Superficial Keratectomy
Dasa V. Gangadhar
Kenneth R. Kenyon
Michael D. Wagoner
Superficial keratectomy involves the surgical removal of subepithelial fibrous membranes and/or anterior corneal opacities that occur in a variety of corneal degenerative and dystrophic conditions. In this chapter the indications, surgical technique, postoperative management, conditions appropriate for treatment, and therapeutic alternatives to this noninvasive minor operative procedure are discussed.
INDICATIONS
A variety of corneal dystrophies, degenerations, and injuries have pathologic changes limited to the anterior cornea. More specifically (and as described in the following sections), those conditions affecting the epithelium, subepithelium, and basement membrane regions are particularly amenable to superficial keratectomy. The most common general indications for performing superficial keratectomy include decreased vision from either corneal opacification or irregular astigmatism and/or recurrent erosions not amenable to more conservative therapies.
SURGICAL TECHNIQUE
Surgery is performed with the aid of an operating microscope in the operating room designated for minor procedures. Local anesthetic consisting of topical proparacaine or tetracaine is usually sufficient. Retrobulbar or peribulbar anesthesia is very rarely necessary. Treatment is limited to the area of superficial corneal abnormality and is not carried out broadly over the entire corneal surface unless the entire cornea is involved. Since these abnormal areas can be subtle in appearance, they must be carefully identified and delineated preoperatively by slit lamp biomicroscopy. An abnormal fluorescein staining or break-up pattern is useful to disclose irregularity of the overlying tear film, as is corneal topography to demonstrate irregular astigmatism.
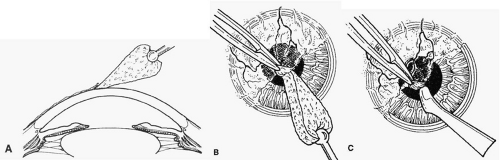
The corneal epithelium is removed over the involved area by gently scraping with a dry cellulose sponge (Weck-cel) or a disposable scarifier blade (Grieshaber 681.01 or Beaver 59). After epithelial removal, the surface should be kept dry to facilitate visualization of subepithelial fibrous plaques or focal accumulations of aberrant basement membrane material. With the aid of a dry cellulose sponge, cleavage planes between the subepithelial fibrous tissue and Bowman’s layer can often be located and exploited. After an edge of the subepithelial fibrous membrane is identified, the tissue can be stripped and peeled with the aid of jeweler’s forceps, frequently as a continuous sheet, thereby leaving Bowman’s layer unharmed. A scarifier may be used to gently scrape or dissect more firmly adherent tissue. Sharp incision or dissection should be avoided to prevent damage to the underlying Bowman’s layer or stroma. The cleared corneal surface can be polished with a cellulose sponge or lightly scraped with a scarifier (Fig. 1).1
Postoperatively, antibiotic ointment is applied and the eye is pressure-patched for 24 hours. Thereafter, antibiotic ointment is initially applied four times a day and reduced in frequency over 2 weeks. Re-epithelialization is usually complete in 5 to 7 days. Contact lens wear can be resumed after 2 weeks.
CONDITIONS APPROPRIATE FOR SUPERFICIAL KERATECTOMY
EPITHELIAL BASEMENT MEMBRANE DYSTROPHY (MAP DOT-FINGERPRINT DYSTROPHY)
Epithelial basement membrane dystrophy is the most common corneal dystrophy, affecting approximately 2% of the population.2 Although most patients remain asymptomatic, about 10% experience recurrent corneal erosions as a consequence of faulty attachment complexes. These attachment complexes consist of hemidesmosomes of the basal epithelial cells, the underlying basement membrane, and the subadjacent anchoring fibrils of Bowman’s layer.3 After an erosion, persistence of devitalized epithelium and fragments of basement membrane may inhibit normal re-epithelialization and formation of secure attachment complexes. Simple superficial debridement for removal of abnormal epithelium and basement membrane, thereby leaving a smooth substrate of Bowman’s layer, can be performed at the slit lamp. The adjacent normal epithelium can resurface this area, allowing formation of competent attachment complexes and resulting in prompt cessation of erosive symptoms with much reduced frequency of recurrences.4,5,6 This procedure can be employed if more conservative measures (i.e., lubricants, patching, bandage contact lenses) fail in halting the erosions.
A smaller subset of patients with epithelial basement membrane dystrophy experience reduction of vision and/or recurrent erosions from the extreme deposition of an abnormal basement membrane and fibrillar collagenous material between the epithelium and Bowman’s layer.2 This material may lead to irregular astigmatism and abnormal tear breakup. Patients typically complain of monocular visual distortion, diplopia, or “ghost images.” By performing superficial keratectomy, this abnormal material can be readily removed, leaving behind a smooth substrate of intact Bowman’s layer. After re-epithelialization a smooth surface is re-established with the elimination of irregular astigmatism.
REIS-BÜCKLERS DYSTROPHY
Reis-Bücklers’ dystrophy is an autosomal dominant condition characterized by the extensive accumulation of a fibrous subepithelial tissue that largely replaces Bowman’s layer.2 Secondarily defective epithelial attachment complexes result in severe recurrent erosions. The accumulations of fibrous tissue also cause irregular astigmatism and a reticular anterior corneal opacification with diminished vision. The anterior location of this dystrophic process makes it amenable to treatment by superficial keratectomy.7,8 A dissection plane can frequently be developed between the fibrous tissue and the underlying normal stroma. Blunt dissection can then be used to peel the fibrous tissue until it is entirely removed (Color Plate 1: Color Fig. 1A-D). Our experience and that of others7,8 have been very favorable with this technique in achieving cessation of the erosions and improvement of vision. The fibrous tissue may recur after some years, but the procedure can be easily repeated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree