Chapter 50 Retinal detachment in childhood
Rhegmatogenous retinal detachment associated with trauma
Traumatic retinal detachment is seen mostly in older children, usually caused by blunt trauma where retinal tears may be found in 2–5%.1 Penetrating injuries and retained intraocular foreign bodies are less frequent causes2,3 but are frequently associated with severe PVR.
Blunt ocular trauma
Retinal dialysis
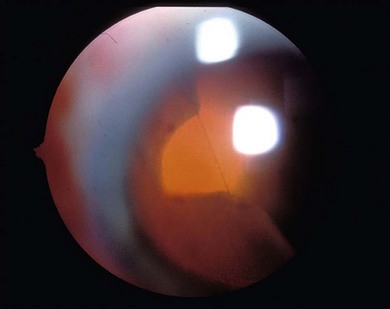
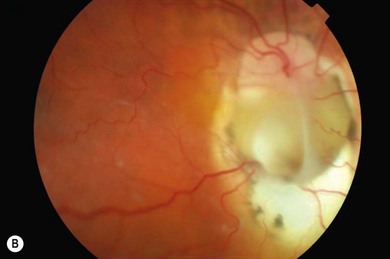
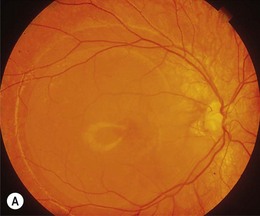
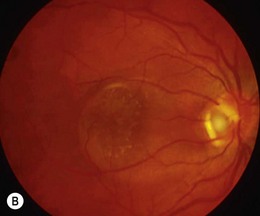
Retinal detachment due to blunt trauma is mostly caused by a disinsertion at the ora serrata in older children. Sudden anteroposterior compression of the globe with a violent coronal expansion leads to retinal avulsion (Fig. 50.1A) characterized by a festoon of non-pigmented pars plana epithelium in the vitreous cavity. This is the hallmark of traumatic retinal dialysis. There may be signs of related orbital injury (Fig. 50.2) or, more freqently, subtle signs of collateral trauma to the iris, lens, or drainage angle. Superior quadrant involvement is more frequent than the lower temporal quadrant involvement seen in non-traumatic dialysis (Fig. 50.1B and see below). Although the disinsertion may exceed 90° and resemble a giant retinal tear, the vitreous characteristically remains attached to the posterior flap so that independent mobility is not a feature. Dialyses, therefore, respond very well to conventional scleral buckling techniques – an accurately positioned 3 mm sponge being all that is required. Further distinguishing features are the absence of radial extensions, which frequently occur at the apices of true giant retinal tears (GRTs) (Fig. 50.3) and the normal compact healthy vitreous architecture. GRTs in childhood are typically associated with abnormal vitreous and inherited vitreoretinopathies (see below). Subretinal fluid recruitment in dialyses is typically slow, so that unless the ora serrata is routinely inspected after blunt trauma, the diagnosis may be delayed by weeks or months until macular involvement causes poor acuity.3
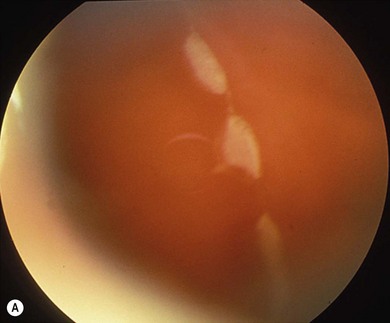
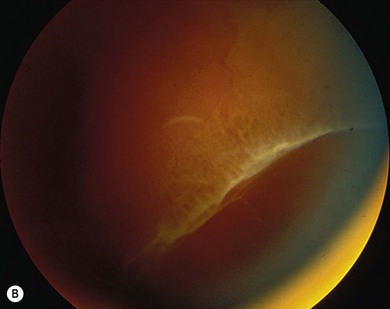
Fig. 50.1 Retinal dialysis. (A) Traumatic 180° “bucket handle” avulsion non-pigmented pars planar epithelium from patient in Figure 50.2. (B) Non-traumatic retinal dialysis. Note characteristic associated cystic oral frill and transdialysis tissue bridges.

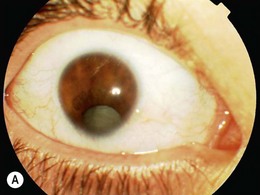
Fig. 50.2 Blunt injury with associated traumatic retinal dialysis. Vision logMAR 0.0 (6/6, 20/20, 1.0) unaided. Note enophthalmos. Fundus findings illustrated in Figure 50.1A.
Ragged impact necrosis breaks account for about one-fifth of the retinal breaks in blunt trauma.3 Retinal vessel and retinal pigment epithelial disruption may be confirmed on fundus fluorescein angiography and retinal detachment usually presents within 6 weeks.3 These breaks are often large, postequatorial, and irregular, making closure by external buckling problematic so that an internal approach is more usually required.
Penetrating ocular trauma
Penetrating injury is an uncommon cause of retinal detachment in childhood and may rarely follow inadvertent perforation of the globe at strabismus surgery. More common causes include accidental sharp penetrating injuries. Intraocular foreign bodies are rarely seen in very young children, although penetrating injuries from air-gun pellets may be seen in older children and adolescents, usually with a poor prognosis because of the associated damage and aggressive PVR. Retinal perforation or incarceration from penetrating trauma rarely causes acute rhegmatogenous retinal detachment. The corneoscleral wound provides access for extrinsic fibroblasts so that the more common sequel is late tractional and rhegmatogenous retinal detachment.5 Vitrectomy and internal tamponade with or without retinal relieving incisions may be required.
Non-traumatic retinal dialysis
Non-traumatic retinal dialysis accounts for approximately 10% of all juvenile retinal detachment2,4 and in 97% affects the inferotemporal quadrant (Fig. 50.1B). Examination of the entire retinal periphery may reveal two or more separate dialyses in the same eye. There is a 2 : 3 male propensity and the majority are hypermetropic or emmetropic.6,7 Detachments associated with dialyses progress slowly and present either as an incidental finding or when the macula becomes detached. They can be managed routinely with conventional buckling. The use of a small (typically 3 mm) circumferential sponge reduces postoperative motility problems. Although the anatomic success rate of surgery is high, visual recovery may remain poor if there has been chronic macular involvement. Familial dialyses are rare, but consideration should be given to sibling examination because (1) the patients are asymptomatic and (2) visual recovery once macular involvement has occurred may be poor. Examination of the fellow eye under anesthesia is important as retinal dialysis may be bilateral and abnormalities of the ora serrata, in the form of a “frill” or flat dialysis, are found in the fellow eye in up to 30%. Prophylactic retinopexy can be applied to avert detachment with potential macular involvement requiring formal repair.
Rhegmatogenous retinal detachment associated with developmental abnormality
Ocular coloboma
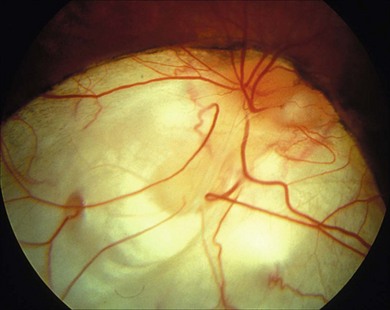
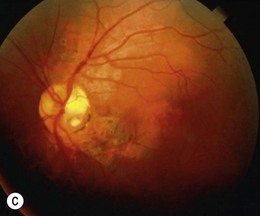
Eyes with colobomas are at increased risk of detachment and account for approximately 0.5% of pediatric retinal detachments8,9 forming part of the spectrum of wider systemic developmental abnormality (Fig. 50.4). GRTs are seen with lens colobomas10 and rhegmatogenous detachment may also develop in eyes with choroidal coloboma, when small retinal breaks may be found in the hypoplastic retina overlying the coloboma. Assessment of vision can be difficult and the diagnosis of detachment can be further impaired by restricted pupil dilation, nystagmus, microphthalmos, and cataract (Fig. 50.5). The intercalary membrane stretched across the coloboma cavity can simulate a retinal detachment on ultrasound examination. The clinician should be alert to this and assess the retinal mobility on dynamic examination before surgery. The intercalary membrane consists of hypoplastic inner retina with reversal and duplication of outer neuroblastic layers at the coloboma margin.11 This marginal duplication has been proposed as a “locus minoris resistentiae” providing adhesion. Both retinal pigment epithelium and Müller cells are vestigial or absent within the coloboma; thus, effective retinopexy may be impossible unless applied outside the margin.
Where retinal breaks occur away from the coloboma, they may be managed by conventional buckling provided the sclera is of sufficient quality and the break can be adequately closed. More usually, the retinal break lies within the coloboma so that identification and closure with retinopexy may be impossible without an internal approach. Retinal breaks over a coloboma are often small and multiple. Their localization can be very difficult preoperatively against the pale scleral background (Fig. 50.6), but may be confirmed peroperatively by the visualization of proteinaceous schlieren (optical variations and inhomogeneities in the transparency of the subretinal fluid) during internal drainage. Laser may be applied around the border of the colobomatous area and where this includes the papillomacular bundle it may be applied prior to retinal reattachment to minimize thermal damage to the nerve fiber layer. Maintenance of tamponade throughout the retinopexy can be compromised by the abnormal configuration of the colobomatous globe and recurrent detachment may occur in up to 30%,12 necessitating permanent internal tamponade.
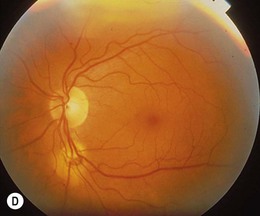
Optic disk pits and macular detachment
The association of serous macular detachment and optic disk pits and coloboma is well recognized and similar findings with the morning glory disk abnormality suggest that these conditions are variations of the same abnormality (Fig. 50.7). The vitreous is characteristically attached. It has been suggested that up to 45% of optic disk pits may be complicated by serous retinal detachment.13,14 Although cases of spontaneous resolution have been reported, the visual prognosis is poor if the detachment persists beyond 6 months.14
Although natural history studies have shown eventual spontaneous reattachment in 25% of cases14 and photocoagulation alone has mixed success, the combination of argon laser photocoagulation with internal tamponade, either with or without vitrectomy, may offer a greater chance of successful retinal reattachment, albeit at greater risk of operative morbidity.
Rhegmatogenous retinal detachment associated with inherited vitreoretinopathies
Inherited vitreoretinopathies are the basis for the majority of rhegmatogenous retinal detachments in childhood and are classified according to Meredith and Snead15 as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree