Chapter 84 Spirochetal Infections
Introduction
The history of spirochetal infections in the eye extends back to the first reported observations of spirochetes isolated from the nervous system.1 Today, the most common organisms encountered in the tissues of the eye and ocular adnexae are Treponema pallidum, the infectious entity causing syphilis; Borrelia burgdorferi, the organism responsible for Lyme disease; and Leptospira species, which upon infection produces a host of local and systemic findings typical of leptospirosis. While the majority of these diseases can be treated effectively in the early stages, recognition of the constellation of symptoms often requires a high degree of clinical suspicion.
Syphilitic uveitis
Infection with the spirochete T. pallidum results in the constellation of ocular and systemic findings associated with syphilis. Sexual transmission is the most common means of inoculation, though direct contact with an active lesion or spread via transfusion are also potential routes of infection. Prior to the advent of penicillin, the disease was associated with high morbidity and mortality; however, as the antibiotic became widely available, the incidence of syphilitic disease dropped steeply. In recent years, changing socioeconomic factors and increases in high-risk sexual behavior, infection with human immunodeficiency virus (HIV), and antibiotic resistance have all contributed to resurgence of the disease. Worldwide, there are an estimated 12 million new cases annually, with 90% found in developing nations, and increases in reported cases are seen most commonly in cases of men having sex with men and those who are coinfected with HIV.2,3
While uncommon, ocular manifestations are typically associated with neurosyphilis, which can occur early or late in the course of infection.4 Symptoms can be seen roughly 2–6 months after initial infection.5 The most common ocular finding is uveitis, occurring in 2.5–5% of patients with tertiary syphilis. Clinical signs are protean and can include iritis, chorioretinitis, panuveitis, vitritis, and placoid chorioretinitis.6,7
Epidemiology and pathogenesis
The only known reservoir for syphilis is in the human, and historically, infection had been limited to populations with poor hygiene, limited access to healthcare, and low socioeconomic status. Worldwide, syphilis cases have increased in the past 10 years, up 33.5% between 2000 and 2004 in the USA and 41.5% between 1999 and 2001 in the UK.3,5 The most current surveillance in the USA indicates that the number of reported cases is rising each year, up 39% since 2006 in the USA. Specifically, the rates are rising sharply among young black men between the ages of 15 and 24, with 58.2 cases per 100 000 compared to 19.3 in 2005.3
Local antibodies are also produced against the lipid, protein, and lipoprotein components of T. pallidum. The majority of bacteria are eradicated by opsonization and engulfed by macrophages. Those organisms that are resistant to phagocytosis may persist locally at the site of inoculation. Dissemination can occur despite the development of the humoral and cellular response, and without treatment, the bacteria can persist in the human host for decades, resulting in continued transmission and end-organ damage.8
Ocular manifestations
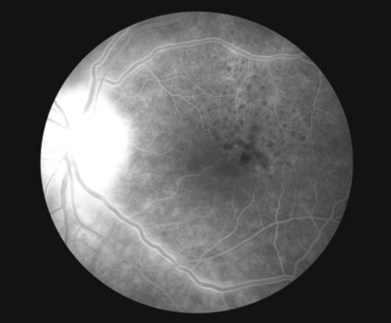
Uveitis is the most common ocular finding, occurring in 2.5–5% of patients with tertiary disease.6 Findings can include keratic precipitates and iritis in the anterior segment of the eye. The iritis and iridocyclitis may manifest as either granulomatous or nongranulomatous inflammation. Dilated iris capillaries may also be noted (roseola), and these dilated and tortuous vessels may be a result of obliterative endarteritis. Chorioretinitis is also common and can present in a variety of ways. Vitritis, vasculitis, papillitis, periphlebitis, exudative retinal detachment, uveal effusion, central retinal vein occlusion, subretinal neovascular membrane formation, retinal necrosis, and neuroretinitis have all been described.9–13 Yellow or gray placoid lesions can often be seen in the macula or juxtapapillary locations. This condition is also termed acute syphilitic posterior placoid chorioretinitis.7,14 The lesions often have atrophic centers and are flat, with no evidence of fluid or hemorrhage. Fluorescein angiography reveals early hypofluorescence and late stain of the lesion with distinctive “leopard spot” hypofluorescence (Fig. 84.1). In patients with HIV, posterior uveitis is more common. A dense vitritis can also be the only presenting sign of syphilitic uveitis in HIV-positive patients.9,15,16 Recently, a more defined presentation of diffuse, creamy retinitis with overlying punctuate retinal precipitates has been described in HIV-positive patients diagnosed with syphilitic uveitis.17–19
Diagnosis
A high level of clinical suspicion is required for the appropriate diagnosis of syphilitic uveitis, due to its variable clinical presentation. In HIV-infected individuals, the presentation of syphilitic uveitis may be atypical; thus a strong clinical suspicion is especially important in evaluating those patients. Appropriate laboratory studies can aid in confirming the diagnosis and rule out other disease entities. Visualization of the organism in lesion exudates or tissue via dark-field microscopy with immunofluorescent staining is considered the gold standard and the quickest and most direct approach for establishing the diagnosis; however, the availability of such facilities limits its utility in clinical practice.20 In addition, these tests are highly specific, but not very sensitive for widespread detection of infection.
The use of a singular type of serologic test is insufficient for diagnosis, as each has its limitations, specifically the false-positive test results in patients without syphilis. False-positive test results may be associated with certain infections (e.g., Lyme disease, leptospirosis, malaria) and medical conditions (e.g., autoimmune disorders, intravenous drug use, pregnancy). A good rule of thumb in the evaluation of the patient with suspected syphilitic infection is to obtain a nontreponemal test and, if the initial study is reactive, confirm the diagnosis with a treponemal test. For those individuals with a positive treponemal screening test, a standard nontreponemal test with titer should be ordered to guide therapeutic decisions. If the nontreponemal test is negative, a different treponemal study should be ordered to confirm the results of the initial test. If the second treponemal test is positive, treatment should be initiated; alternatively, those patients with a history of prior therapy should be followed by observation unless a review of their sexual history indicates a likelihood of re-exposure.21,22
Newer testing, which may not always be available to the clinician, includes polymerase chain reaction (PCR) assays and rapid specific treponemal tests. PCR assays, if available, should be conducted on frozen specimens (shipped according to the laboratory specifications), but cannot discern between live or dead organisms. The rapid tests, which may use as little as 10–50 µL of sample, are considered to be equivalent to the older specific treponemal antibody tests, and have similar limitations in terms of distinguishing active versus inactive infection.23,24
For HIV-infected individuals, these serologic tests are often accurate and reliable for diagnosis as well as following the response to therapy. Atypical results (i.e., unusually high/low/fluctuating titers) without corresponding clinical findings suggestive of early syphilis should prompt the clinician to investigate further and consider other tests to confirm the diagnosis.21 False-negative tests may occur due to insufficient production of antibody to the bacterial proteins, or an overall lack of immunoreactivity.
Consideration of further testing is warranted in all patients with neurosyphilis, as no single test can be used to diagnose this presentation in all instances. Cerebrospinal fluid (CSF) analysis, along with VDRL and FTA-ABS tests, may need to be considered in confirming the diagnosis of neurosyphilis.4 CSF FTA-ABS is often too sensitive and thus the role of this test is still controversial. CSF VDRL does have the advantage over CSF FTA-ABS in cases requiring differentiation of current active infection from past infection. Leukocytosis and elevated protein concentrations can be seen in the CSF and these findings are often present for more than 1 year in those individuals with neurologic symptoms. This is consistent with neurosyphilis and warrants treatment even if test results are negative.
Differential diagnoses
The clinical findings and possible differential diagnoses for syphilitic uveitis are listed in Table 84.1. The most critical diagnosis to make may be acute syphilitic posterior chorioretinitis, and one must rule out acute posterior multifocal placoid pigment epitheliopathy and atypical serpiginous choroidopathy. In these instances, the use of intravitreal steroid or systemic immunosuppressive therapy for treatment of these conditions may unmask an underlying infection.14 It is important to emphasize that a high degree of clinical suspicion is vital in order to make the diagnosis, and that serologic confirmation is required.
Table 84.1 Differential diagnosis of ocular syphilis with laboratory workup
| Disease/disorder | Possible serologic/laboratory testing |
|---|---|
| Toxoplasmosis | IgM-ELISA, IgG-ELISA for antibodies to Treponema gondii |
| Rubella | IgM-ELISA, IgG-ELISA for rubella; rubella titer |
| Cytomegalovirus (CMV) | CMV DNA PCR |
| Human immunodeficiency virus (HIV) | ELISA |
| Herpes simplex virus (HSV) | Diagnostic viral culture, HSV-1/HSV-2 serologic assays |
| Varicella-zoster virus (VZV) | Diagnostic viral culture, antibody assays |
| HLA-B27-related uveitis | HLA-B27 genetic testing |
| Primary intraocular lymphoma | Cytology on vitreous or aqueous humor; neuroradiologic and CSF studies |
| Sarcoidosis | Angiotensin-converting enzyme (ACE) level |
| Tuberculosis | PPD, QuantiFERON gold testing |
| Idiopathic uveitis | Diagnosis of exclusion after testing for other uveitic entities |
IgM/IgG, immunoglobulin M/G; ELISA, enzyme-linked immunoabsorbent assay; PCR, polymerase chain reaction; HLA, human leukocyte antigen; CSF, cerebrospinal fluid; PPD, purified protein derivative.
Treatment
The clinician who diagnoses syphilitic infection in a patient has two responsibilities: to report the case to the state Department of Health;25 and to determine if he or she is comfortable in managing and following the therapeutic regimen for the patient. A survey of infectious disease practitioners conducted in 2008 found variation in the management of syphilis among the experts, particularly in cases where patients were coinfected with HIV.20 It is the recommendation of the authors that the ophthalmologist treat the patient in consultation with an infectious disease specialist.
Penicillin G is the preferred treatment for all stages of syphilis (Table 84.2). The dose, route of administration, and duration of therapy are determined by the stage and clinical findings. Sexual partners of the infected individual also need to be evaluated and treated.21 For patients with a penicillin allergy, alternative antibiotics may be used; however, as the other medications are not as effective as penicillin, skin testing and desensitization are recommended, especially in those patients who are coinfected with HIV. As for patients diagnosed with congenital syphilis, treatment with aqueous penicillin G or procaine penicillin G via intravenous administration is recommended. Other antibiotics such as ceftriaxone and ampicillin have been used, but there is no optimal therapy for congenital syphilis noted at this time.
Table 84.2 Recommended treatment of syphilis
| Stage of disease | Preferred treatment | Alternative treatment |
|---|---|---|
| Primary, secondary, or early latent | Benzathine penicillin G 2.4 million units IM, single dose | Doxycycline 100 mg po BID ×2 weeks or tetracycline 500 mg po QID ×2 weeks |
| Late latent, latent syphilis of unknown duration, tertiary stage, or those who fail primary therapy | Benzathine penicillin G 2.4 million units IM, administered weekly ×3 weeks | Doxycycline 100 mg po BID ×4 weeks or tetracycline 500 mg po QID ×4 weeks |
| Neurosyphilis | Aqueous penicillin G 3–4 million units IV every 4 hours ×10–14 days | Procaine penicillin 2.4 million units IM daily ×10–14 days and probenecid 500 mg po QID ×10–14 days |
Notes: (1) Human immunodeficiency virus-positive patients should be treated with penicillin at all stages of infection, and those allergic to penicillin should be desensitized and then treated with the full regimen. (2) All patients with tertiary syphilis should have a cerebrospinal fluid analysis and be evaluated for neurosyphilis.
(Adapted from Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR 2010;59:26–40.)
Syphilitic uveitis or other ocular manifestations associated with neurosyphilis should be treated according to the recommendations for neurosyphilis.4 A CSF examination is recommended for all patients with syphilitic eye disease to guide therapy. The recommended regimen is aqueous crystalline penicillin G delivered intravenously, as no alternative has been proven scientifically effective. In those patients who have failed primary therapy and show evidence of tertiary syphilis, asymptomatic neurosyphilis may be present and may warrant evaluation of the CSF.21 With regard to neurosyphilis in the HIV-positive patient, treatment with intravenous penicillin utilizing the neurosyphilis recommendations results in rapid resolution of findings.19 It is important to note that therapy must be of a duration and dose sufficient to cure neurosyphilis, regardless of CSF findings.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree