is more localized, so collateral tissue damage is negligible. The Fugo blade has proved to be advantageous over existing forms of treatment (Table 50.1). Additional advantages include its reliability and relatively low cost, compact dimensions, and lightweight portability. Many procedures that once involved overnight or longer stays at a hospital are now treated in an outpatient setting using the Fugo blade.
To date, I have treated a variety of ENT conditions and performed a range of surgical techniques using the Fugo blade with great success (Table 50.2). Several illustrative examples are described below.
The Larynx
Use of the Fugo blade (rather than a laser, with its accompanying fumes) allows the surgeon to effectively concentrate on the laryngeal structures and treat them with minimal tissue excision and minimal rupture of the superficial lamina propria.
Vocal Nodules
Vocal nodules appear on the free edge of the vocal cord at the junction of its anterior one third and posterior two thirds, the location of maximum cord vibration and hence subject to maximum trauma. Nodules can range in size from that of a pinhead to a small pea. Nodules develop as a result of vocal trauma, for example, when a person speaks in unnaturally low tones for prolonged periods or at high intensities. Vocal nodules mostly affect teachers, singers, vendors, or actors and can also be seen in school-age children and adolescents. Patients with vocal nodules report hoarseness, vocal fatigue, and pain in the throat on prolonged phonation.
Table 50.1. Comparison of Conventional Surgical Methods with the Fugo Blade
| Disadvantages of Carbon Dioxide Laser and KTP Laser | Advantages of the Fugo Blade |
| Staff training required. Every staff member in the operating room must don special protective eyewear. | Minimal training required; no special preparation needed before or during surgery |
| Difficult and prolonged learning curve for proper handling | Easy to handle |
| Imprecise and inaccurate skin and soft-tissue dissection | Precise and accurate skin and soft-tissue dissection |
| Poor tissue definition | Better tissue definition |
| Palpable collateral tissue damage | No collateral tissue damage |
| Thermal damage to some tissues (e.g., laryngeal and tracheal cartilage) results in fibrosed tissue. | Laryngeal and tracheal cartilage tissues are easy to divide with minimal damage. |
| Severe postoperative tissue reaction and edema | Minimal bleeding; almost no bleeding from capillaries |
| Slow re-epithelialization | No or minimal postoperative pain and tissue reaction or edema |
| Extensive recovery period | Faster re-epithelization ensures faster healing and recovery. |
| Short recovery period | |
| Better patient compliance with postoperative care and follow-up |
Table 50.2. ENT Conditions Treated and Procedures Performed Successfully Using the Fugo Blade
| Pathology/Condition | Surgical Procedures |
| Branchial sinus | Arytenoidectomy |
| Granuloma of the vocal process | Branchial cyst excision |
| Keloids (ear lobule, chest wall, upper arm) | Division of tongue tie |
| Laryngeal stenosis | Parotidectomy |
| Multiple juvenile laryngeal papillomas | Tonsillectomy |
| Nasolabial cyst | Uvulopalatopharyngoplasty |
| Pharyngeal stenosis | |
| Reinke’s edema | |
| Septal papilloma | |
| Tracheal stenosis | |
| Tracheal stomal papilloma | |
| Ventricular cyst | |
| Vocal nodule | |
| Vocal polyp |
Early cases of vocal nodules can be treated conservatively by educating the patient about proper use of the voice. Surgery is required for large or long-standing nodules in adults.
Surgical Technique: Microlaryngeal Surgery with the Fugo Blade
- Inpect and photograph the lesion to be treated (Fig. 50.1).
- Ablate the nodule with the laryngeal probe of the Fugo blade (Fig. 50.2). The blade delivers plasma energy at the tip with outstanding precision and without clinically visible collateral damage. Even the surrounding normal epithelium is unaffected.
- It takes only 5 to 7 minutes to very gradually remove the nodule or polyp.
- To prevent recurrence of the nodule, penetrate the subepithelial space to a depth of 0.5 mm.
- It takes only 5 to 7 minutes to very gradually remove the nodule or polyp.

Figure 50.1. Vocal nodule before, during, and after surgery with the Fugo blade.

Figure 50.2. Fugo blade microlaryngeal probe.
Postoperative Management
Postoperatively the vocal cord looks slightly swollen but heals and returns to normal within 2 weeks. Postoperative pain is nonexistent, and the patient is discharged the same day. If a laser were used for the same purpose, the recovery period would be much longer. The nodule has not recurred in any of the 11 cases I have treated with the Fugo blade.
Multiple Juvenile Laryngeal Papillomas
Juvenile-onset laryngeal papillomas are the most common cause of laryngeal tumors in children. They are caused by virally induced epithelial proliferation (human papillomavirus types 6 and 11). They tend to disappear after puberty, which demonstrates hormonal involvement to some extent. Papillomas appear as glistening, fleshy, wartlike, white irregular growths that are sessile (occasionally pedunculated), friable, and bleed easily (Fig. 50.3). They are benign and are seen mostly on the true and false vocal cords and the epiglottis. If they are allowed to advance, however, known complications include spreading to other sites in the larynx and tracheobronchial tree and to the nasopharynx and nasal vestibule, respiratory obstruction, and, rarely, malignant degeneration.
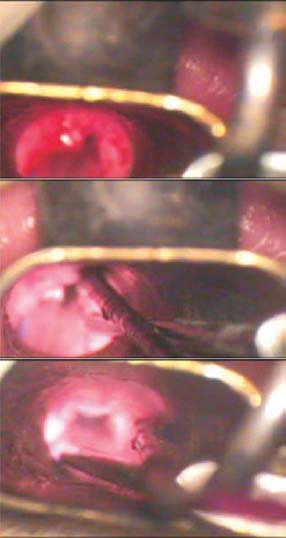
Figure 50.3. Laryngeal papilloma before, during, and after surgery with the Fugo blade.
Laryngeal papillomas are undoubtedly one of the most challenging benign conditions facing the laryngologist, especially because of their propensity to recur. Many different methods, including conventional surgery; laser surgery; medical therapy with indole-3-carbinol, α-interferons, and acyclovir; and even photodynamic therapy have been used to treat patients with laryngeal papillomas, yet the multitude of methods seems to reflect the inability of a single individual method to control the disease.
The Fugo blade has been singularly helpful in treating this condition. It is very easy to ablate the papillomas in depth without damaging the submucosa. Tissue definition is good and precise dissection is possible. Healing takes place within a week and without scarring. Postoperative edema is minimal, and voice quality returns to near normal in virtually all patients. With lasers, 10 to 15 treatment sessions are necessary just to control the condition. With the Fugo blade however, 3 to 5 treatments are enough to control and even eradicate the disease. I have successfully treated 4 cases of juvenile laryngeal papillomas using the Fugo blade.
Laryngeal Cyst/Anterior Saccular Cyst
In the anterior ventricle of the larynx lies the sacculus laryngis, also known as the laryngeal saccule. This process contains numerous mucous glands, and its role is to express secretions to lubricate the vocal fold. Obstruction of the saccule causes secretion retention and saccule distention, which presents as a cyst in the laryngeal ventricle. Because there is no connection with the intralaryngeal lumen, it is called a “saccular cyst.” It generally presents in the anterior part of the ventricle or posteriorly into the false vocal cord of the epiglottic fold. Patients generally present with a history of hoarseness. I have treated two such cases with the Fugo blade.
Surgery is done under general anesthesia. The standard method is marsupialization, which is an insufficient treatment, because the cyst recurs in many patients. The effective treatment is complete excision of the cyst (Fig. 50.4). A recurrence requires a more extensive external approach.

Figure 50.4. Ventricular cyst before, during, and after surgery with the Fugo blade.
Complete dissection of the laryngeal cyst is easy with the Fugo blade. Bleeding is negligible. The Fugo blade easily reaches the required depth for dissection, with clinically little collateral damage. Re-epithelization is rapid.
The Trachea
The use of Fugo blade to treat conditions of the trachea is illustrated with a few examples.
Tracheal Stomal Papillomas
When the Fugo blade is used to excise tracheal stomal papillomas, burning and charring of the tissue is remarkably absent (Fig. 50.5).
Tracheal Stenosis
Submucosal dissection of fibrous tissue using the plasma knife has made it possible to achieve the desired lumen size with the least amount of damage to the mucosa (Fig. 50.6).
Figure 50.5. Tracheal stomal papilloma before, during, and after surgery with the Fugo blade.
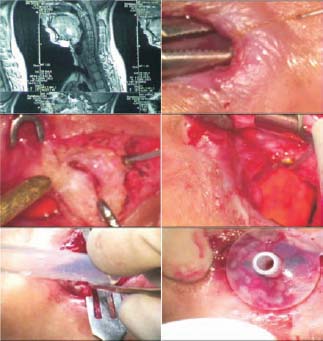
Figure 50.6. Computed tomographic scan showing the extent of tracheal stenosis. The surgical photographs show incision of the skin, exposure and cutting of the cricoid and tracheal cartilages with the Fugo blade, and dissection and excision of the fibrous tissue.
Oral Cavity and Oropharynx
Tonsillectomy
My colleagues and I first performed a tonsillectomy with a Fugo blade on a 40-year-old woman with tonsillitis. Since then, we have done many more tonsillectomies on both adults and children and in some cases, on patients with large tonsils that interfered with the patient’s swallowing and breathing, sometimes severely enough to cause sleep apnea.
Surgical Technique: Tonsillectomy
- Make an incision with the Fugo blade only in the mucous membrane.
- Separate the superior pole from the bed by separating the fibrous bands by just touching the activated Fugo blade tip to the tissue.
- Cut the mucosa of the posterior pillar with the Fugo blade. The incision should be deep enough to reach the surgical capsule of the tonsil.
- Use the Fugo blade to separate the tonsil and its capsule from the surrounding peritonsillar tissue.
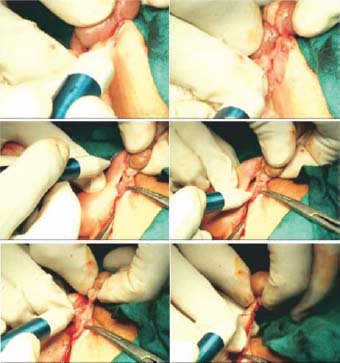
- Gripping the tonsil by its upper pole, continue to draw the tonsil toward the midline and continue the dissection with the Fugo blade to reach the lower pole. At this point, the firm fibrous fold is very easy to divide using the Fugo blade without much bleeding. It is very easy to dissect the tonsil completely (Fig. 50.7). However, it is important to note that the cutting power of the Fugo blade is slow, and as a result it does take longer to remove the tonsils.
- Minor bleeding is controlled quickly and effectively with the Fugo blade tip Occasionally, you may need to suture the paratonsillar vein with a silk thread.
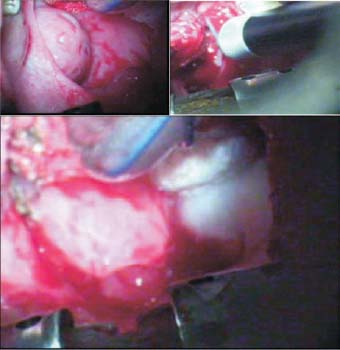
Figure 50.7. Tonsil before, during, and after surgery with the Fugo blade. The tonsillar bed is clean and is devoid of charring or tissue damage.
Postoperatively less facial edema, inflammation, and slough formation is seen than with conventional dissection methods. Sloughing will disappear in about 10 to 12 days. Almost no tissue reaction occurs, and scarring of the tonsillar bed is minimal. Compared with micro-electrocautery tonsillectomy and laser tonsillectomy, the Fugo blade’s thermal collateral damage is negligible, hence postoperative pain, slough formation, and complications such as hemorrhage and tissue fibrosis are significantly reduced. Patients treated with the Fugo blade return to their normal diet sooner than those who undergo bluntdissection tonsillectomy.
Superficial Parotidectomy
As the first steps in superficial parotidectomy, it is very easy to dissect and raise a skin flap with the Fugo blade. Tissue dissection is precise, bleeding is minimal, and no collateral tissue damage occurs. A standard parotidectomy skin incision is shown in Figure 50.8.
TECHNIQUE
Anesthesia
Administer general anesthesia.
Surgical Technique: Superficial Parotidectomy
- Make a standard parotidectomy skin incision (Fig. 50.8).
- Deepen the incision below the mandible through the platysma down to the level of (but not into) the deep cervical fascia.
- Using the Fugo blade, raise the skin and subcutaneous tissue flap anteriorly and the platysma inferiorly. Use silk sutures to hold the flaps. Hemostasis is effectively obtained with the plasma knife itself.
- The greater auricular nerve lies on the deep cervical fascia investing the sternomastoid muscle. Separate the anterior border of the sternomastoid muscle using the Fugo blade from the posterior border of the parotid gland. Divide the greater auricular nerve at the point where it crosses onto the parotid gland.
- Further up, separate the gland from the mastoid process and the cartilaginous external meatus under the microscope.
- Now deepen the sulcus by sharp dissection to expose the posterior belly of the digastric muscle and trace the muscle upward and backward to the point where it dips beneath the mastoid process. At this stage, identify the main trunk of the facial nerve. Deepen the sulcus between the parotid gland on the one hand and the external meatus and mastoid process on the other so that the edge of the bony meatus can be identified.
- At this stage, use the hemostat to splay out the bands in the sulcus and seek the facial nerve by blunt dissection. Insert a hemostat into the gland immediately superficial to the main trunk of the nerve and open it up in order to establish a plane. Insert a suitable retractor into the plane to retract the superficial lobe of the parotid forward and to allow identification of the bifurcation of the nerve. Slide the hemostat over the upper division and open the blades.
- Incise the glandular tissue overlying the posterior blade using the Fugo blade upward and backward to divide the posterior border of the gland. Identify all branches of the facial nerve and divide the glandular tissue superficial to the nerve. (It is very easy to dissect this glandular tissue; it feels like you is cutting a piece of cake.) In this way, the superficial lobe is mobilized up to the upper border of the gland. Repeat the procedure to mobilize it from the zygomatic arch.
- Then divide the lower half of the posterior and the inferior border using the same technique along the inferior division and consecutive branches.
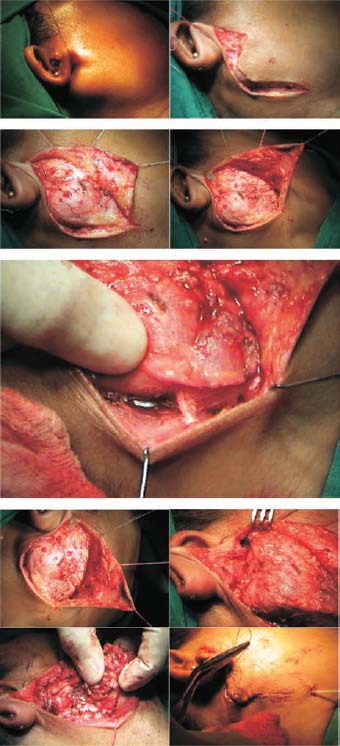
Figure 50.8. Superficial parotidectomy with the Fugo blade. The skin flap is raised, the greater auricular nerve is divided, the parotid gland is separated from the surrounding structures, and the facial nerve is exposed and identified. The tumor tissue is excised with the Fugo blade, preserving the facial nerve and its branches.
Postoperatively not much seepage occurs in the draining chamber wound. It heals nicely within 1 week. No complications have occurred during any of the surgeries we have done.
Uvulopalatoplasty with Tonsillectomy
Uvulopalatoplasty is commonly used to alleviate snoring. Uvulopalatoplasty with tonsillectomy (Fig. 50.9) is used to treat snoring accompanied by mild obstructive sleep apnea.

Figure 50.9. Excision of uvula. Division of the soft palate muscle along with tonsillectomy is done with the Fugo blade with no charring of tissue.
Reduced postoperative pain, fewer complications, and hence less morbidity and better compliance are some of the advantages of using the Fugo blade in this procedure. Postoperative hemorrhage and palatal insufficiency are lower; the patient heals more quickly as compared with conventional surgical methods. Finally, standard laser-assisted uvulopalatoplasty required multiple sittings to stiffen the palate and achieve the required results. The Fugo blade makes this a one-stage procedure.
Pharyngeal Stenosis
CASE STUDY
A 45-year-old woman was involved in motorcycle accident in which she was partially strangled by the dupatta (a traditional scarf worn around the neck) she was wearing. She suffered injuries to the larynx, including fracture of the hyoid bone, thyroid cartilage, and cricoid cartilage and avulsion of the epiglottis. There was history of pain around the neck and immediate respiratory distress for which an emergency tracheostomy had been performed. The patient later presented with dysphagia, for which nasogastric feeding was started. Then the patient underwent pharyngeal dilation using a laser. Three attempts were made to relieve the stenosis, but each attempt led to further worsening of the condition. After this, the patient had to undergo a feeding jejunostomy. She was advised to undergo a total laryngectomy as well. The patient presented to me after this advice. The computed tomographic (CT) scan showed complete closure of the pharynx with a normal glottis. The supraglottic portion of the larynx was unidentifiable (Fig. 50.10).
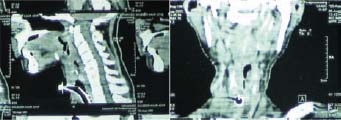
Figure 50.10. CT scans showing severe pharyngeal stenosis.
The patient underwent exploration of the neck with the Fugo blade and complete excision of the scar tissue (Fig. 50.11).
At present, the patient still has a minitracheostomy to maintain a normal airway. She has undergone decannulation repeatedly, but with little success because the jejunal graft, being a muscular tube, remains collapsed most of the time. She can swallow normally and has good, understandable speech. To speak, she must block the tracheostomy tube with her thumb. However, the patient is otherwise pursuing a normal life with no difficulty with regard to her respiratory, speech, and deglutitory functions.
We believe that the successful management and cure of this case is entirely due to the distinct advantages (better tissue definition, negligible thermal damage and scarring, better healing, less fibrosis) that the Fugo blade offers over conventional surgical methods and lasers.
The Ear, Nose, and Neck
Keloid on the Ear Lobule
The Fugo blade has proved to be an effective and easy instrument in the excision of keloids of the ear lobule (Fig 50.12) (and at other sites, including the chest wall and upper arm). Compared with conventional treatment methods, recurrence of keloids is negligible when treated with the Fugo blade. Several cases of recurring keloids were followed over a period of 3 years after surgery with a Fugo blade; not a single case showed evidence of recurrence.
We have also used the Fugo blade to excise a preauricular sinus.
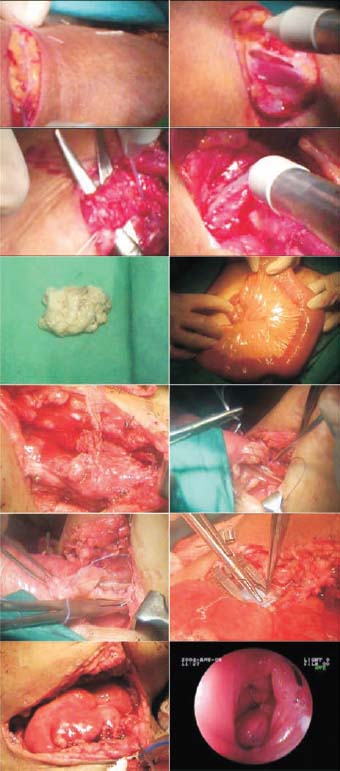
Figure 50.11. A jejunal graft was used for reconstruction of a muscular tube from the base of the tongue to the upper end of the esophagus and was also stitched to the soft tissue around the glottis.
Figure 50.12. Steps of operation showing excision of a keloid using the Fugo blade.
Other Sites
I have successfully used the Fugo blade to treat septal papilloma and to excise nasolabial cysts, branchial cysts, and branchial sinus.
Summary
Although originally created for ophthalmic applications, the Fugo blade has proved to be an ideal substitute to enable ENT surgeons to provide patients with all the benefits of laser-assisted ENT surgery. Current applications of lasers can be damaging to the delicate vocal fold, especially in cases of juvenile laryngeal papillomas. The advent of the Fugo blade has led to better anatomical and physiologic results. It has definitely improved the quality of patient care.
Suggested Reading
Feder RJ. Laryngeal granuloma as a complication of CO2 laser. Laryngoscope. 93:944–945.
Myssiorek D, Persky M. Laser endoscopic treatment of laryngoceles and laryngeal cysts. Otolaryngol Head Neck Surg. 1989;100:538–541.
Ossoff RH, Werkhaven JA, Dere H. Soft-tissue complications of laser surgery for recurrent respiratory papillomatosis. Laryngoscope. 1991;101:1162–1166.
Rosen CA, Woodsen GE, Thompson JW, et al. Preliminary results of the use of indole-3-carbinol for recurrent respiratory papillomatosis. Otolaryngol Head Neck Surg. 1998; 118:810–815.
Shikowitz MJ, Abramson AL, Freeman K, et al. Efficacy of DHE photodynamic therapy for respiratory papillomatosis: immediate and long-term results. Laryngoscope. 1998; 108:962–967.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree