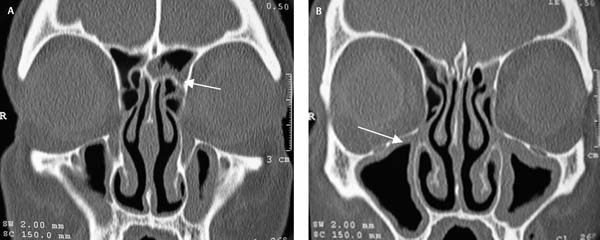
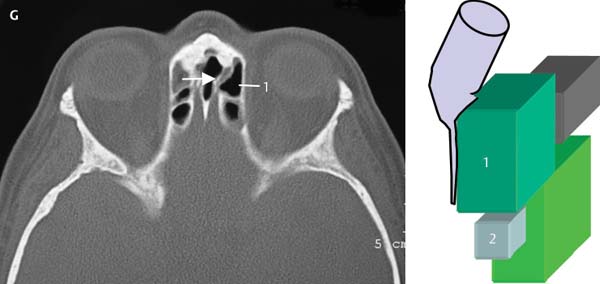
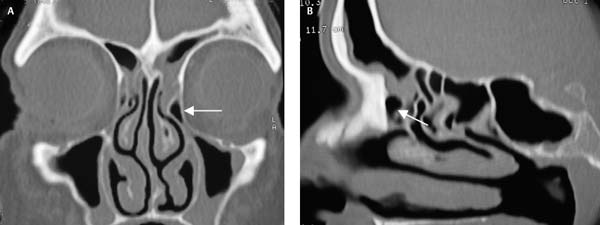
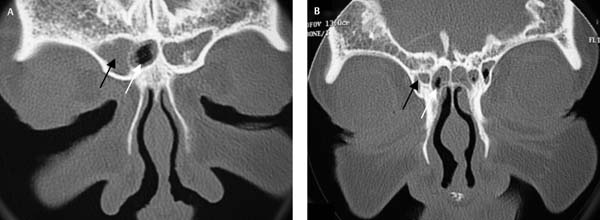
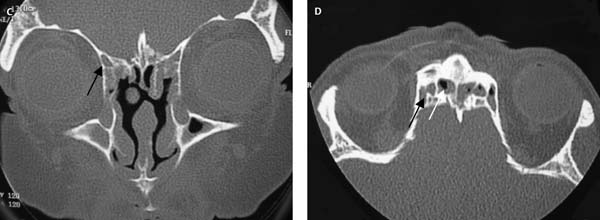
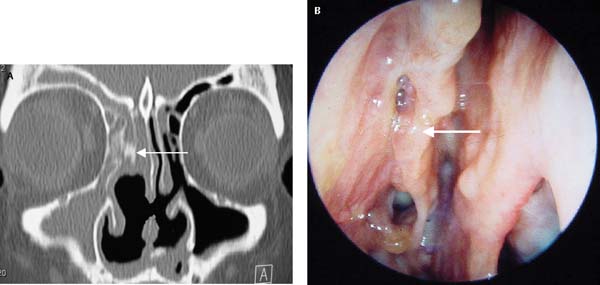
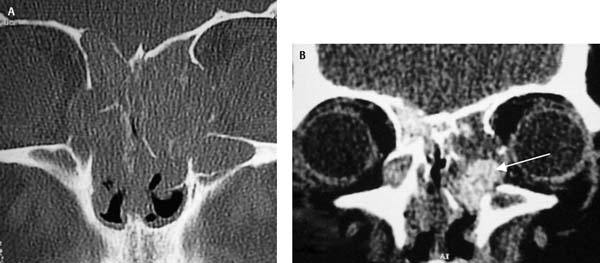
7 The frontal recess has always been considered to be the most difficult area to dissect.1–4 This is largely due to its location behind the beak of the frontal bone.5 There are three major philosophies regarding the management of disease of the frontal recess and sinus. The minimal invasive sinus technique (MIST) advocates management of the maxillary sinus and associated transitional spaces (hiatus semilunaris and ethmoidal infundibulum) without performing surgery in the frontal recess.6–8 This philosophy states that treatment of the maxillary sinus and associated transitional spaces will result in clearance of the frontal recess and sinus disease. There are few published papers supporting this theory and all publications come from the same group of investigators.6–8 Until there is substantial evidence that this approach works for a broad spectrum of frontal sinus and frontal recess disease, we do not advocate this approach. The second philosophy is that the frontal recess and frontal sinus should only be operated on if there are symptoms that can be directly ascribed to the frontal sinus such as frontal headache and pain. Although we agree that surgery on a diseased frontal sinus or recess that is symptomatic is appropriate, we disagree that this is the only indication for surgery in this region. Patients who present with nasal obstruction, postnasal drip, purulent rhinorrhea and anosmia, and who have radiological disease in the frontal sinus or recess need to have this region surgically addressed. These patients have their diseased maxillary sinuses, ethmoid, and sphenoid sinuses addressed and it makes no sense that just because they do not have localized frontal pain or tenderness, that the frontal sinus should not be addressed as well. It has been well recognized that retained or residual cells in the frontal recess/sinus is one of the most common causes of endoscopic sinus surgery (ESS) failure.1,2 In this chapter we present our graduated approach to surgery of the frontal recess and sinus. In the easy frontal recess and sinus, simple maneuvers in terms of endoscopy and surgical access (axillary flap) are advocated and are, in most cases, sufficient to allow clearance of the frontal recess and frontal ostium. In the difficult frontal recess or sinus, the additional technique of frontal sinus mini-trephination is presented. These difficult patients may also benefit from the surgeon having computer-aided surgical navigation available. The mainstay of our surgical technique is the axillary flap technique. This technique has similarities to the frontal sinus rescue procedure described by Kuhn et al.9 in that mucosal flaps are raised during the surgery on the frontal ostium. However, the major difference is that the frontal sinus rescue procedure is designed for the management of patients who have failed previous standard ESS and have a stenosed frontal ostium. The axillary flap technique is designed for all patients undergoing frontal recess or sinus procedure including previously operated patients. The central concept of the axillary flap procedure is removal of the anterior wall of the agger nasi cell. This is not new and was described by May and Schaitken10 as part of their naso-frontal approach (NFA 1) to the frontal sinus. Schaefer and Close11 have advocated a similar approach with removal of the bone above the insertion of the middle turbinate. The major difference between these approaches and the axillary flap approach is the elevation of a mucosal flap which can be replaced at the end of the procedure to cover the raw exposed bone that is seen after removal of the anterior wall of the agger nasi cell. This prevents granulation tissue from forming over the exposed bone with subsequent scarring and cicatrization of this area. Such scarring can pull the upper extension of the middle turbinate laterally and close off the anterior aspect of the frontal recess. This may in turn lead to blockage of the frontal outflow tract and result in recurrent frontal sinusitis. May and Schaitkin advocated enlarging the frontal ostium in their NFA II and III approaches.10 This is unnecessary and not advocated in the vast majority of patients as the removal of residual cells within the frontal recess with the exposure of the frontal ostium is usually sufficient to achieve resolution of frontal sinusitis. It is our philosophy that where patients have cells in the frontal recess or frontal ostium that obstruct the outflow of the frontal sinus, that these should be removed without enlarging the frontal ostium. Even very small frontal ostia can function well if their outflow pathway is not obstructed and the patient should be given the opportunity to see if the natural size of their frontal ostium is sufficient. In some patients, especially those with severe mucosal disease, this ostium may become edematous and obstruct and, if this causes symptoms, then enlargement of the ostium is indicated. However, this occurs in the minority of cases and it’s not possible to predict which patients with a particular frontal ostium size will obstruct and become symptomatic. In most patients the only way to enlarge a frontal ostium is with a drill. Drilling in the frontal ostium without creation of the largest possible ostium is likely to result in an intense fibrous reaction from the exposed raw bone and in most cases will increase the likelihood of postoperative scarring and stenosis. As can be seen in Chapter 9, enlargement of the frontal ostium is usually done with a modified Lothrop procedure/Draf 3/frontal drillout and very rarely with a Draf type 2 (unilateral enlargement of the frontal ostium) procedure, due to the increased incidence of fibrosis and stenosis seen with unilateral drilling on the frontal ostium.12 This is especially true for patients who have severe mucosal disease and in whom the inflammatory process continues in the postoperative period.13 Our philosophy is that a patient who has undergone appropriate medical therapy (including systemic steroids) and is then found to have mucosal thickening in the frontal recess or sinus should have all cells cleared from the frontal recess and frontal ostium exposed (Fig. 7.1).13–16 In patients without significant disease of the frontal recess (Fig. 7.1), only the diseased sinuses are addressed and the frontal recess is left untouched. Partial surgery of the frontal recess is never indicated. If only the roof of the agger nasi cell is removed or one of the frontal ethmoidal cells is removed, scarring is likely to result. The cells in the frontal recess are usually in close approximation and partial clearance of cells will very likely result in adhesions forming between these closely approximated surfaces with obstruction of the drainage pathway of the frontal sinus. Our philosophy is an all or nothing approach. The frontal recess is either left entirely alone or all the cells are removed from the recess with visualization of the frontal ostium. In a patient who is to undergo frontal recess clearance and sinus surgery, the computed tomography (CT) scans need to be carefully assessed and the three-dimensional (3D) reconstruction of the anatomy performed (see Chapter 6). Once the surgeon has a clear understanding of the anatomy, a surgical plan should be formulated. An example of such a plan is presented in Fig. 7.2. In this patient, after uncinectomy and middle meatal antrostomy, an axillary flap is performed to expose the anterior face of the agger nasi cell. This is removed with the Hajek Koeffler punch (Karl Storz, Tuttlingen, Germany) and the agger nasi cell visualized. The malleable frontal sinus curette* (Medtronic ENT, Jacksonville, FL) is placed posteromedially to the agger nasi cell’s posterior wall and roof, and the cell removed by fracturing it forward. The resultant debris is removed with a microdebrider. The residual roof of the agger nasi cell is cleared and the type 3 (T3) cell visualized. After careful assessment of the axial scans we know that the frontal sinus drains medially around this cell and the suction curette is slid along this drainage pathway into the frontal sinus and the cell fractured laterally and removed. An angled microdebrider blade is used to clear debris, and small residual bony fragments are cleared with giraffe forceps and the malleable frontal sinus hooked probe* (Medtronic ENT). The frontal ostium is visualized but all mucosa around the frontal ostium is preserved. Fig. 7.1 In coronal CT (A) note the mucosal thickening in the left frontal sinus (white arrow) and recess with a normal right frontal sinus and recess. In coronal CT (B) note the mucosal thickening of the right maxillary sinus (white arrow). In this patient the left frontal recess would be cleared of cells and the frontal ostium identified while on the right side no surgery would be performed in the frontal recess. Both maxillary sinuses would be surgically addressed. Fig. 7.2 The T3 cell is numbered 1 in the coronal CT scans (A–C) and the parasagittal scan (D) and the agger nasi cell is numbered 2. In the axial CT scans (E–G), the T3 cell is numbered 1 with the frontal sinus drainage pathway medial to this cell (white arrow). Surgeons should recognize potentially difficult frontal recesses by studying the CT scans at the time the patient is listed for surgery.13–16 Recognition of potential difficulties can aid the surgeon when discussing the likelihood of success of the procedure and the probable need for further surgery such as enlargement of a very narrow frontal ostium. In addition, the likelihood of possible ancillary procedures, such as a mini-trephine of the frontal sinuses, can be assessed and discussed with the patient. The need for computer-aided surgical navigation is assessed at the same time. The surgeon should assess the degree of difficulty of the surgery and if the case is too difficult for their level of expertise, the patient should be referred to a specialist rhinologist. The following features should be sought on the CT scan. Patients who have a wide anteroposterior (AP) diameter will usually have a technically easier operation and will in most cases have a better prognosis for maintenance of health of the sinuses after surgery. This reflects the postoperative size of the frontal ostium that can be achieved without drilling on the ostium. Figure 7.3 illustrates a patient with a wide AP diameter compared with a patient with a narrow AP diameter. Note the space available to operate in the wide diameter patient. Single agger nasi cell is the simplest configuration in the frontal recess and, after removal of this cell, the frontal ostium can be identified (Fig. 7.4). A simple cell configuration of one or two associated frontal ethmoidal cells is also relatively easy to deal with in the frontal recess. Even after an axillary flap approach these cells can be difficult to access and surgery often requires an angled endoscope thereby increasing the difficulty of the surgery. In addition a high T3 or type 4 (T4) cell can be confused with the frontal sinus and the CT scans should be reviewed to ensure that the drainage pathway of the frontal sinus is identified and instrumented. These cells need to be removed to allow adequate ventilation and drainage of the frontal sinus. An example of this is given in Fig. 7.5. This can be problematic if the frontal sinus is completely opacified and the surgeon wishes to ensure the pus or inspissated mucus is cleared from the sinus. Failure to clear thick mucus or pus from the frontal sinus may allow the inflammatory process to continue in the postoperative period in the region of the frontal ostium. This delays the healing process and can increase the risk of scarring and adhesions in the frontal region. An example of a small frontal sinus ostium is presented in Fig. 7.6. Fig. 7.3 (A–C) The patient has a very narrow anteroposterior (AP) diameter. (A) The clue to the narrow AP diameter is the thick bone (white arrow) on either side of the frontal ostia, which is not present in equivalent coronal CT of the patient with a wide AP diameter (D). In the parasagittal scans (B,E) the difference between (B) a narrow AP and (E) a wide AP is apparent (white arrows). On the axial CT scans (C,F) the difference in the AP diameter is again apparent (white arrows). Fig. 7.4 In coronal CT scan (A) the left frontal recess has a single agger nasi cell (white arrow). This can be clearly seen on the parasagittal scan (B, white arrow). This is the simplest configuration seen in the frontal recess. Fig. 7.5 Bilateral type 3 cells are seen obstructing the frontal ostium. The parasagittal view is of the right side. Fig. 7.6 This patient has a combination of an intersinus septal cell (white arrow) and a small frontal sinus on the right (black arrow) and on the left. The small drainage pathway of the frontal sinus on the right is marked with a black arrow (B–D). New bone formation in the region of the frontal ostium and recess often indicates osteitis of the surrounding bone. If the new bone obstructs the frontal ostium, removal will often leave vascular and inflamed exposed bone, which will usually produce significant fibrosis and scar tissue. Restenosis and obstruction of the frontal ostium will often result. An example of the CT scan appearance of new bone formation is shown in Fig. 7.7. Cultures of removed bone should be performed and patients should then be started on appropriate antibiotics. Consideration should also be given to suppressing the inflammatory response during the healing period. This can be done by giving a 3-week course of oral steroids. Alternatively, or in combination with the oral steroids, the mini-trephine cannulas can be left in place for 3 to 4 days postoperatively and the frontal sinuses irrigated with prednisolone drops after saline douching. This serves two purposes as it keeps the frontal ostium clear of blood clot (which can contribute to fibrosis and scarring) and the prednisolone diminishes the inflammatory response in the immediate postoperative period. Previous surgery, especially amputation of the middle turbinate with lateralization of the remnant with associated scar tissue formation, can make exposure of the frontal ostium difficult. Diagnosis is made both on the CT scan appearance and on endoscopy. The CT scan can show residual cells and new bone formation and endoscopy can confirm the presence of scar tissue in the frontal recess. An example is shown in Fig. 7.8. Some patients may have extensive and severe disease in the frontal recess (Fig. 7.9). In this example the patient has allergic fungal sinusitis with expansion of the frontal recess and double densities visible on soft tissue settings (white arrow). The frontal recesses in this patient were filled with highly vascular polyps and inspissated fungal material. Not only were the normal anatomical landmarks distorted in this patient but there was extensive bleeding in the frontal recess as the polyps were removed. As previously stated such vascularity can significantly increase the degree of difficulty for the surgeon during removal of the polyps and cells, and during identification of the frontal ostium. Patients who have previously had resection of their middle turbinates can be difficult to manage as the absence of the middle turbinate has removed the most important operative landmark (Fig. 7.10). Fig. 7.8 The amputated right middle turbinate is marked with a white solid arrow in both the CT scan and on the endoscopy picture. The uncinate remains and abuts the retained anterior ethmoid cells obstructing the drainage of the frontal sinus. On the endoscopic view significant scarring is seen between the lateralized residual middle turbinate and lateral nasal wall (uncinate). If there are polyps present, identification of the residual middle turbinate can be difficult (Fig. 7.11). The first step is to identify the maxillary ostium and to clear the maxillary sinus of polyps using the maxillary trephination procedure if necessary (Chapter 5). This will allow positive identification of the lamina papyracea, which is an important landmark in the further dissection of the frontal recess. The next step is to gently debride the polyps to reveal the underlying bony structures—the septum, olfactory recess, residual middle turbinate, and posterior bony choanae. If the anatomy is still unclear then the polyps in the region of the posterior bony choanae and the anterior face of the sphenoid should be removed. The natural ostium of the sphenoid is usually ~12 mm above the bony posterior choanae. The microdebrider blade is 4 mm and this can be used to measure 12 mm from the posterior bony choanae. A useful additional landmark is the roof of the maxillary sinus which can be used as a guide to enter the sphenoid. Harvey et al.17 have shown that a horizontal line taken from the maxillary sinus roof onto the anterior face of the sphenoid provides a safe point of entry into the sphenoid. Once the polyps in this region are cleared, the residual superior turbinate may come into view. If this has also been previously resected, then the polyps should be cleared from the skull base. The fovea ethmoidalis and olfactory fossa are normally in the same horizontal plane in this posterior region of the ethmoids and gentle removal of polyps (without bone removal) should safely expose the skull base and residual superior turbinate. The previously identified lamina papyracea is an important additional landmark. The next step is to identify the ostium of the sphenoid sinus (the method is described in Chapter 8) and enlarge the natural ostium of the sphenoid. This will allow the skull base to be positively identified and the dissection can then be brought along the skull base anteriorly. The surgeon needs to check the CT scan to identify the position of the anterior ethmoid artery and whether it is suspended within a mesentery or not. Using the lamina papyracea as the lateral landmark, the skull base as the superior landmark, and the beak of the frontal maxillary process as the anterior landmark, the frontal recess can be identified. In most patients a small stump of residual middle turbinate can be seen and an axillary flap is performed and the axilla opened with a Hajek Koffler punch. Now that all the landmarks for the frontal recess are established, the clearance of the frontal recess can continue according to the 3D reconstruction of the anatomy of that recess with localization of the frontal sinus drainage pathway and stepwise removal of each remaining cell in the frontal recess.
Surgical Approach to the Frontal Sinus
and Frontal Recess
 Which Patients Are Suitable for Frontal Recess and Frontal Sinus Surgery?
Which Patients Are Suitable for Frontal Recess and Frontal Sinus Surgery?
 Assessing the Frontal Recess and Frontal Sinus Prior to Surgery
Assessing the Frontal Recess and Frontal Sinus Prior to Surgery
Identifying the Easy from the Difficult Frontal Recess and Sinus
Narrow versus Wide Anteroposterior Diameter of the Frontal Ostium
Single Agger Nasi Cell or Simple T1/2 Configuration (Videos 10 to 14, 18, and 19)
Frontal Ethmoidal Type 3 and 4 Cells Obstructing the Frontal Sinus Ostium (Videos 15, 16, 20, and 21)
Small Frontal Sinus with Poorly Pneumatized Agger Nasi Cells and Small Frontal Ostium
New Bone Formation in the Region of the Frontal Ostium
Previous Surgery with Scarring of the Frontal Recess
Extensive Disease in the Frontal Recess
Resected Middle Turbinates and Patients with Few or No Operative Landmarks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree