Fig. 18.1
Retinoblastoma with regional extraocular spread
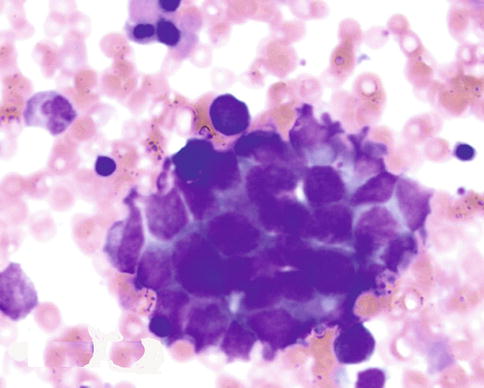
Fig. 18.2
The bone marrow aspiration smear positive for the retinoblastoma cells
18.3 Diagnostic Evaluation
Patients suspected to have extraocular retinoblastoma need to have extensive evaluation investigating the sites described above (Table 18.1). In anticipation of aggressive chemotherapy, baseline laboratory work should be performed (Table 18.2).
Table 18.1
Systemic workup for suspected metastatic disease
Organ/system | Tests |
|---|---|
Central nervous system | Brain and orbit MRI with and without contrast |
Lumbar puncture for CSF cytology | |
Spine MRI with and without contrast (if CNS disease is present or appropriate, focal neurological signs are present) | |
Visceral organs | Abdominal CT with IV contrast |
Bone and bone marrow | Bone scan |
Bone marrow aspirate and biopsy |
Table 18.2
Laboratory workup for suspected metastatic disease
Complete blood count with differential |
Liver function studies |
Estimate of glomerular filtration rate via either timed urine collection for creatinine clearance or nuclear medicine renal function study |
Audiogram |
LDH determination may also be useful to provide an estimate of the total body tumor burden |
18.4 Differential Diagnosis
While theoretically a broad differential diagnosis exists for the findings associated with extraocular retinoblastoma, in the appropriate context (patient with a history of intraocular retinoblastoma), it is usually fairly obvious whether or not a patient has extraocular retinoblastoma. However, bone and bone marrow disease should be differentiated from secondary neoplasms, since secondary leukemia and other small round blue cell tumors may occur in patients with heritable retinoblastoma and differential diagnosis may be difficult. Occasionally orbital masses can develop and be suspected to represent orbital retinoblastoma, but instead may be due to granulomas or other causes [1].
18.5 Treatment and Prognosis
18.5.1 Regional Extraocular (Orbital) Retinoblastoma
In this section we will summarize data indicating that patients with regional extraocular (orbital) retinoblastoma can be cured with an appropriately intensive treatment that includes systemic chemotherapy and external beam radiation therapy.
18.5.1.1 Isolated Orbital Retinoblastoma
Patients with isolated orbital retinoblastoma had fared poorly when treated with surgery +/− radiation therapy [2], but their prognosis improved considerably when conventional chemotherapy was added to the treatment regimen, with 1-year event-free survival of 40 % following treatment with a variety of chemotherapy agents [3, 4]. The management of orbital retinoblastoma is discussed in detail elsewhere (Chap. 17).
18.5.1.2 Regional Extraocular Retinoblastoma
More recent publications confirm that patients with regional extraocular disease (orbital and/or preauricular disease, optic nerve margin positivity) may be cured with conventional chemotherapy and external beam radiation therapy. Investigators in Argentina treated 15 patients with orbital or preauricular nodal disease on 2 consecutive protocols. Chemotherapy included vincristine, doxorubicin, and cyclophosphamide (local protocol 87) or vincristine, idarubicin, cyclophosphamide, carboplatin, and etoposide (local protocol 94). The external beam radiation therapy dose was 4,500 cGy, administered up to the chiasm for patients with orbital disease and to the involved nodes in patients with preauricular adenopathy. The group achieved a 5-year event-free survival of 84 % [5]. The Argentine and New York groups also reported the results of 12 patients with optic nerve margin positivity treated with the chemotherapy regimens above and orbital radiation therapy (4,000–4,500 cGy). All 12 were event-free survivors [6].
Similarly, investigators in Brazil reported the results of 2 consecutive protocols. Chemotherapy included vincristine, doxorubicin, cyclophosphamide, cisplatin, and teniposide (1987–1991) or ifosfamide, etoposide, cisplatin, and teniposide (1992–2000). The external beam radiation therapy dose was 4,000–5,000 cGy to the orbit. Triple intrathecal therapy was also administered. Their therapy was successful in 20 of 32 patients (63 %) with orbital disease and 22 of 29 (76 %) with optic nerve margin positivity [7].
18.5.2 Distant Metastatic Retinoblastoma Without CNS Involvement (Stage 4a)
In this section we will summarize data indicating that patients with distant metastatic retinoblastoma have a poor prognosis when treated with conventional therapy but may be cured when therapy is intensified to include high-dose chemotherapy with autologous stem cell rescue (ASCR) (Fig. 18.2). Most of the experience involves patients with stage 4a metastatic disease that does not involve the central nervous system [8].
18.5.2.1 Conventional Dose Chemotherapy Plus Radiation Therapy
Older publications from several centers reported the results of trials utilizing conventional dose chemotherapy and radiation therapy for metastatic extraocular disease, most using vincristine, doxorubicin, cyclophosphamide, cisplatin, and etoposide. Despite occasional reports of long-term event-free survival [9, 10], the bulk of the evidence suggested that the prognosis remained grim with such an approach [11–13]. More recent publications confirm the dismal prognosis. The Argentine investigators (using the regimens discussed above) noted that all 26 patients with distant metastases died [5]. Similarly, the Brazilian investigators noted that treatment with their regimens (discussed above) led to survival of only 1 of 14 patients (7 %) with distant metastases [7].
18.5.2.2 Case Reports of High-Dose Chemotherapy with ASCR
Individual case reports had suggested that the use of high-dose chemotherapy with ASCR might be beneficial for patients with metastatic retinoblastoma [14, 15], and subsequently Institut Curie investigators reported the results of 25 patients with high-risk retinoblastoma treated with high-dose carboplatin, etoposide, and cyclophosphamide followed by ASCR [16]. Five of eight patients with stage 4a disease were event-free survivors 11–70 months after high-dose chemotherapy. Three had central nervous system relapses and died of disease 10–20 months after high-dose chemotherapy. Three other patients had disease that progressed during induction with conventional induction chemotherapy and never received high-dose chemotherapy. In total, then, five of 11 patients (45 %) with stage 4a metastatic disease were event-free survivors.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


