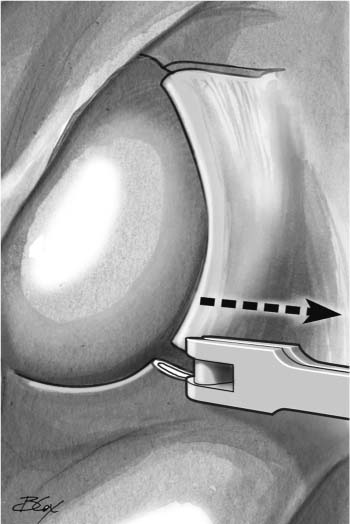
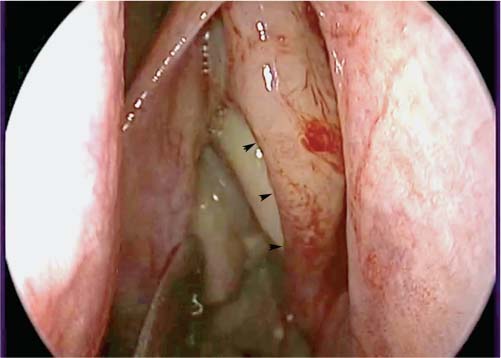
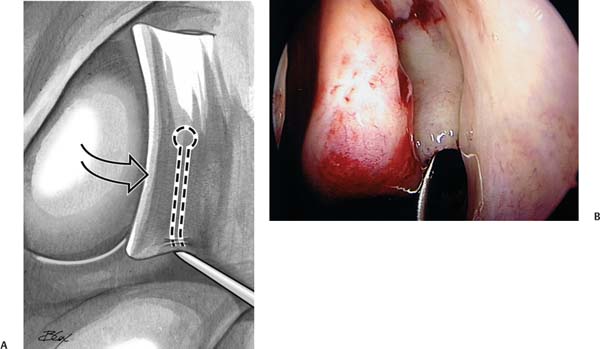
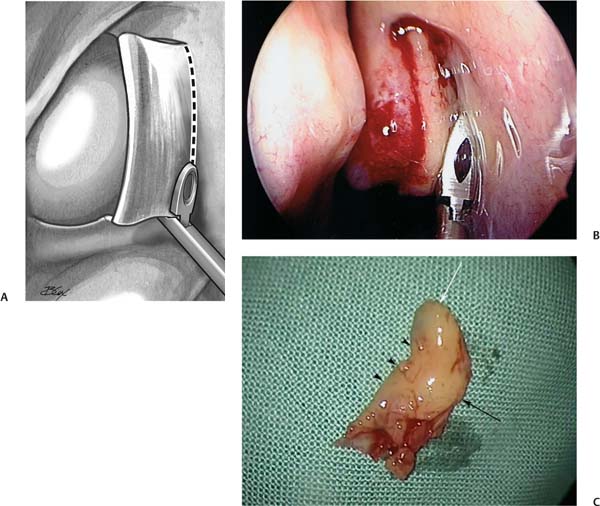
12 Revision Maxillary Sinus Surgery including Canine Fossa Trephination One of the keys to achieving successful outcomes from functional endoscopic sinus surgery (FESS) is controlling disease within the maxillary sinus. Depending on the disease process present, different approaches are required to achieve this. However, what is essential is to provide adequate ventilation and optimize the natural drainage pathway for the maxillary sinus. Additionally, it is important to reduce the disease load within the maxillary sinus to optimize the chance of the sinus mucosa returning to a healthy state. Even if initial management of the maxillary sinus is optimal, there are several potential reasons for persistent disease within the sinus requiring further surgical intervention. Revision surgery may play a role in the continuum of management of the patient’s disease condition; however, different care may be required at different time points and the underlying factors contributing to sinus disease must be sought and addressed. In this chapter, we provide an overview of the indications and the options for surgical treatment in the management of previously operated maxillary sinus, including the canine fossa trephination techniques. The potential causes for failed surgery are numerous. Several series have looked at the causes of postsurgical persistent or recurrent disease, and provide information regarding the frequency of various anatomic findings, many of which pertain to the maxillary sinus. Chu et al1 evaluated 153 patients requiring revision endoscopic sinus surgery, and found the most common surgical alteration associated with recurrent sinus disease was middle meatal scarring and lateralization of the middle turbinate. This was usually the result of partial middle turbinectomy during the initial surgery. Lateralization of the middle turbinate was also reported by Musy and Kountakis2 as the most common postsurgical finding associated with primary surgery failure. Other findings included incomplete anterior ethmoidectomy (64%), scarred frontal recess (50%), retained agger nasi cell (49%), incomplete posterior ethmoidectomy (41%), retained uncinate process (37%), middle meatal antrostomy stenosis (39%), and recurrent polyposis (37%). Ramadan3 reviewed 52 cases and found that the most common cause of failure was residual air cells and adhesions in the ethmoid area (31%), followed by maxillary sinus ostial stenosis (27%), frontal sinus ostial stenosis (25%), and a separate maxillary sinus ostium stenosis (15%). Focusing more specifically on the maxillary sinus, Richtsmeier4 reviewed 85 patients presenting with persistent maxillary sinus symptoms after endoscopic sinus surgery and identified 10 categories of reasons for failure. These included obstructed natural ostia, disease in the anterior ethmoid or frontal sinus, resistant organisms, intrasinus foreign body, incurable mucosal disease, noncompliant patient, wrong primary diagnosis, maxillary osteitis, mucus maltransport, and immunodeficiency. Cohen and Kennedy5 simplified this by clustering the above into six large categories of local problems: recirculation, infection draining into the maxillary sinus from elsewhere, retained foreign material (including infected dental work), failure of mucociliary transport, scar separation of the sinus from the nasal cavity, and local osteitis. The recirculation phenomenon may be caused by a retained or partially resected uncinate process with an iatrogenic posterior fontanelle antrostomy. Less frequently, it can be caused by scarring at the anterior aspect of the antrostomy. The “missed ostium sequence,” as described by Parsons et al,6 occurs when there is incomplete removal of the most anterior portion of the uncinate process, obscuring the position of the natural maxillary sinus ostium. This prevents the middle meatal antrostomy from communicating with the natural ostium, resulting in a recirculation phenomenon (Fig. 12.1). In this instance, mucociliary flow causes mucous to reenter the sinus causing a functional obstruction of the maxillary sinus and continued sinus disease (Fig. 12.2). The treatment at surgery is to resect the intervening tissue; this removes the bridge generating the recirculation. A 70-degree scope is ideally suited to examine these regions and to ensure that there is no residual uncinate or scarring present. A common cause of persistent disease in the maxillary sinus is mucous and/or mucopus draining into it. Infected secretions may also originate either from disease in the frontal sinus, frontal recess, and/or the anterior ethmoid cells, and these areas can usually be identified easily on a computed tomography (CT) scan (Figs. 12.3A,B). It is essential to localize accurately the origin of the infected material and to target treatment toward these areas; in most cases, this will lead to resolution of the maxillary disease. Even after managing this frontal or ethmoidal disease, however, there may be a requirement to control and eradicate disease within the maxillary sinus that may have arisen because of the persistent infected load seeping into the maxillary sinus. Fig. 12.1 The“missed ostium sequence”: after the uncinectomy has been performed, 2 to 3 mm of residual uncinate remains(solid black arrow), obscuring the natural maxillary sinus ostium(broken black arrow). This may not be recognized by the surgeon, and can result in a posterior fontanelle ostium being created. This can subsequently result in a mucus recirculation phenomenon. The position of the original edge of the uncinate process is illustrated by the dotted line. Fig. 12.2 Intraoperative picture of mucus recirculation; a sickle knife is used to demonstrate a stream of mucus originating from the natural maxillary sinus ostium, and partly flowing back into the sinus through an accessory ostium in the posterior fontanelle. Fig. 12.3 (A) Coronal computed tomography (CT) scan of the sinuses, bone window, demonstrating diseased residual right ethmoids cells with significant osteitis and new bone formation (arrowheads), representing a source for mucus draining into the diseased right maxillary sinus ostium.(B) Parasagittal CT scan of the sinuses, bone window, in the same patient showing disease in a retained agger nasi cell (asterisk) and frontal sinus. Fig. 12.4 (A) Coronal computed tomography (CT) scan of the sinuses, soft tissue window, demonstrating diffuse fungal rhinosinusitis, with complete opacification of bilateral maxillary sinuses and typical double-densities.(B) Coronal CT scan of the sinuses, soft tissue window, showing partial opacification of the left maxillary sinus, and a metal density representing dislodged dental amalgam. Careful attention should be given to the possibility of retained foreign bodies on the sinus floor, including inspissated concretions, dental filling material, or bone chips. These may be manifested on preoperative CT imaging by partial to complete opacification, double densities (Fig. 12.4A), calcifications, or metal artifact (Fig. 12.4B). However, the diagnosis can only be confirmed by endoscopic examination using angled scopes during surgery. This is achieved by first performing an uncinectomy and middle meatal antrostomy, followed by inspection with a 70-degree endoscope. Polyps and thick tenacious mucous in the floor and anterior regions of the sinus require removal. In patients with severe and aggressive disease, such as allergic fungal rhinosinusitis, as well as the nonallergic eosinophilic rhinosinusitis variants, leaving eosinophilic mucin within the sinus may contribute to a rapid recurrence of disease.7 This may be due to ongoing exposure to fungus within the mucin, or toxic substances such as major basic protein released by the eosinophils. Figure 12.5 demonstrates ointment left within the maxillary sinus during prior surgery. It must be emphasized that no ointment should ever be left within the sinonasal cavity, as the petroleum component within the ointment cannot be absorbed or cleared by the body and remains as a foreign body. Occasionally, a unique reaction known as myospherulosis occurs, which was so named due to its histopathologic pattern once mistakenly thought to represent endosporulating fungus. Patients who develop myospherulosis appear more likely to form postoperative adhesions, which may hasten the need for revision surgery.8 Instances when maxillary disease is inaccessible through a wide middle meatal antrostomy may require a sublabial approach via canine fossa trephination. This permits the inspection and debridement of the entirety of the sinus cavity. If inspissated material, such as eosinophilic mucin is evident on the floor of the sinus, the offending material can either be lifted up using the tip of the trocar as a spoon to where it can be accessed by a curved suction through the middle meatal antrostomy, or simply removed using the microdebrider. In a study of patients with severely diseased maxillary sinuses, those who underwent canine fossa trephination and clearance of the sinuses had significantly improved long-term outcomes with regard to disease recurrence and symptom scores as compared with patients who did not have the procedure performed.7 Failure of mucociliary transport often results from systemic disease, such as cystic fibrosis or Kartagener syndrome. These entities are identified by careful history, laboratory studies, and light as well as electron microscopy. In these situations, a “megaostium” (i.e., one that encompasses most of the medial wall of the maxillary sinus) should be created to allow for copious nasal irrigation with concomitant appropriate head positioning and gravity drainage. Fig. 12.5 Endoscopic view of antibiotic ointment left within the maxillary sinus during a previous surgery. Complications of prior endoscopic sinus surgery include the formation of synechiae causing obstruction of the nasal passage or sinus outflow tract, osteitis with significant bony hypertrophy, or even mucocele formation. A condition predisposing to scar formation and ostial stenosis is the creation of circumferential mucosal trauma during surgery, particularly if the antrostomy produced is not large. The maxillary sinus is infrequently the site of mucocele formation, accounting for less than 10% of all paranasal sinus mucoceles.9,10 However, the most common situation leading to the development of mucoceles in this area is following Caldwell–Luc procedures, where the mucosa has been stripped. This process can be suspected on CT when there is smooth, round enlargement of a completely opacified sinus with associated bony remodeling and thinning (Fig. 12.6). Both the employment of through-cutting instruments and the judicious use of a powered microdebrider are helpful in preventing excessive mucosal stripping during FESS. This, in turn, minimizes the exposure of bone, which leads to osteitis, persistent inflammation, and perhaps further scarring and bony hypertrophy. Unopened infraorbital ethmoid (Haller) cells can directly obstruct maxillary sinus outflow (Fig. 12.7). Alternatively, even when opened, a diseased residual Haller cell may have osteitic partitions creating persistent localized mucosal hypertrophy. These partitions can be a focus for residual inflammation, if not totally resected.11 A biofilm is a multicellular community of bacteria that is embedded in a self-produced exopolysaccharide matrix and irreversibly attached to a surface. The existence of biofilms on the sinus mucosa of patients with chronic rhinosinusitis (CRS) is well described, and there is increasing evidence that biofilms affect the postoperative evolution of these patients. In an initial study, Bendouah et al12 cultured 31 bacterial strains from post-ESS patients, of which 22 were significant biofilm producers. They found a correlation between the in vitro biofilm-producing capacity of Pseudomonas aeruginosa and Staphylococcus aureus and unfavorable evolution after ESS, as determined by questionnaire and endoscopy. In a retrospective analysis of 40 sinus surgical patients conducted in our department, bacterial biofilms were detected in 50% of these.13 This subset of patients had significantly worse preoperative radiologic scores, as well as statistically worse postoperative symptoms and mucosal outcomes. The only other factor that was statistically related to an unfavorable outcome was the presence of fungus at the time of surgery. In this study the presence of polyps, eosinophilic mucin, or pus was not related to poor outcome. This provides evidence that biofilms indeed may play an active role in perpetuating inflammation in CRS patients, and may explain the recurrent and resistant nature of this disease. Fig. 12.6 Coronal computed tomography(CT) scan of the sinuses, bone window, demonstrating a right maxillary sinus mucocele arising after previous Caldwell–Luc procedure; note the smooth, rounded enlargement of the completely opacified right maxillary sinus, with associated thinning of the lateral(arrowheads) and medial walls (white arrow) of the sinus. Fig. 12.7 Coronal computed tomography(CT) scan of the sinuses, demonstrating an infraorbital ethmoid cell(arrowheads), or Haller cell, contributing to outflow obstruction of the left maxillary sinus, which is partially opacified. Given that biofilms present on sinus mucosa are difficult to eradicate with conventional antibiotic therapy, our department has investigated the usefulness of topical antibiotics via nasal irrigation. This was done with the aim of delivering high concentrations of antibiofilm agents with potentially low systemic absorption and side effects. Mupirocin was capable of reducing biofilm mass in vitro by greater than 90% at concentrations of 125 μg/mL or less, in all S. aureus isolates investigated.14 Ciprofloxacin and vancomycin were largely ineffective within safe dosage ranges. To examine the efficacy and tolerability of topical mupirocin in the clinical setting, a prospective open-label pilot study was performed.15 Sixteen patients with surgically recalcitrant CRS, who had positive nasendoscopically guided cultures for S. aureus, were treated with a 3-week course of 0.05% mupirocin in lactated ringers nasal lavages given twice daily. Fifteen of the 16 patients had improved nasendoscopic findings after treatment; 12 patients noted overall symptom improvement based on the sinonasal outcome test (SNOT-20) and visual analogue scale (VAS) questionnaires; and 15 patients had negative swab results for S. aureus after treatment. Only minimal adverse effects were experienced. Thus, the topical application of mupirocin via nasal irrigation may be useful in eliminating S. aureus biofilms present on the sinus mucosa of patients with CRS, and may offer an additional treatment to patients with recalcitrant sinusitis. Cigarette smoking has been associated with statistically worse outcomes after ESS based on disease-specific quality of life measures.16 Exposure to cigarette smoke adversely affects mucosal ciliary function,17 as well as sinus cilia regeneration following functional endoscopic sinus surgery.18 A history of smoking should be elicited for all patients presenting with postoperative sinonasal complaints and smoking cessation encouraged, with an emphasis on the detrimental effects of cigarette smoke on nasal and sinus health. In patients with post-ESS symptoms where no origin for their symptoms can be identified, other causes of sinonasal symptoms should be considered. In the case of facial pain, neuralgia, migraine-equivalent (midfacial headache), or dental problems may be responsible. Axial CT should be used to carefully assess the possibility of a small periapical abscess producing pain. In individuals with a history of migraine or multiple surgeries, a trial of amitriptyline may be warranted. The clinician should attempt to elicit the patient’s symptoms and classify them according to severity. The total severity can be classified by having patients answer the following question using a VAS graded on a 10-cm scale, “How troublesome are your symptoms of rhinosinusitis?” A VAS score of ≤3 corresponds to mild, >3 to 7 corresponds to moderate, and >7 corresponds to severe.19 The goal of the medical work-up is to identify mucosal, systemic, and environmental factors responsible for poor outcome. A history of underlying immune deficiency, connective tissue disorder, cigarette smoking, malignancies, or genetic disorder such as cystic fibrosis or primary ciliary dyskinesia should be sought. A complete immune work-up, and possibly a vaccine response, should be ordered to rule out immune deficiency if suspected. Blood work is also helpful to rule out other systemic disorders such as Wegener granulomatosis and sarcoidosis. Defects in functional immune response not evident in static testing have been identified in certain patients who have refractory CRS. In the absence of response to all other therapies, a 6-month trial of intravenous high-dose immunoglobulin (IVIG) may be warranted.20 Sinonasal endoscopy, preferably rigid, is essential in evaluating persistent disease. It may help identify structural anomalies, masses, or secretions not seen on anterior rhinoscopy. The presence of a posterior fontanelle ostium and circular flow of mucus should be sought. This can often be seen with a 30-degree endoscope. The bacteriology of CRS may vary in an individual patient over time. Obtaining endoscopically guided cultures from the middle meatus or the sphenoethmoid recess (not the nasal cavity) will help in the selection of antibiotic therapy, particularly in cases unresponsive to empiric therapy. Care must be taken to avoid contact with the nasal wall or vestibule to minimize contamination, and to sample directly within purulent secretions when present, rather than adjacent areas. CT of the sinuses is essential for completing the assessment of the patient with persistent post-ESS complaints. Preferably, the patient should undergo a high-definition helical multislice CT scan of the sinuses, with cuts measuring 0.5 to 1 mm in the axial plane, and reconstructed in the coronal and parasagittal planes. CT may be used to assess disease load or to identify technical factors that may not be revealed on endoscopy such as the presence of a natural or accessory ostium, residual ethmoid cells, Haller cells, persistent frontal recess and frontal sinus disease, obstructions to sinus drainage, or mucocele formation. Disease load can be determined from identifying the number of sinuses involved with disease and the extent of their involvement. The Lund–Mackay staging system is an effective method of standardizing reporting of radiologic severity of disease.21,22 In patients selected to undergo revision maxillary sinus surgery, particular attention must be paid to the preoperative CT scan specifically to determine the level of integrity of the lamina papyracea. Areas of dehiscence—which may be due to the previous surgery, exuberant disease, or underlying patient anatomic variations—can be present and can be of significant size (Fig. 12.8) (see Video 12.1). For this reason, it is prudent practice always to verify the integrity of the lamina papyracea prior to clearing disease from this area. This is done by applying gentle pressure to the globe of the eye, while inspecting for transmitted movement of the lamina under endoscopic visualization. Cases of dehiscence of the lamina papyracea after previous endoscopic sinus surgery are often the result of forcing instruments, such as a curved suction, into the area of the natural maxillary sinus ostium under poor visualization, in the setting of severe mucosal disease and edema. The most common area for dehiscence in the lamina papyracea is just posterior to the frontal process of the maxilla, where the bone is thinnest. Recognition of this situation is of utmost importance for patients who will undergo a canine fossa puncture or trephination, as the use of the microdebrider to clear disease overlying the dehiscence could result in orbital penetration with disastrous consequences. In this instance, polyps should be carefully cleared using cold steel instruments, such as through-biting Blakesley forceps. Fig. 12.8 Coronal computed tomography(CT) scan of the sinuses, bone window, demonstrating a sizable bony defect (arrowheads) in the lamina papyracea of the left orbit. Finally, it must be emphasized that in the presence of unilateral disease, bony expansion, or destruction, or exuberant local disease out of proportion to the rest of the sinus cavities, it is essential to exclude the possible diagnosis of neoplasm (either benign or malignant). Magnetic resonance imaging (MRI) scans should be obtained in patients suspected of having a nasal mass, to better delineate the tumor size and differentiate it from pooled sinus secretions. It is uncommon for image guidance to play a role in revision surgery to the maxillary sinus. There may be a place in situations where disease is extending beyond the confines of the maxillary sinus (i.e., into the infratemporal fossa or orbit). A detailed discussion of the medical management of refractory maxillary sinus disease is beyond the scope of this chapter, and is covered elsewhere in this book. However, it must be stressed that an adequate trial of maximal medical therapy should be given preoperatively and documented in the chart. Systemic steroids may be beneficial in the preoperative period to reduce the size and vascularity of polyps in patients with significant nasal polyposis. A preliminary study recently published found that 30 mg of prednisone administered daily for 5 days preoperatively resulted in a significantly improved surgical field grading score during endoscopic sinus surgery.23 Empiric treatment regimes range from 30 to 50 mg of prednisone daily for between 5 and 7 days preoperatively. However, further studies are necessary to clarify the optimal dose of steroids, length of treatment, and groups of patients that would benefit from this treatment. The role of revision surgery is principally to improve medical management and surgery should be planned and executed to optimize this. This is achieved by reducing disease load, by removing recurrent nasal polyps or hypertrophic sinonasal mucosa, and/or by improving access for continuing medical care in the form of topical solutions. Wide antrostomies are necessary in certain patients for problem sinuses to provide better access for irrigating solutions. The patient can never truly be deemed a failure of therapy until all obstructions to drainage and ventilation (or irrigation) have been corrected. Continued postoperative medical therapy is essential and can be considered an integral part of surgery. The decision to reoperate a patient with maxillary sinus disease is centered principally on the demonstration of a symptomatic obstruction to sinus drainage or the presence of significant disease load in the sinuses. This must be tempered by the clinician’s judgment, experience, and comfort level. Given the nature of endoscopic sinus surgery and the close proximity of numerous critical structures, special care must be taken to avoid serious intraoperative complications from damage to adjacent structures.24–26 Preoperative sinus imaging and a precise understanding of the patient’s anatomy are thus of paramount importance. Indications for revision sinus surgery can be grossly divided into four main categories: A. Incomplete previous surgery • Persistence of symptoms and signs of CRS with or without nasal polyposis or recurrent acute sinusitis with retained uncinate process or persistent ethmoid cells on CT • Unrepaired septal deviation, persistent concha bullosa, or Haller cell impairing maxillary sinus drainage (see Videos 12.2, 12.3, and 12.4 for demonstrations of the surgical approach to each of these problems) • Missed ostium sequence with recirculation of mucus (see Video 12.5 demonstrating the uncinectomy and middle meatal antrostomy in the presence of an accessory mallary ostium) B. Complications of previous surgery • Synechia formation causing obstruction of nasal passage or sinus outflow • Lateralization of the middle turbinate with or without adhesions between the middle turbinate and lateral nasal wall • Significantly denuded bone, with subsequent osteitis and bony hypertrophy impairing sinus outflow • Suspected mucocele formation C. Recurrent sinus disease • Recurrent nasal polyps refractory to maximal medical management • Persistent isolated sinusitis that is symptomatic • Recurrent allergic fungal rhinosinusitis • Concurrent nasal polyposis and an intolerance or contraindication to oral cortisone D. Histologic evidence of neoplasia • Unexpected diagnosis of neoplasia on pathologic analysis with subtotal resection • Localized severe disease suspicious for neoplasia such as inverted papilloma Prior to performing revision uncinectomy or maxillary antrostomies, it is essential to manage any adhesions in the region. Any simple adhesions between the middle turbinate and lateral nasal wall can be divided with through-cutting instruments. A decision must be made as to the position of the middle turbinate. If the middle turbinate is in a lateralized position, then it may be important to fix it in a more midline position. Our preferred method is to suture the middle turbinate to the septum with a 4–0 Vicryl (Ethicon, Somerville, NJ) suture running from one middle turbinate, through the septum, then the contralateral middle turbinate. The stitch is then run forward and tied just inside the nasal vestibule. The swing-door technique of uncinectomy was created with the aim of achieving a complete removal of the mid-portion of the uncinate process and exposing the natural ostium of the maxillary sinus. This technique is ideally performed during the initial surgical attempt. However, if there is an indication for revision maxillary sinus surgery and a retained uncinate process is one of the contributing reasons, then elements of this technique can be applied as needed. A sickle knife is used to cut the uncinate horizontally just under the axilla of the middle turbinate (Figs. 12.9, 12.10). The tip of the sickle knife should go through all three layers (mucosa–bone–mucosa) and will then be felt to strike the hard bone of the frontal process of the maxilla. Risk of penetration of the orbit is extremely small as the uncinate attaches to the frontal process on the maxilla in this region and not onto the lacrimal bone as it does above the inferior turbinate insertion. Next, the pediatric backbiter is introduced into the middle meatus and the free edge of the uncinate mobilized with the tooth of the backbiter (Fig. 12.11). This allows the tooth to be slid into the hiatus semilunaris and the uncinate engaged. Usually, three bites of the backbiter are necessary before the frontal process is reached, but this may vary from patient to patient and be considerably less in patients with a retrocurved uncinate (Fig. 12.12) or who have had previous surgery. With the third bite, the backbiter is rotated from horizontal until it is angled at 45 degrees so that the tooth when closed should pass medial to the nasolacrimal duct. The risk of injury to the nasolacrimal duct is reduced with this maneuver. The right-angled ball probe is placed through the inferior cut behind the uncinate process and the midportion of the uncinate process is fractured anteriorly (Fig. 12.13). Next, an upturned 45-degree through-biting Blakesley forceps is used to cut the uncinate flush with the lateral nasal wall (Figs. 12.14A,B). The mid-portion of the uncinate can now be removed in one piece (Fig. 12.14C). Fig. 12.9 In this diagram, the sickle knife makes the upper cut directly under the axilla of the middle turbinate. A pediatric backbiter is introduced at the vertical and horizontal portions of the uncinate process and the lower cut is made. EB, ethmoid bulla; UP, uncinate process; MT, middle turbinate. Figs. 12.10 Intraoperative photo of the sickle knife making the upper horizontal cut in the uncinate process directly under the axilla of the left middle turbinate. Fig. 12.11 Illustration of the pediatric backbiter making the lower horizontal cut at the transition between the middle portion and the horizontal portion of the uncinate process. It is important to note that we discourage the use of the microdebrider for removal of the midportion of the uncinate. To remove the uncinate flush with the frontal process of the maxilla, the microdebrider blade needs to be pushed firmly against the orbital wall. This significantly increases the risk of orbital penetration and damage to the medial rectus muscle. If the microdebrider blade is used only very gently against the frontal process, inevitably, a variable amount of uncinate will remain and this will make identification of the natural ostium more difficult. In addition, even gentle use of the microdebrider blade on this portion of the lamina papyracea may be sufficient to penetrate the orbit. The thinnest and therefore the most dangerous region of the lamina papyracea is the region directly behind the frontal process of the maxilla and may, in fact, be dehiscent in some patients. We therefore recommend that microdebriders should be avoided in this area. Removal of the midportion of the uncinate is easily and cleanly achieved with cold steel instruments without significant risk to the orbit and is therefore the recommended technique. Removal or trimming of the horizontal section of the uncinate is often performed with the microdebrider as the direction of the blade in inferior and away for the lamina papyracea therefore not putting this area at risk. This is described below. Fig. 12.12 Endoscopic view inside the left middle meatus demonstrating a retrocurved uncinate process; the free edge is indicated (arrowheads). Before any attempt is made to visualize the natural ostium, the zero-degree endoscope should be changed to the 30-degree endoscope. This allows better visualization of the middle meatus and greater precision in the dissection. The natural ostium is found by placing the tip of the ball probe directly over the cut edge of the horizontal portion of the uncinate. If possible, any residual horizontal portion of uncinate bone should be dissected free from between its two mucosal layers. The double right-angled ball probe is used to elevate the mucosa off the medial side of the uncinate (Fig. 12.15). The bone is then fractured medially and the mucosa on the lateral side is elevated. The bone can then be removed using a straight Blakesley forceps (Fig. 12.15), leaving only the mucosal layers, which are then delicately trimmed with the microdebrider. This allows the edges of the mucosa to be closely applied resulting in first intention healing. Failure to remove the bone from the horizontal portion of the uncinate can leave exposed bone between the mucosal layers resulting in granulation and scar tissue formation. Once the mucosal edges of the horizontal uncinate are trimmed, this will expose the natural ostium of the maxillary sinus with no trauma to the superior and posterior regions of the natural ostium. Fig. 12.13 (A) Illustration of the ball probe placement behind mid-portion of the uncinate process, which is then fractured forward flush with the lateral nasal wall. (B) Intraoperative photo of a ball probe fracturing the midportion of the uncinate process forward flush with the lateral nasal wall. Fig. 12.14 (A) The 45-degree through-biting Blakesley is used to cut the uncinate process flush with the lateral nasal wall. (B) Intraoperative photo of the 45-degree through-biting Blakesley cutting the uncinate process flush with the lateral nasal wall. (C) The removed middle portion of the uncinate process, with the superior portion (white arrow), anterior cut edge (black arrow), and posterior free edge (arrowheads) indicated. It may be necessary to enlarge the meatal antrostomy to examine the sinus with an angled scope accurately, and to instrument the sinus in case of diseased material requiring removal. This is done by removing the posterior fontanelle using a straight through-biting Blakesley forceps or micro-debrider. An antrostomy diameter of ~10 × 10 mm is usually sufficient to perform these tasks. Furthermore, in cases of accessory or iatrogenic sinus ostia located in the area of the posterior fontanelle (Fig. 12.16), or in the missed ostium sequence as described above, it is necessary to join surgically the posterior ostium to the natural maxillary sinus ostium. This is done to prevent the recirculation phenomenon, which may account for recurrent sinusitis symptoms after ESS. This can be done by inserting a backbiter into the accessory ostium and coming forward to the natural ostium (see Video 12.5); any excessive tissue edges can be carefully microdebrided thereafter. It is currently unclear whether creating a wide meatal antrostomy is detrimental to the long-term health of the maxillary sinus. A study in our department showed that there was a significant decrease in nitric oxide (NO) concentration in the maxillary sinuses and nasal cavities of patients with large maxillary sinus ostia (greater than 5 × 5 mm).27 NO is produced by nitric oxide synthase (NOS) type II in the mucosa of the sinuses,28,29 and its production is induced by bacterial inflammation.30 It is known to stimulate ciliary motility, and is believed to play an important role in the innate immune defenses of the nasal mucosa to bacteria, viruses, and fungi.31 However, it is not known whether a lower concentration of NO in the nasal cavity and sinuses actually predisposes to recurrent infections; this association still needs to be studied. Fig. 12.15 (A) Diagram illustrating the double right-angle ball probe dissecting the bone of the horizontal portion of the uncinate process.(B) Intraoperative photo of the ball probe dissecting the bone away from the mucosa of the horizontal portion of the uncinate process. (C) Bone of the horizontal portion of the uncinate process removed from between the two layers of mucosa. Fig. 12.16 Endoscopic view of the right natural maxillary ostium anteriorly(arrowheads), as well as an accessory ostium in the posterior fontanelle (black arrow), using a 30-degree endoscope. Another consequence of removal of the posterior fontanelle during enlargement of the maxillary meatal antrostomy may be the drainage of secretions from the frontal and anterior ethmoid sinuses into the maxillary sinus. The natural drainage pathway of the former two sinuses begins above the natural maxillary sinus ostium, and runs along the base of the ethmoid bulla, then across the posterior fontanelle and under the eustachian tube to the nasopharynx. For the aforementioned reasons, enlargement of the maxillary sinus ostium into the posterior fontanelle is not performed in all patients, but rather is reserved for those with more severe disease. This includes extensive polyp formation within the maxillary sinus, or large amounts of thick and viscid secretion, such as fungal mucous. Additionally, patients with Samter’s triad and cystic fibrosis should have a wide meatal antrostomy to allow copious sinus irrigation and delivery of topical therapy. Following the uncinectomy, it is useful to grade the extent of disease affecting the maxillary sinus at the time of surgery. This will aid in the intraoperative decision-making process. A 70-degree endoscope is used to visualize the maxillary sinus contents through the natural ostium, and the level of disease is graded according to Table 12.1. Grade 1 (Fig. 12.17A) and grade 2 (Fig. 12.17B) are reversible with adequate clearance of mucus and aeration of the maxillary sinus, but grade 3 disease is irreversible (Fig. 12.17C). Therefore, the polyps, and especially the thick eosinophilic mucus should be cleared before reepithelialization and reciliation occur. Extensive maxillary sinus disease can be a difficult problem to tackle endoscopically, especially in the anterior and inferior regions of the antrum. Access by way of the natural ostium of the maxillary sinus will only allow the posterior lateral wall, the posterior region of the roof, and the posterior wall of the maxillary sinus to be cleared of pus, fungal debris, and polyps. As we have stressed, it is essential to remove as much of the disease burden as possible to allow for resolution of symptoms. Access to these areas has been aided by the recent introduction of 90- and 120-degree cutting blades. Alternatively, an inferior meatal approach may be used, but once again, access to the anterior half of the maxillary sinus is compromised. This is due to the two fulcrums that the microdebrider and instruments must pass to reach the sinus cavity (Fig. 12.18). Therefore, in many patients with extensive maxillary sinus disease, complete removal of all polyps and debris requires access through the anterior maxillary wall of the maxillary sinus. With this access the blade or instrument has only one fulcrum, and so a much greater range of motion within the sinus can be achieved (Fig. 12.19). One such method is the traditional Caldwell– Luc approach performed through the anterior wall of the maxillary sinus. This is, however, associated with significant morbidity such as facial numbness or paresthesia (9%), oroantral fistulas (1%), gingivolabial wound dehiscences (1.5%), and dacryocystitis (2.5%).7 Canine fossa puncture (CFP) was initially proposed as an alternative method of obtaining access to the maxillary antrum. Fig. 12.17 The following pictures of the left maxillary sinus were taken after a maxillary antrostomy has been performed and illustrate the grades of disease.(A) Grade 1: Slightly edematous mucosa and cobblestoning in the area of the sinus floor. (B) Grade 2: Edematous mucosa with small polyps, which are reversible with medical treatment, provided there is no significant eosinophilic mucus.(C) Grade 3: Extensive polyps and tenacious mucus completely filling the maxillary sinus, requiring a canine fossa trephination(CFT). A description of this standard technique is as follows:32 the lip of the patient is elevated and the canine tooth identified. The root of this tooth is traced superiorly with the finger until the canine fossa is palpated. A small volume of 2% lidocaine with 1:80,000 of adrenalin is infiltrated into this region. A small incision is made in the gingivobuccal sulcus above and slightly lateral to the apex of the canine tooth, and the soft tissue is dissected off the anterior face of the maxilla. A canine fossa trocar (Karl Storz, Tuttlingen, Germany) is placed in the fossa and directed posteriorly. Using a rotating forward motion, a round 4-mm opening is created, which allows insertion of a straight or a curved 4-mm microdebrider blade. When the bone is too thick, a couple of firm taps with the palm of the hand is usually sufficient to drive the trocar through the bone. However, occasionally tapping with a mallet is necessary. This sublabial mucosal incision is small enough to close spontaneously and is not sutured. After the tip of the trocar is felt to fully penetrate the sinus, it is withdrawn and the microdebrider is introduced into the puncture with its blade kept closed to prevent soft tissues from being aspirated in during this step. Once inside the sinus, the 70-degree telescope is introduced into the nasal cavity to look through the antrostomy. At this point, the gate of the blade is opened, which helps to remove most of the blood from within the sinus and allows visualization of the blade within the maxillary sinus (Fig. 12.20). This step is important to confirm the position of the microdebrider in the sinus, and not in the orbit or soft tissues. The blade can then be used to remove polyps under direct vision. Fig. 12.18 Axial section through the maxillary sinus demonstrating the microdebrider blade being passed through an inferior meatal antrostomy. Due to the anterior fulcrum at the nasal vestibule and the posterior fulcrum at the antrostomy, only the posteromedial region of the sinus can be effectively cleared. Fig. 12.19 Axial section through the maxillary sinus demonstrating the microdebrider blade being passed through a canine fossa puncture. As a result of the single fulcrum at the anterior face of the maxilla, the entire sinus can be accessed by the microdebrider. Fig. 12.20 Endoscopic view through a right maxillary antrostomy, using a 70-degree endoscope, illustrating the microdebrider blade which has been passed though the canine fossa trephination (CFT) site in the anterior face of the maxilla. The incidence of complications with the old CFP technique was 75%.32 In a review of 37 CFPs in 21 patients, the most common complaint was of cheek swelling in 38% of the sides, followed by facial pain (32%), facial numbness (30%), cheek pain (27%), dental numbness (27%), gingival complications (24%), and facial tingling (16%). Most of these (75.5%) resolved within the first month after surgery; however, 28% had persistent complications with facial tingling, numbness, or continued pain. These longer-term complications are thought to be a result of injury to branches of the infraorbital nerve. Thus, the anatomy of the nerve as it exits the infraorbital foramen and divides into the anterior superior alveolar nerve (ASAN) and middle superior alveolar nerve (MSAN) is of particular importance when performing this procedure. Cadaver research conducted in our department had determined that the safest entry point for the canine fossa trocar was the junction of the midpupillary line and a horizontal line running along the base of the pyriform aperture (Fig. 12.21).33 One of the shortcomings of the canine fossa puncture is that it is performed in a blind manner. Even though the soft tissues anterior to the maxilla are dissected off, the precise area through which the trocar is placed is not visualized, and the ASAN or the MSAN could thus be injured. Additionally, the use of the trocar may fracture the thin bone of the anterior maxillary wall around the puncture site. The edges of the trocar are meant to act as a drill, cutting the bone with a rotating motion and minimal pressure. If significant pressure is applied to the trocar, a fracture of the surrounding bone will often occur, enlarging the area of trauma and increasing the risk of nerve injury. And even if the trocar creates a sharp 4-mm puncture in the bone, the 4-mm debrider blade fits very snugly through this opening and manipulation of the blade within the sinus may itself cause fracture of the surrounding bone, with the potential of neurologic injury. Furthermore, devitalized bone fragments may act as a nidus of persistent inflammation and granulation within the maxillary sinus. To overcome all of these problems, a new technique, referred to as canine fossa trephination, was devised to improve the bony penetration through the anterior face of the maxillary sinus. Fig. 12.21 The landmarks for the canine fossa puncture/trephine are the intersection between a vertical line through the pupil and a horizontal line through the floor of the nose. Fig. 12.22 The canine fossa trephination kit (Medtronic ENT, Jacksonville, FL) consisting of an endoscope sheath (black arrow) with a protruding blade, which allows retraction of soft tissues during dissection on the anterior face of the maxilla; a reusable drill guide(white arrow), and 5-mm reusable drill bit that fits the microdebrider hand-piece. Canine fossa trephination (CFT) is now our procedure of choice for anterior approaches to the maxillary sinus (see Video 12.6). The essential difference between CFT and CFP is that a 5-mm hole is accurately drilled through the anterior maxillary face under direct visualization rather than using a trocar. To enable us to do this, new instrumentation has been developed to aid in the accurate placement of the drill hole. The canine fossa trephination kit (Fig. 12.22) consists of an endoscope sheath with a protruding blade, which allows retraction of soft tissues during dissection on the anterior face of the maxilla. In addition, the kit contains a reusable drill guide and 5-mm reusable drill bit that fits the microdebrider handpiece. The endoscope sheath is placed on a zero-degree scope, the lip is held up and gingivobuccal sulcus infiltrated with lidocaine and adrenalin. An angled 6-mm incision is made in the gingivobuccal sulcus using a 15-blade or Colorado diathermy needle. A suction Freer elevator is used to elevate the soft tissues off the anterior face of the maxilla in a subperiosteal plane. Once this is achieved, the extension on the endoscope sheath is used to hold away soft tissues allowing clear visualization of the subperiosteal plane on the anterior face of the maxilla. The dissection is then continued in a superior and lateral direction, to expose the area located at the intersection of the midpupillary line and a horizontal line running along the lower border of the nasal alae. It is not uncommon to visualize one of the branches of the anterior-superior alveolar nerve on the anterior face of the maxilla (Fig. 12.23). If a branch is seen, the dissection is carried a little further to avoid injury to the nerve (see Video 12.7). Fig. 12.23 A branch of the anterior-superior alveolar nerve is seen on the anterior face of the maxilla (black arrows); the dissection is therefore carried a little further to avoid injury to the nerve. The canine fossa drill guide (Medtronic ENT, Jacksonville, FL) is then placed on the anterior face of the maxilla at the junction of the two lines described above. The canine fossa drill (Medtronic ENT) is attached to the microdebrider hand-piece and irrigation is attached to the back of the drill guide, allowing irrigation of the burr during drilling. The burr is used at 12,000 rpm for best results. Note that the drill should be maneuvered so that it is perpendicular to the anterior face of the maxilla and not angled tangentially to the maxilla. A 5-mm diameter hole is drilled through the bone (Fig. 12.24), and a Frazier suction is used to remove any bone dust from the hole and surrounding soft tissues. The 4-mm microdebrider blade is then placed through the trephine into the maxillary sinus in the closed position, and a 70-degree endoscope is passed transnasally to the maxillary antrostomy. At this point, the gate of the blade is opened to remove the blood from within the sinus and to allow visualization of the blade within the maxillary sinus. This confirms the position of the microdebrider, and this step is important to avoid inadvertent injury to the orbit or soft tissues. The first step is to enlarge the maxillary antrostomy as this provides improved visualization into the sinus with the 70-degree scope. The blade is used to enlarge the maxillary sinus antrostomy, removing any residual uncinate process and posterior fontanelle up to the posterior wall of the maxillary sinus. This affords the widest possible view through the antrostomy, and the surgeon can then remove polyps and thick mucous from the sinus under direct vision. Angled suctions are used for the lateral recesses and anterior face of the maxillary sinus (Fig. 12.25). The endoscope can also be placed through the trephine into the sinus to inspect and ensure the complete removal of disease material. It is important to note that only polypoid tissue and mucin are removed, and the denuding of bone is avoided. This helps to ensure a speedy reepithelialization and reciliation in the postoperative period. Fig. 12.24 A5-mm hole is drilled into the anterior face of the maxilla. Fig. 12.25 View through the middle meatal antrostomy using a 70-degree endoscope, showing an angled suction passed via the trephination in the anterior face of the maxilla and used to clean the inferior, lateral, and retrolacrimal recesses of the maxillary sinus. As for the middle portion of the uncinate process, care is taken not to microdebride tissues based superiorly in the area of the lamina papyracea because of the risk of orbital penetration. If this needs to be performed due to a significant amount of polypoid tissue narrowing the antrostomy, the scrub nurse should be asked to gently push on the eye while the surgeon inspects the lamina for transmitted movement, indicating a bony dehiscence (see Video 12.1). If movement is seen, it is recommended not to use powered instrumentation for this area, but rather to clear the polyps using through-biting Blakesley forceps. To assess whether the new technique reduced the incidence and severity of complications, a clinical study of 63 patients was undertaken, including 36 bilateral procedures giving a total number of 99 anatomically directed canine fossa punctures (aCFP; without the trephination kit) and trephines (CFT; with trephination kit).34 The overall frequency of adverse events was significantly reduced to 45%, compared with the previously reported 75% with the traditional blind technique. The number of patients complaining of persisting adverse effects was reduced from 28% to 5%. The 67 CFT procedures had a significantly lower frequency of adverse events (40%) than the 32 aCFP procedures (53%). This again emphasizes the need to visualize the anterior face of the maxilla before placing the trephine and also emphasizes the increased risk of nerve injury if a trocar rather than trephination set is used. We have focused on the use of CFT and its applications in revision maxillary sinus surgery. However, it must be recognized that the principles promoted in revision surgery are often applicable in primary surgery, and CFT is a very useful tool in the management of many disease processes within the maxillary sinus. In patients with extensive polyposis and/or eosinophilic mucin, mucopyoceles, antrochoanal polyps, foreign bodies, and other situations where access to parts of the maxillary sinus not attainable through a maxillary antrum is required, then CFT is the approach of choice. Patients who have undergone either the canine fossa puncture or trephination usually do not require suturing of their gingivobuccal incisions. They are advised to rinse their mouths with saline after meals during the first few postoperative days, until the incisions have sealed. Nasal saline irrigation is begun on the day after surgery, and all patients receive 5 to 10 days of broad-spectrum antibiotics. The first postoperative visit and debridement is performed at 2 weeks. Even if initial management of the maxillary sinus is optimal, there are several potential reasons for persistent disease within the sinus requiring further surgical intervention. The causes of persistent maxillary sinus symptoms after endoscopic sinus surgery can be categorized into recirculation, infection draining into the maxillary sinus from elsewhere, retained foreign material, failure of mucociliary transport, scarring, and local osteitis. The goal of the clinical evaluation and diagnostic imaging studies is to determine the underlying factors contributing to sinus disease. Revision maxillary sinus surgery seeks to improve medical management by reducing disease load and improving the maxillary sinus drainage pathway, providing access for topical medications. This is done by removing recurrent nasal polyps or hypertrophic sinonasal mucosa from the maxillary sinus disease and ensuring an adequate maxillary antrostomy. To achieve this, depending on the technical factors identified, revision uncinectomy, scar division, middle turbinate medialization or enlarging the antrum posteriorly into the fontanelle, may be performed. The canine fossa trephination technique is a highly effective way to reduce disease load in the severely diseased maxillary sinus, whether in revision surgery or in the primary setting. Recent modifications to this technique have been successful in reducing the rate of associated complications. • The goal of assessment of the patient with symptoms suggesting persistent or recurrent sinus disease is to identify the presence of technical, mucosal, and systemic factors contributing to poor outcome by using the appropriate tests. • Know that medical management will be required after surgery. Protocols should be in place to manage recurrent or recalcitrant bacterial or fungal colonization of the maxillary sinus. • The goal of surgery is to provide a well-ventilated, epithelialized, and disease-free maxillary sinus. It should be noted that in some situations, medical management may be required to further treat those patients with severe mucosal disease. • Causes of persistent maxillary sinus symptoms after ESS can be clustered into six large categories: recirculation, infection draining into the maxillary sinus from elsewhere, retained foreign material, failure of mucociliary transport, scar formation, and local osteitis. • Indications for revision endoscopic sinus surgery can be broadly categorized as follows: (1) incomplete previous surgery, (2) complications of previous surgery, (3) recurrent or persistent sinus disease, and(4) histologic evidence of neoplasia. These criteria are not absolute and the decision to reoperate is most often based on clinician judgment and experience. • Surgery is aimed at either improving the natural maxillary sinus drainage pathway (i.e., uncinectomy, scar division, middle turbinate medialization, or changes to the antrum) or through removal of persistent and significant maxillary sinus disease via the canine fossa trephine approach.
 Causes of Failed Maxillary Sinus Surgery
Causes of Failed Maxillary Sinus Surgery
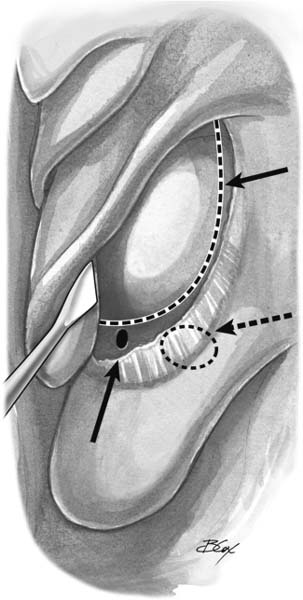
Recirculation
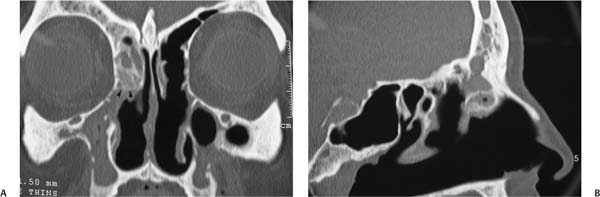
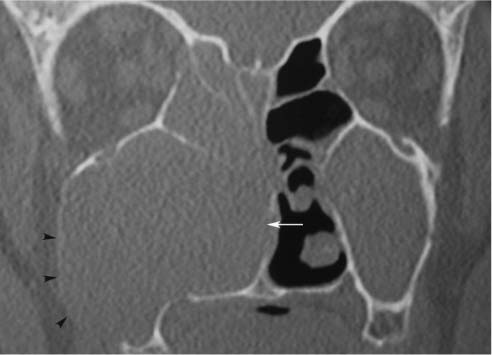
Infection Draining into the Maxillary Sinus from Elsewhere
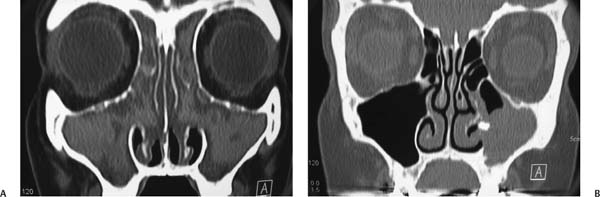
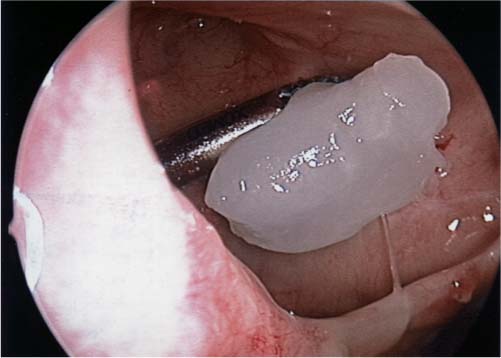
Retained Disease or Foreign Material
Failure of Mucociliary Transport
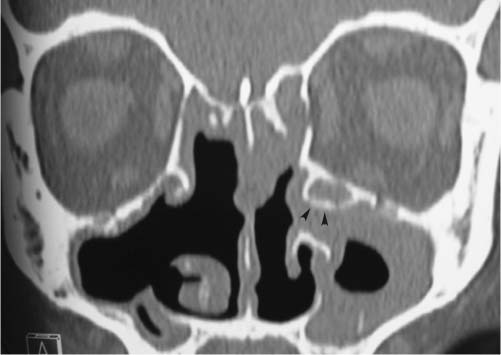
Scar Formation
Osteitis
Biofilms
Other Causes
 Preoperative Management
Preoperative Management
Clinical Assessment
Imaging Studies
The Role of Image-guided Surgery
Medical Management
 Surgery
Surgery
Indications for Revision Surgery
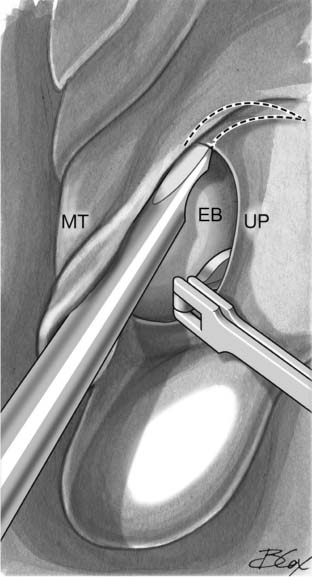
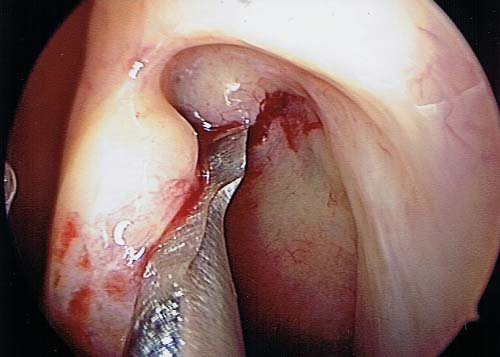
Revision Uncinectomy and Maxillary Antrostomy
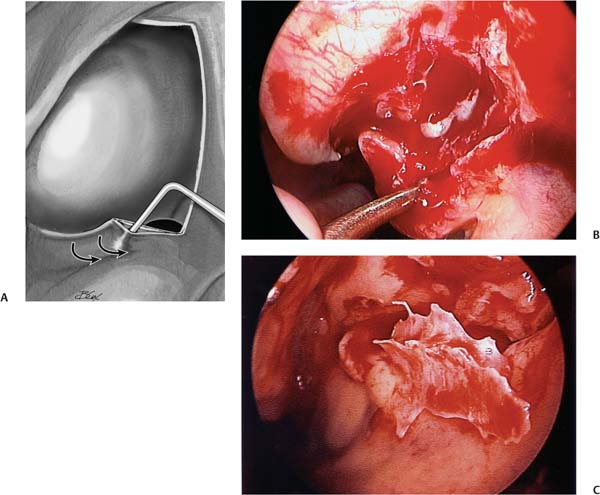
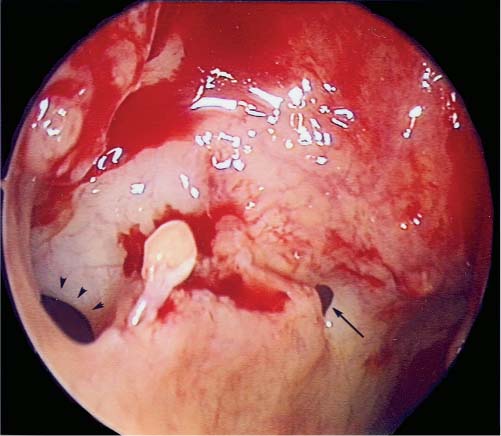
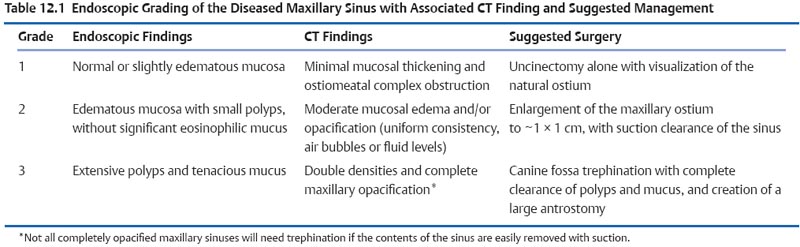
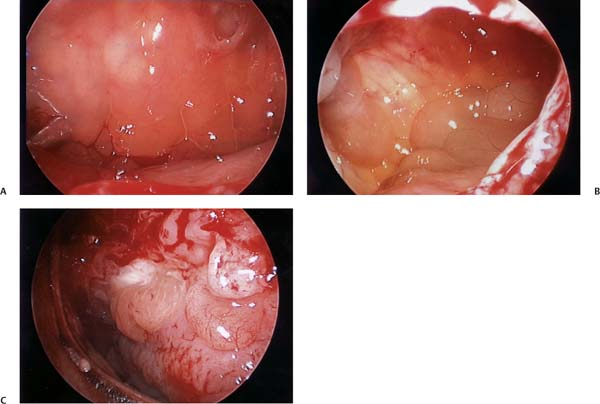
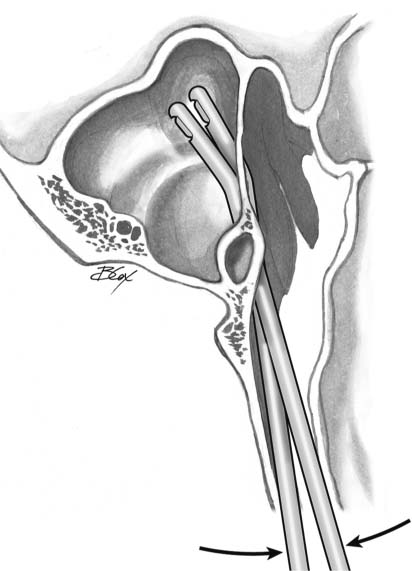
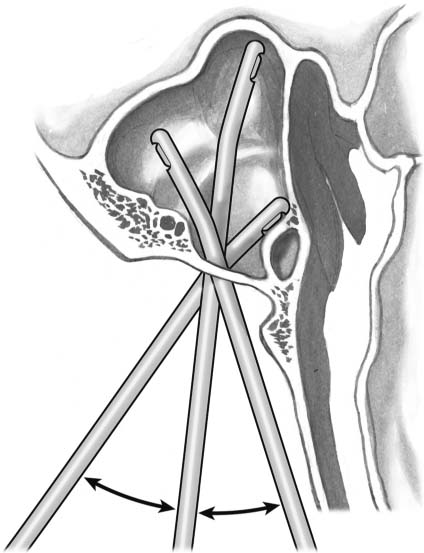
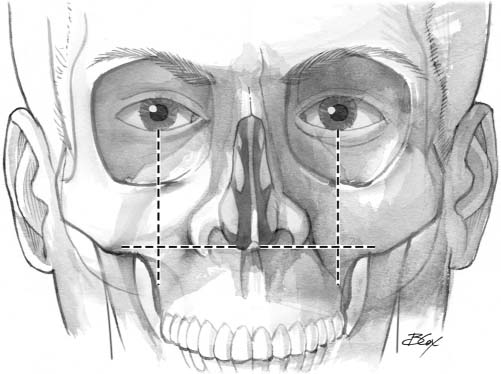
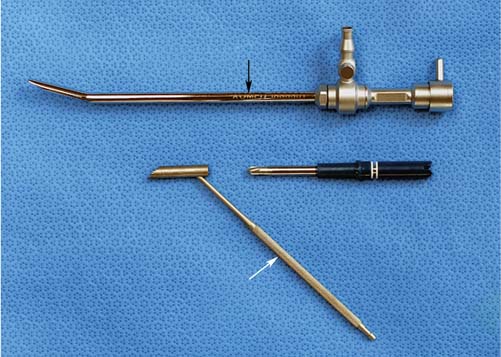
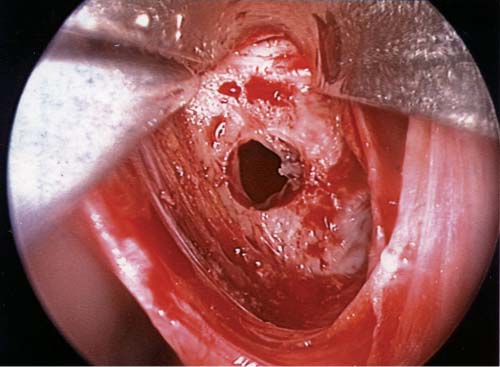
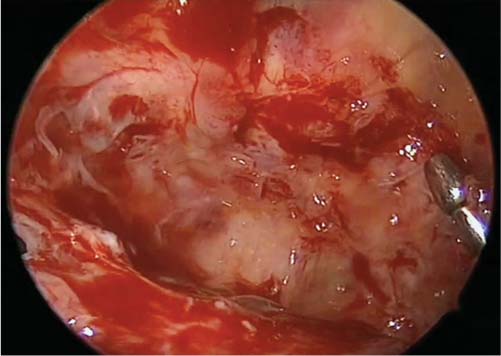
Anterior Approaches to the Maxillary Sinus including Canine Fossa Trephination
 Postoperative Care
Postoperative Care
 Conclusion
Conclusion
Revision Maxillary Sinus Surgery including Canine Fossa Trephination
Pearls
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree