CHAPTER 172 Rehabilitation of Facial Paralysis
The facial nerve, once damaged, rarely attains full recovery of function. Given the challenges to the patient, counsultations regarding facial nerve paralysis require a clinician’s fullest thought and compassion. A realistic approach yields the rewards of patient compliance, understanding, satisfaction, and acceptance of reality. A recent review of all state and federal civil trials alleging malpractice and facial nerve paralysis demonstrates the importance of careful explanation and documentation, as well as the importance of good patient rapport and bedside manner in preventing lawsuits.1
Patient Assessment
An outline of assessment of facial nerve paralysis is presented in Box 172-1.
Assessment of the Deformity
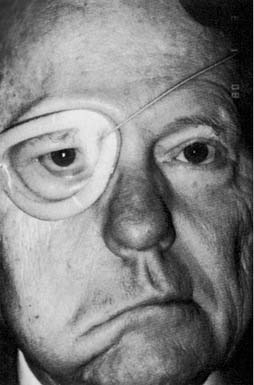
Physical examination includes complete head and neck examination with attention to cranial nerve function and the presence of functional masseter and temporalis muscles. The degree of facial nerve function is recorded using the House-Brackmann Facial Grading System2 (Table 172-1). A number of facial nerve grading scales have been developed, but the House-Brackmann scale was adopted by the Facial Nerve Disorders Committee of the American Academy of Otolaryngology–Head and Neck Surgery in 1985 because of its reproducibility and ease of use.2 This scale is useful for evaluation of overall function, but it is insufficient for precise assessment of defects affecting one or more branches of the facial nerve, and it does not allow precise measurement of effectiveness of treatments isolated to one region of the face. Therefore, the examination should assess deformity of the upper, middle, and lower thirds of the face independently. This approach allows more precise characterization of defects, aids the decision-making process for rehabilitation, and allows more precise assessment of treatment results. Facial tone also is noted, as is the presence of any reinnervation. Thorough assessment of the eye also is performed. Visual acuity, corneal integrity, eyelid closure, tearing, Bell’s phenomenon, lagophthalmos, lower lid laxity, position of the lacrimal puncta, and eyebrow position are noted. Nasal examination focuses on the position of the ala and nasal septum and the presence or absence of nasal obstruction. Oral competence and height and position of the lower lip are carefully reviewed. In long-term paralysis (of more than 1 year’s duration), electromyography (EMG) of the facial muscles is performed before reinnervation procedures. Occasionally, muscle biopsy provides additional information about the presence of viable muscle for innervation. If nerve fibrosis is suspected, nerve biopsy occasionally is indicated.
Table 172-1 House-Brackmann Grading System
| Grade | Description | Characteristics |
|---|---|---|
| I | Normal | Normal facial function in all areas |
| II | Slight | |
| III | Moderate | Appearance: obvious but not disfiguring weakness between the two sides; noticeable but not severe synkinesis, contracture, and/or hemifacial spasm |
| IV | Moderately severe dysfunction | |
| V | Severe | |
| VI | Total | No facial function |
From House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146.
Another important component of the assessment is evaluation of the patient’s smile pattern. The smile is created by the muscles of the lips, and smile patterns can be classified into one of three types.3 The “Mona Lisa” smile is the most common smile pattern (67%). It is dominated by action of the zygomaticus major muscle: The corners of the mouth move laterally and superiorly, with subtle elevation of the upper lip. The canine smile (31%) is dominated by levator labii superioris action, appearing as vertical elevation of the upper lip, followed by lateral elevation of the corner of the mouth. The least common smile is the full denture smile (2%), or “toothy smile,” produced by simultaneous contraction of the elevators and depressors of the lips and angles of the mouth. Knowledge of facial muscle anatomy and the smile pattern exhibited by the patient is important in considering rehabilitation techniques other than nerve grafting to recreate a balanced facial appearance at rest and the simulation of a symmetric smile.
Considerations in Facial Nerve Rehabilitation
Generally, however, the order of preference for rehabilitation procedures is as follows:
Time since Transection
A chronic, long-standing paralysis with complete muscle degeneration poses several problems with regard to eventual reinnervation surgery. The facial muscles may undergo denervation atrophy. Severe atrophy renders the reasonably normal muscles incapable of reinnervation and contraction. Such severe atrophy may occur after 18 months of complete denervation, although in some clinical situations, muscles have been known to persist inexplicably for many years without incurring such atrophy.4 EMG is the most helpful method for assessing facial muscle atrophy and is therefore a preoperative prerequisite for all reanimation candidates if the paralysis is of more than 12 months’ duration. The presence of nascent, polyphasic, or normal voluntary action potentials in a patient with facial paralysis indicates the occurrence of reinnervation. If more than 12 months have passed since the facial nerve injury, the situation can be assumed to be stable, and an attempt at surgical reanimation may be warranted. Within the first 12 months, however, the presence of potentials may mean that reinnervation is occurring and that facial movements may return in the next few months. Reanimation surgery should therefore be postponed. Fibrillation or denervation potentials mean that the EMG electrode is positioned in denervated muscle. This is an optimal situation for cable nerve grafting or, when no viable proximal facial nerve is available, for hypoglossal-facial anastomosis.
Status of the Proximal and Distal Facial Nerve
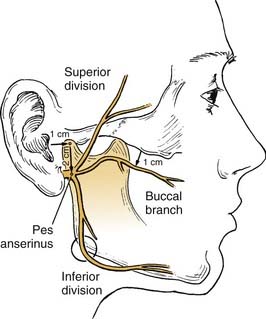
The facial nerve distal to the injury site serves as a conduit for neural regeneration to the facial muscles after neurorrhaphy, grafting, or hypoglossal-facial anastomosis. With acute injuries (incurred less than 72 hours previous), the electrical stimulator may be used to identify the distal nerve and the muscular innervation of distal branches. After this “golden period,” however, the surgeon must rely on visual identification of the divisions and branches of the distal nerve, because the capability of being stimulated electrically generally is lost after approximately 72 hours. For this reason, transected nerve branches in trauma or tumor cases should be tagged for identification by placing a small colored suture around or adjacent to each nerve branch. Any anatomic or surgical landmarks should be precisely dictated in the operative note. If no suture markers are available, and the golden period has elapsed, careful surgical searching (preferably with use of loupes or an operating microscope) may reveal each of the divisions or branches of the facial nerve. A topographic map is essential in guiding the dissection. A review by Bernstein and Nelson5 describes the variability with which these branches are placed. The following landmarks are helpful (Fig. 172-1).
(From House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146.)
As an example of selective routing, when a parotid tumor operation results in excision of the pes anserinus and the proximal facial branches, a branched nerve graft may be placed to reinnervate the zygomatic and the buccal branches, excluding unimportant branches. Fisch6 advises clipping branches of cervical branches in order to route innervation to the more important portions of the face. Data confirming the efficacy of this technique, however, are very limited.
If no nerve branches are found, and EMG shows that denervated facial muscles are present, the nerve graft may be sutured directly to the muscles targeted for reinnervation (muscular neurotization). In these instances, the most important muscles are those of the midface (zygomaticus major and minor, levator labii superioris) and orbicularis oculi muscles. Reinnervation will not be as complete as in routine nerve grafting because the regenerating axons must form new connections to the old motor endplates, or they must create their own.7
Viability of Facial Muscles
Four types of EMG responses are observed8:
Status of Donor Nerves
The hypoglossal nerve is the most frequently used nerve source for transfer. Reflex and physiologic similarities between the hypoglossal and facial nerves have been described.9 The integrity of the hypoglossal nerve must be determined before it is transferred for reinnervation. Irradiation of the brainstem, lesions of the skull base and hypoglossal canal, and surgical procedures of the upper neck may affect the integrity and function of this nerve.
The cross-face nerve graft procedure (faciofacial anastomosis) initially was thought to be the most appropriate and ingenious facial reanimation procedure.10,11 The procedure is unique in that it borrows appropriate neural input from the contralateral normal side and routes it to the paralyzed side. Such a procedure requires a fully intact (contralateral) facial nerve.
Age
The proximal neuron’s ability to regenerate declines with time because of denervation and aging-related changes. The etiologic mechanism probably involves diminishing regenerative vitality of the perikaryon (cell body), although peripheral scarring may play a role. The clinical implication is that facial reanimation surgery should always be performed as soon as possible, provided that the operative procedure does not interfere with or injure existing innervation or ongoing reinnervation.12
Prior Radiotherapy
Radiotherapy, a necessary component of treatment for certain salivary gland malignancies, appears to have a deleterious effect on reinnervation through facial nerve grafts. McCabe13 demonstrated satisfactory muscle reinnervation from grafting despite irradiation in animals. These investigators subsequently have documented return of facial function in nine patients who received post-grafting radiotherapy. McGuirt and McCabe13 and Conley and Miehlke14 have published reports indicating that facial nerve grafts function well even though irradiated, and that nerves are among the most radioresistant tissues of the human body. Pillsbury and Fisch15 found that radiotherapy reduced the average outcome from 75% to 25% of nerve function recovery in a review of 42 grafted patients. Irradiation probably affects the neovascularization of the nerve graft by decreasing vascularity of the tissue bed and probably injures the proximal and distal segments of the nerve as well. The most radiosensitive portion of the nerve—the pontine nucleus—should be assessed to determine whether it was present in the field of irradiation.
Congenital Paralysis
In a series of 95 infants with neonatal paralysis, Smith and associates8 found 74 of the cases to be secondary to intrauterine injury or birth trauma, whereas 21 were thought to be congenital. These infants should be studied with nerve excitability and EMG testing early in life to ascertain the status of nerves and muscles. Most patients with injury-related neonatal paralysis recover rapidly, whereas the paralysis associated with other congenital anomalies (such as Möbius syndrome) is permanent. Nerve exploration or transfer generally is futile in the latter cases.
Early Care of Facial Nerve Injury
Eye Protection: Evaluation and Treatment of Eyelid Paralysis
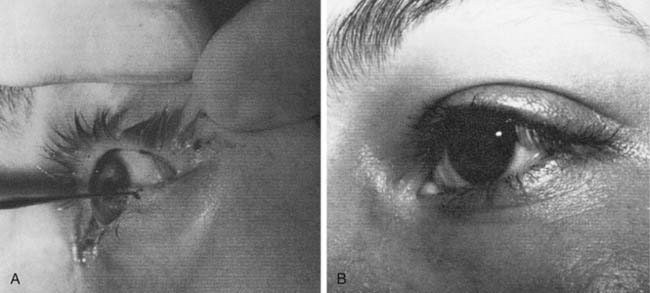
Lacriserts, contact lenses, and occlusive bubbles commonly are used, although patient compliance may be problematic16 (Fig. 172-2). The eyelids frequently are patched or taped, but if incorrectly used, these methods may result in corneal injuries. Tape should not be placed vertically across the eyelashes, but applied horizontally above the eyelashes on the upper eyelid, or supporting the lateral canthal portions of the lower eyelid.17 When an eye patch is used, care must be taken to ensure that the eye cannot open, because this would allow contact between the patch and the cornea.
Procedures to Treat Paralysis of the Lower Lid (Ectropion)
Tarsorrhaphy
For longer-lasting protection, the lid adhesion tarsorrhaphy is preferred. The lid margin (gray line) of each lid is denuded 4 to 6 mm from the lateral canthus, and a similar suture technique is used to approximate the denuded mucocutaneous junctions of upper and lower lids (Fig. 172-3). Like the temporary lateral tarsorrhaphy, this procedure can be reversed if function returns. The cosmetic deformity of tarsorrhaphy and the availability of improved, alternative techniques to rehabilitate the eyelids have reduced the use of tarsorrhaphies.
Wedge Resection and Canthoplasty for Paralytic Ectropion
The tarsal strip procedure described by Anderson and Gordy18 modifies the previously described technique by denuding the conjunctiva over the lateral tendon and separating the posterior lamella and the tendon from the anterior lamella. The isolated tarsal strip is then suspended to the lateral orbital rim. In cases of severe ectropion, the lower lid punctum may be everted and displaced laterally after lateral canthoplasty. In these instances, a medial canthoplasty is used to restore the physiologic relationship of the punctum to the globe.19,20 The lower lid also may be augmented with auricular cartilage to address inadequate support of the medial tarsal plate in cases not amenable to lateral tendon suspension alone.21
Procedures to Treat Paralysis of the Upper Lid (Lagophthalmos)
Weights, Springs, and Slings for Lagophthalmos
Under local anesthesia, an incision is made extending equally between the medial and middle thirds of the supratarsal crease, and the skin is elevated to the superior border of the tarsus. A pocket is formed immediately superficial to the tarsus to accommodate the dimensions of the weight. The weight is placed so that its inferior border is parallel to and just above the eyelash line. It is important to create a pocket directly on the tarsal plate, with care taken to preserve a thin cuff of tissue at the lid margin to prevent inferior extrusion of the implant. The implant is secured with clear nylon sutures superior and inferior to the tarsal plate, the orbicularis-levator complex is reapproximated, and the skin is closed.16
Palpebral springs and silicone (Silastic) slings as described by Morel-Fatio and Lalardrie22 and Arion,23 respectively, also have been used for lagopththalmos. Silastic slings are used less frequently and are complicated by lateral ectropion.24 Both types of implants share the disadvantage of extrusion, and they are more difficult to place than eyelid weights. Currently, titanium chain link implants are being used with greater frequency and with excellent results. These implants may be camouflaged to obtain a better cosmetic result, because they conform to the shape of the eyelid. Additionally, the titanium implants have been shown to result in less corneal astigmatism or cornea-altering effect on the globe itself than that typical with gold weights.25
Facial Nerve Grafting
Facial nerve grafting for acute causes such as parotid malignancy requires the surgeon to customarily identify the distal facial nerve trunk divisions or branches for the distal anastomosis. Nerve restitution should be performed at this time unless extenuating circumstances (e.g., anesthetic complications, intraoperative emergencies) rule out immediate grafting.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree